Novel Therapeutic Agents State Of The Art Targeting
advertisement

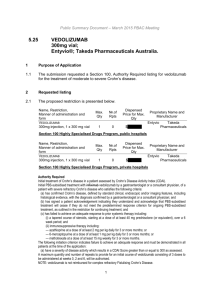
Positioning our recent and future advances in therapies for Crohn’s disease William J. Sandborn, MD Professor & Chief, Division of Gastroenterology Director, UCSD IBD Center Recent and future advances • Azathioprine – new data • Deep remission and treat to target • New agents Mild to moderate disease Rifaximin EIR Moderate to severe disease Vedolizumab (anti-alpha 4 beta 7) Ustekinumab (anti-interleukin 12/23 Tocilizumab (anti-interleukin 6) Tofacitinib (Janus Kinase [JAK] inhibitor) Eldelumab (Anti-IP 10) Top Down Therapy With Azathioprine + Prednisone Versus Step Up Therapy With Prednisone And Then Azathioprine In Adults With Newly Diagnosed Crohn’s Disease Cosnes J. Gastroenterology 2013 Top Down Therapy With Azathioprine + Prednisone Versus Prednisone In Adults With Newly Diagnosed Crohn’s Disease Sustained steroid free remission Survival free of relapse Panes J. Gastroenterology 2013 Treat-to-Target Algorithm ) CRP, C-reactive protein. Bouguen G, et al. Clin Gastroenterol Hepatol. 2013 Sep 10. [Epub Ahead of Print] Rifaximin Extended Intestinal Release for Crohn’s Disease: Results at Week 12 Prantera C, et al. Gastroenterology 2012 Therapeutic Targets for Lymphocyte Trafficking Leucocyte Adhesion NATALIZUMAB CD 11a/CD18 VEDOLIZUMAB LEUCOCYTE 41 (VLA-4) 47 ISIS-2302 CCX282-B CCR9 MAdCAM mAb (PF547659) ICAM-1 CCL-25 MAdCAM-1 ACTIVATED INTESTINAL MICROVASCULAR ENDOTHELIAL CELLS Adapted from Danese S Gut 2011;60:998-1008 ETROLIZUMAB VCAM-1 Vedolizumab: A Humanized, Monoclonal Antibody (mAb) Against 47 Integrins N • Targets only a4b7 integrin • Created by insertion of ACT1 CDRs into human IgG1 framework • Two amino acid substitutions abrogate Fc-receptor binding and complement fixation (ADCC) • IV infusion over 30 – 60 minutes N N CDR1 CDR2 CDR3 N VH VL CH1 CL C C CH2 CH3 C C Vedolizumab For Active Crohn’s Disease Response and Remission at Week 8 P=NS P=0.04 Response or Remission (%) • 185 patients with active Crohn’s disease receiving a stable dose of 5ASA or antibiotics or no medical therapy • Randomized to receive IV doses of placebo, 0.5 mg/kg, or 2.0 mg/kg MLN02 on days 1 and 29 • The primary endpoint was % clinical response (decrease in CDAI of 70 points) at day 57 • Secondary endpoint was % remission (CDAI < 150) at day 57 • Saturation of 47 on peripheral blood lymphocytes was not consistently achieved Feagan Clinical Gastroenterology & Hepatology 2008 Vedolizumab For Active Crohn’s Disease Remission at Week 8 * * p-value < 0.05 ITT population * * Feagan Clinical Gastroenterology & Hepatology 2008 MLN0002 induced a significantly greater clinical remission rate in patients with Crohn’s disease compared to placebo (2 mg/kg group) at days 15, 29, and 57. Vedolizumab (Anti-Alpha 4 Beta 7 Integrin) For Moderately-to-Severely Active Crohn’s Disease: Results at Week 6 in 368 Patients Induction ITT Population Patients, % P=0.23 P=0.02 95% CI: Δ 7.8 1.2, 14.3 Δ 5.7 –3.6, 15.0 Sandborn W. N Engl J Med 2013 Vedolizumab (Anti- 47 Integrin) For Maintenance of Response in Moderately-toSeverely Active Crohn’s Disease: Results at Week 52 in 461 Patients Maintenance ITT Population * ** ** ** * Patients, % * Δ17.4 Δ14.7 Δ13.4 Δ15.3 Δ15.9 Δ12.9 Δ7.2 Δ2.0 *P<0.05 **P<0.01 †CS tapering began in responders at 6 weeks; for others, as soon as a clinical response was achieved. Sandborn W. N Engl J Med 2013 Other Drugs in this Class • Anti-MAdCAM1 (PF-00547,659) • Etrolizumab (anti-7, rhumab beta 7) • Anti-7 (AMG181) Biology of Interleukins 12 and 23 IL-12 Stimulus TLR? AntiIL-12/23 p35 p40 IL-12R1 2 Ag Antigen Presenting Cell MHCII CD4+ TCR IL-23R IL-12R1 p19 p40 IL-23 AntiIL-12/23 X IFNg (Th1) IL-17 (Th17) Anti-IL-12/23 • Ustekinumab and briakinumab are fully human IgG1 monoclonal antibodies • Bind the p40 subunit of human IL-12/23 • Prevent IL-12 and IL-23 from binding IL-12Rb1 • Normalize IL-12 and IL23 mediated signaling, cellular activation, and cytokine production • In development in Crohn’s disease and psoriasis Ustekinumab (anti-IL 12/23p40) for Induction of Clinical Response in Moderate to Severe Crohn’s Disease All Patients 60 P=.02 P=.019 P=.335 P=.337 20 0 2 4 6 Weeks 1.2 100 Infliximab-Experienced