Dr-Kumar
advertisement

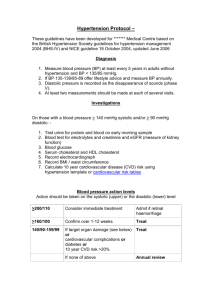
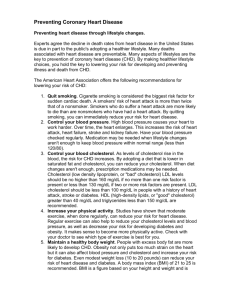
HEART DISEASE WHY WE GET THEM AND WHAT TO DO ABOUT THEM SOMNATH KUMAR CONSULTANT CARDIOLOGIST Department of Cardiology LANCASHIRE TEACHING HOSPITALS UNITED KINGDOM The Problem…. • Cardiovascular disease continues to be the biggest killer in the UK today • Almost 200,000 deaths per year • One in three premature deaths • Half of these CHD • A quarter stroke • Most can be prevented/delayed Objectives • Prevention: Primary versus Secondary • Coronary Artery Disease (CHD) Risk Factors • Q RISK 2 Risk Assessment • Do You Know Your Numbers? AND your Pulse ? • Q&A INTER-HEART: 52 Countries - every inhabited continent 15,152 cases with14,820 control group • ”Disease” related risk factors - Diabetes Hypertension Abdominal obesity ApoB/ApoA1 • Behaviour related risk factors Alcohol intake Exercise Psychosocial stress Current smoking INTERHEART Study ”nine potentially modifiable risk factors account for over 90% of the risk of an initial acute myocardial infarction” Population attributable risk fractions Smoking Hypertension Lipids (ApoB/A1 ratio) Abdom obesity Diabetes Fruit & Veg Alcohol Physical Activity Psychosocial Other Salim Yusuf et al . Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study). Lancet 2004 364 9437 ____________________________________________________________ Lifetime Risk of Coronary Heart Disease in the Framingham Study ______________________________________________________________ Men At age 40 years: 48.6% At age 70 years: 34.9% Women 31.7% 24.2% _________________________________________________________________ Lloyd-Jones et al. Lancet 1999; 353:89-92 Life style is a Driver of CVD Physical inactivity Life style intervention Excessive food intake Stress Smoking Obesity Hypertension Risk factor modification Diabetes Dyslipidaemia Atherosclerosis Chronic heart failure Atherosclerosis Arterial & venous thrombosis/ cardiac & cerebral events Arrhythmia Cardiovascular risk factors Non-modifiable: Age Gender Family History Ethnicity Socio-economic status Modifiable: Smoking Hypertension Obesity Hyperlipidaemia Salt intake Alcohol intake Diet Diabetes Physical activity Psychosocial factors Healthy Lifestyle? Physical activity • If maintained BP can be reduced by 3.8 to 2.6 mmHg, systolic and diastolic • 30 minutes - on five or more days/wk • Reduces the risk of CHD by more than 18%, • If no exercise is taken studies show that people are 30% more likely to become hypertensive. DE-NIAL IS JUST NOT A RIVER IN EGYPT Abdominal ObesityKNOW YOUR FIGURES • BMI – Normal < 25 – Obese 25-29.9 – Obese > 30 • Waist circumference – > 40 inches in men – > 35 inches in women • Waist circumference is more sensitive of risk of heart attack than BMI New Definition of High Blood Pressure • Old – BP a number to keep below 140/90 • New - a disease of the blood vessel where vascular biology is altered – Arteries cannot vasodilate properly and sodium and glucose accumulate in the arterial wall • New Goals 140 systolic / 90 diastolic – Lowers damage to heart brain, eyes, kidneys, pancreas, blood vessels of the legs/feet, sexual function What is Cholesterol? • Cholesterol is used to form cell membranes • LDL (BAD) pro-inflammatory – High levels are a predictor of atherosclerosis and heart disease • HDL (GOOD) anti-inflammatory – Removes excess cholesterol from arteries – Slows the growth of plaques – High levels protect against heart attack – Low levels increase risk http://www.fundaciondiabetes.org/activ/prevenir_obesidad/images/obesidad.jpg Cholesterol Management Guidelines Lower LDL Increase HDL • Exercise • Smoking Cessation • Weight Reduction • • • • < 7% saturated fat 10-25 grams fiber 2 grams plant stanols like Take Control Statins Questionable: • Alcohol – Red Wine • Estrogen Definition of Metabolic Syndrome Central obesity (waist circumference ≥ 94cm for European men and ≥ 80cms for European women) and any two of the four factors below: • ↑ Trigs ≥ 1.7 mmol/L or treatment for this • ↓ HDL < 1.03 mmol/L in men, < 1.29 mmol/L in women or specific treatment for this • ↑ BP ≥130/85 or treatment of previously diagnosed hypertension • ↑ FPG ≥ 5.6mmol/L or diagnosed T2 diabetes International Diabetes Federation, 2004 Alcohol intake • Low to moderate intake is associated with a • • • • lower risk of CVD Heavy alcohol is associated with high risk for hypertension and stroke Drinkers of more than 35 units/wk double their risk of mortality Binge drinking strongly associated with a large rise in BP Women drinking more than ever before. Red Flags • Blood pressure • Cholesterol >160/100 mmHg >7.5 mmol/l GIVE SOUND ADVICE Smoking • Strong association with CVD • Smoking as few as 3 per/day doubles risk of MI or death • Best quit success with counselling and pharmacological therapy • Level of risk falls with abstinence Health Benefits after Smoking Cessation Stress Management INTERHEART Study confirmed that psychosocial factors can contribute to sudden cardiac death Well being Wellbeing in Lancashire Q risk-2 Levels of risk • <10% risk over the next 10 years classed as low CVD risk • 10-20% risk over the next 10 years - classed as moderately increased CVD risk • >20% estimated risk over the next 10 years - classed as high risk. Putting prevention first • National vascular checks programme • Commenced 04/09 • Comprehensive CV risk assessment to be offered to all aged 40-74 • PCT delivery It’s all atheroma…. • • • • • Common aetiology Systemic disease Risk factors Common treatment aim Prevention of events The “Calcium Score” Source: services.epnet.com/getimage.aspx?imageiid=6857 EBCT = electron-beam computed tomography NHS Health Checks Programme Multi-level framework for identifying facilitators and barriers to attaining a healthy life Macro Level Economic Policies; Government Policies; Laws; Media; Technology; Industry Relations ; Transport Micro environment Level Local Community; School settings; Worksites Fast food outlets; Cafes & restaurants Household Level Food availability; Role models; Culture; Feeding Styles Individual Level Demographic factors Biology; Genetics; Flavour experiences; Learning history Action Plan 1. Get a annual check-up, know your numbers and follow-up – – – 2. 3. 4. 5. 6. Monitor your cholesterol and fasting blood glucose BP targets vary according to patients Check thyroid, liver and kidney function, Vitamin D levels, hormones Examine your diet and get a nutrition assessment with a dietitian Exercise Non-Negotiable daily appointment for you 30-60 minutes 5 days a week Develop a management plan to control stress and anxiety and depression... and seek help if no improvement Quit smoking Learn to measure your own pulse – practice brings perfection Balance your life when possible… …and make time for fun… And help others to achieve well-being We, the cardiology team at LTH THROUGH IMPROVED PATIENT CARE & COMMUNICATION Between primary and secondary care