High_Risk_Antepartum_Nursing_Care_4
advertisement

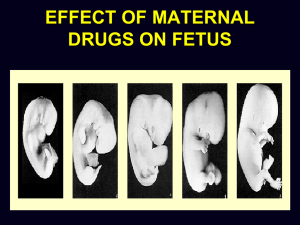
Sickle Cell Anemia Nursing Care: Monitor fetal status Provide emotional support RH Sensitization RH Sensitization is a condition in which a Rh-negative women becomes pregnant with a Rh-positive fetus and may become sensitized to Rh antigen and develops anti-Rh antibodies which may cross the placenta in subsequent pregnancies with Rh-positive fetuses and destroy the RBC’s. Complications: Erythroblastosis fetalis Hydrops fetalis Hyperbilirubinemia /Kernicterus Fetal dead RH Incompatibility Rh Sensitization All pregnant women should have a Type and Rh and an indirect Coombs. Pregnant women who are Rh-negative should have : Serial Indirect Coombs Unsensitized Rh-negative clients should have RhoGam: During pregnancy at 28-32 weeks gestation After any invasive procedures. In the Postpartum period within 72 hours. RH Incompatibility Nursing Care: Teach Client about the importance of complying with prenatal visits, laboratory testing, and RhoGam injection Check Laboratory results on all pregnant clients . Report findings of the client having Rh-negative blood and indirect Coombs results. Follow through if invasive procedures are done or after delivery about RhoGam. Support client who has developed fetal complications from Rh incompatibility Hyperthyroidism and Pregnancy HYPERTHYROIDISM is an endocrine disorder in which there is a excessive amount of the thyroid hormone produced. Complications in pregnancy: Thyrotoxicosis(Thyroid storm) Cardiac Dysrrhythmia’s Preeclampsia Malnutrition Fetal complications: abortion, premature delivery Neonatal complications: Prematurity, hyperthyroidism Hyperthyroidism In Pregnancy Review of the clinical manifestation of Hyperthyroidism Tachycardia and Palpitations Nervousness Weakness Tremors Heat intolerance Weight loss despite eating regular diet, Hair loss Diarrhea Hyperemesis gravidarum T4 and T3 are elevated an TSH decreased Hyperthyroidism and Pregnancy NSG. DX: Alt. Nutrition, less than body requirements Risk for injury Knowledge deficit Nsg Care Assess the client for clinical manifestation of complications of the hyperthyroidism or pregnancy Monitor lab tests- thyroid function tests Administer antithyroid medications- Propylthiouracil (PTU) Assist the client to meet her nutritional needs during the pregnancy with education and evaluation of diet . Hyperthyroidism in Pregnancy Nsg. Care Daily weights Monitor fetal status Emotional support Hypothyroidism in Pregnancy Hypothyroidism is a condition where thyroid does not produce enough thyroid hormone Complications Decreased fertility Abortions Stillborns And congenital malformations Review of the clinical manifestations of hypothyroidism Cold intolerance Weight gain Dryness of skin Puffy face Constipation Mental dullness Hypothyroidism in Pregnancy Laboratory Findings Low T4 and T3 and elevated TSH levels Nsg. Diagnosis Risk for Maternal/Fetal Injury Knowledge deficit Nsg Care Preconception Care- treatment of Thyroxine prior to getting pregnant Administer Levothyroxine Monitor TSH levels and T4 levels Instruct the client about the importance of medical therapy Monitor fetal status with FMC or NST’s Systemic Lupus Erythematosus in Pregnancy Systemic Lupus Erythematous(SLE) is a chronic, multisystem autoimmune disorder Complications in pregnancy Renal Failure Cardiac Problems CNS Problems Preeclampsia Abortions Fetal Loss Newborn- prematurity, congenital heart block, and neonatal lupus IUGR Exacerbation of SLE Systemic Lupus Erythematosus in Pregnancy Review of the clinical manifestations of SLE Joint pain Skin rash nephritis Pericarditis Anemia Leukopenia Thrombosis of multiorgans Fever neuropsychiatric Systemic Lupus Erythematosus in Pregnancy Laboratory Findings with SLE Leukopenia- WBC under 4,500 Thrombocyctopenia- PLt- under 100,000 Anemia- Hg- under 10 Positive direct Coombs’ test Positive Anticardiolipin antibodies Positive tests for rheumatic factors False Positive test for syphilis Positive antinuclear antibodies Increased serum creatine and decreased creatine clearance and proteinuria Cont. SLE in Pregnancy NSG Diagnosis Risk for Maternal and Fetal Injury Knowledge Deficit Anxiety or Fear NSG Care Preconceptation Care Instruct the client to see her health care providers frequently and to follow the medical therapy Monitor the client and the fetus and neonate for complications Administer Medications as order Prednisone Aspirin Cyclophosphamide( Cytoxan)- only for life-threatening conditions Azathioprine (Imuran) Anticardiolipin Antibody Syndrome Anticardiolipin Antibody Syndrome is an autoimmune disorder which the client has the Anticardiolipin antibodies. It can be seen in clients with or without SLE. It can produce negative outcomes in pregnancy and fetal loss Complications of Anticardiolipin antibody syndrome in Pregnancy Maternal Thrombosis Cerebral vascular accidents, Amaurosis fumax Transient ischemic attacks SLE Autoimmune thrombocytopenia Anticardiolipin Antibody Syndrome Cont. Complications Fetal Complications Abortions Fetal loss IUGR Placental insufficiency Clinical Manifestations Several Fetal Losses Spontaneous Abortions Laboratory findings Positive serum Anticardiolipin antibody titer Other abnormal immunologic studies Anticardiolipin Antibody Syndrome Nsg Diagnosis Risk for Maternal and Fetal Injury Anxiety or Fear Nsg Care Administer medications Immunosuppressant drugs- corticosteroids and others Aspirin Anticoagulants-Heparin Instruct on medication therapy Monitor client and fetus for complications Emotional support Myasthenia gravis in Pregnancy Myasthenia gravis (MG)is a complex autoimmune disorder that affects the neuromuscular system . Complication of MG in Pregnancy Exacerbation of the myasthenia gravis or a myasthenic crisis Maternal mortality because of respiratory arrest Pregnancy loss Premature labor Transient Neonatal Myasthenia Gravis Pulmonary Hypoplasia of the neonate Myasthenia Gravis in Pregnancy Review of the clinical manifestations of MG Progressive muscle weakness Difficulty in swallowing Ptosis Slurred speech Fatigue Problems breathing NSG Diagnosis Risk for Maternal and Fetal Injury Anxiety or Fear Fatigue Alter nutrition Risk for aspiration Myasthenia Gravis in Pregnancy NSG Care Monitor client and fetus for complications Administer medications – Many medications will exacerbate MG .Check any medication prior to give it. See chart Acetylcholinesterase drugs Pyridostigmine bromide ( Mestinon) po or parental if client can not swallow Check that client can swallow first Anticholinergics ( Atropine)for drug over dose Corticosteroids- Prednisone Instruct client on therapy regimen and compliance with the therapy and seeing health care providers regularly. Monitor client closely in Labor. Myasthenia Gravis In pregnancy Note Magnesium sulfate is absolutely contraindicated for clients who have Myasthenia Gravis Prepare room with suction ,oxygen, and ambu bag and check emergency equipment. Check infant at time of birth and in nursery for sucking and muscle tone. Watch when the baby feeds. Provide frequent rest periods for mother Deep Vein Thrombosis in Pregnancy Deep Vein Thrombosis (DVT)is a condition where blood clots form in the veins. Complications of DVT in Pregnancy Vascular occlusion Embolism Pulmonary embolus Hypoxia Acidosis death Deep Vein Thrombosis in Pregnancy Clinical Manifestations of DVT Muscle pain Tenderness and swelling of calf Positive Homan’s sign Diagnostic parameters Doppler ultrasonography Venography may cause risk to fetus Impedance plethysmorgraphy Deep Vein Thrombosis in Pregnancy NSG Diagnosis Alter. Tissue Perfusion Risk for Injury NSG Care Maintain bedrest during the acute phase Apply Ted hose Monitor fetal status Administer Anticoagulation therapy Heparin-IV the Subcutaneous Follow protocols for anticoagulant therapy NO Warfarin Coumadin Deep Vein Thrombosis In Pregnancy NSG Care No heparin therapy once labor starts. Monitor laboratory testing PT, APTT, INR, Blood clotting times Infections Types of infections: TORCH STI’s Other TORCH TORCH is a group of infections which can cause serious problems to the fetus T= Toxoplasmosis O= Other- Hepatitis -HIV R= Rubella C= Cytomegalovirus (CMV) H= Herpes Toxoplasmosis Toxoplasmosis is a protozoan infection which is acquired by the infestation of raw meat and handling of raw meat in mass qualities, cat feces and handling cat litter. If the pregnant acquires toxoplasmosis during pregnancy it can be passed the fetus via the placenta. Maternal effects are mild-flu-like symptoms Fetal-abortion, and congenital effects Neonatal effects- CNS lesions which could lead to hydrocephy, microcephaly, seizures and chronic retinitis Toxoplasmosis Pregnant Clients should not handled cat litter or cat feces. When handling cats wash hands afterwards Pregnant clients should not eat raw meat and when handling large amounts of raw meat they should wear gloves. Wash hands after handling raw meat Other Hepatitis is a viral infection. There are several different types. HAV and HBV are the must common seen in the fetus. HAV is