Patients (%) 80 40 Previously Treated with Infliximab Placebo Ustekinumab Median CRP (mg/dL) Patients (%) 100 80 60 P=.046 P=.001 P=.004 P=.022 4 6 8 40 20 0 2 8 CRP in All Patients Weeks Week 0 Week 8 1.0 0.8 0.6 0.4 0.2 0 Subcutaneous Intravenous Placebo Subcutaneous Intravenous Ustekinumab Sandborn WJ. Gastroenterology 2008;135:1130-1141. Ustekinumab (Anti-IL-12/23p40) for Induction of Moderate to Severe Crohn’s Disease Clinical Response Clinical Remission + + + + + + + + + + +p<0.05 vs. PBO by CMH test Sandborn WJ. N Engl J Med 2012; 367:1519-1528 Ustekinumab (Anti-IL-12/23p40) for Maintenance of Moderate to Severe Crohn’s Disease p<0.001 p=0.029 Sandborn WJ. N Engl J Med 2012; 367:1519-1528 Tofacitinib an Oral Janus Kinase (JK) Inhibitor Cytokine α γ β JAK P STAT STAT STAT JAK P STAT P Tofacitinib blocks phosphorylation of STAT and downstream activation P mRNA P Cytokine Effects on the immune system IL-2 Stimulate the proliferation and differentiation of Th, Tc, B, and natural killer (NK) cells IL-4 Induce the differentiation of Th0 to Th2 Induce immunoglobulin switching IL-7 Promote the development, proliferation and survival of T, B, and NK cells IL-9 Stimulate intrathymic T cell development IL-15 Promote the proliferation, cytotoxicity and cytokine production of NK cells IL-21 Enhance T and B cell function Tofacitinib (CP-690,550) is a novel, small-molecule, oral JAK inhibitor Tofacitinib inhibits JAK1, JAK2, and JAK3 in vitro with functional cellular specificity for JAK1 and JAK3 over JAK2. Importantly, tofacitinib directly or indirectly modulates signaling for an important subset of pro-inflammatory cytokines including IL-2, -4, -7, -9, -15, and -21 Sandborn W. New England Journal of Medicine 2012 Tofacitinib for Induction in Moderate to Severe Crohn’s Disease: Clinical Response and Remission at Week 4 Clinical Response-70 Estimated clinical response rate (80% CIs) Clinical Response-100 49.9% 60 42.9% 48.0% 44.8% 50 60 40.8% 50 33.7% 40 40 30 30 20 20 10 10 N=34 N=36 N=34 N=35 0 38.8% 28.1% N=34 N=36 N=34 N=35 0 Placebo 1 mg BID 5 mg BID Tofacitinib Sandborn W. Gastroenterology 2011 Abstract 15 mg BID Placebo 1 mg BID 5 mg BID Tofacitinib 15 mg BID Mean percentage change from baseline in log transformed CRP (mg/L) in those patients with baseline CRP ≥5 mg/L (B) Sandborn W. Gastroenterology 2011 Abstract Tocilizumab (Humanized Monoclonal Antibody Interleukin-6 Receptor – Previously Atlizumab or MRA) For Active Crohn’s Disease • 36 patients with active Crohn’s disease (CDAI > 150, ↑ CRP) • Randomized to receive IV placebo, tocilizumab (previously atlizumab, MRA) 8 mg/kg every 2 weeks, or atlizumab 8 mg/kg every 4 weeks for 12 weeks • The endpoints were % response (decrease in CDAI 70) and remission (CDAI 150) at week 12 • Frequency of adverse events similar in all groups P=0.019 P=NS Ito Gastroenterology 2004 Other Drugs in this Class • BMS-945429 (fully human antibody to interleukin-6) • PF-04236921 (fully human IgG2 antibody to interleukin-6) Interferon Gamma Inducible Protein 10 (IP-10 or CXCL-10) Belongs to CXC family of chemokine ligands Induced by IFN- and produced by various cell types including hematopoietic & stromal cells Mechanism of action CXCR3-mediated recruitment of T cells to inflamed tissues CXCR3-independent (or dependent) modulation of functions of other cells including epithelial, endothelial and islet cells CXCR3 IP-10 Unidentified receptor Heparan sulfate TLR4 (?) T cell ↑ Trafficking Epithelial ↓ Proliferation & Migration1,2 Endothelial ↓ Proliferation3 Islet cell ↑ Apoptosis4 1 Suzuki et al. Pathology International 2007; 57(7):413-420; 2. Soejima et al, J Immun 2001; 167:6576-6582; 3. Luster et al. J Exp Med 1995; 182:219-231; 4. Schulthess et al. Cell Metabolism 2009;9(2):125-139 Drug in this Class • Eldelumab (fully human antibody to IP-10) Conclusions • Top down therapy with steroids and azathioprine is not effective in adults with newly diagnosed Crohn’s disease • Treatment goals in Crohn’s disease are evolving towards deep remission achieved via a treat to target strategy • Agents targeted against multiple targets including beta 7 integrin, MAdCAM-1, and the p40 subunit of interleukin 12/23, and possibly JAK, IP-10, and interleukin-6, hold great promise for the future