acquired through fecal commination. HBV is acquired through body secretions-blood and genital secretions HBV effects on the client are fever, malaise, nausea, and abdominal discomfort and maybe liver failure. HBV effects on the fetus preterm birth and fetal death. The Neonate can be born with the infection Rubella Rubella is a viral infection that is spread by droplets or cross the placenta. It is also called the German Measles. Rubella titers are drawn on all pregnant women Rubella titer of 1:8 or more indicated immunity Rubella less than 1:8-example a titer of 1:6 or 1:4 indicates the client is non-immune. The client will need a Rubella immunization after delivery. Rubella effects on the client are fever, rash and mild lymphedema. Fetal effects are abortion, congenital anomalies and death Cytomegalovirus Cytomegalovirus (CMV) is a viral infection through respiratory droplets and body fluids and cross the placenta. CMV effects on the pregnant client are asympotomatic illness, cervical discharge, or mononucleosis-like syndrome. CMV effects on the fetus are fetal death or severe generalized disease, hemolytic anemia, jaundice, hydrocephaly, microcephy. CMV effects on the neonate are pneumonia, hepatosplenomegaly and deafness Herpes Simplex Virus Herpes Simplex Virus (HSV)is a viral infection that is spread by exposure to the vesicular lesions. HSV effects on the pregnant client are blisters which are painful, rash, fever, malaise, nausea, and headaches. HSV effects on the fetus are abortion, preterm labor, stillborn, IUGR- transplacental spread of infection is rare. HSV effects on the neonate are skin lesions, mental retardation, and microcephaly STI’s Human Immunodeficiency Virus (HIV) Chlamydia Syphilis Hepatitis B Group Beta Streptococci (GBS) Herpes Gonorrhea Human papillomavis (HPV) Urinary Tract Infections in Pregnancy Lower UTI’s – Cystitis Can cause preterm labor and pyelonephritis Upper UTI’s- Pyelonephritis Can cause preterm labor , sepsis, and renal failure Medications Cephalosporin's Ampicillins or Amoxicillin No Sulfonamide within 4 weeks of delivery can cause kernicterus in the neonate No Trimethoprim in early pregnancy No Tetracyclines Epilepsy in Pregnancy Epilepsy is a neurologic disorder in which there is recurrent seizure activity. The client who is pregnant and has epilepsy could have an increased risk for seizures , abortions, premature labor, and stillborn infants. Many anticonvulsants can produce teratogenic effects Phenytoin(Dilantin) Carbamazepine Dapakote The pharmokenetics of the seizure medication is effect by the changes in physiology during pregnancy. Trauma in Pregnancy Trauma in pregnancy Abdominal Trauma can be caused by Accidents such as falls or automobile accidents (MVA) Assault With weapons Abuse/violence Complications unique to pregnancy of abdominal trauma Placenta abruption Preterm labor Uterine trauma or rupture Bladder trauma or rupture Maternal or Fetal death Trauma in Pregnancy Clinical Manifestations History of trauma or accident Visible injuries Pain Signs of Shock Uterine activity Abdominal swelling or firmness Nonreassuring fetal Heart Pattern Nsg diagnosis Risk for Injury Anxiety Alt. Tissue Perfusion Fear Trauma in Pregnancy NSG Care Assess and triage the serious of injures ABC’s Start Iv with Large bore catheter Monitor for clinical manifestations of shock and /or hemorrhage Monitor uterine activity Monitor fetal heart pattern I&O-hourly Be Prepare for a delivery of the baby Notify ICN staff Emotional support Cholcycstitis and Cholelithiasis in Pregnancy Cholcycstitis and Cholelithiasis are common during pregnancy. Clinical manifestations Right upper quadrant tenderness and pain Murphy” Sign Attacks after meals Pain with nausea and vomiting Medical Treatment during pregnancy Low Fat Diet Cont. NSG Care Monitor for signs of Gall bladder obstruction Instruct client on low fat diet Less than 20 grams of fat Calories such come mainly from carbohydrates Plenty of fruit and vegetables Lean meats Only 10-12 % of calories such be protein A pregnant client will not be able to have lipotripesy or drugs to dissolve gall stones. Surgery in Pregnancy The problem with surgery in pregnancy will vary depending on the surgery. Complications that are unique with pregnancy preterm labor, and fetal injury from various cause such as hypoxia, medications, and trauma. Close monitoring for labor and the fetal status are required SUBSTANCE ABUSE in Pregnancy Substance Abuse is a major problem in the United States . It is estimated that 10% of pregnant abuse 0r use some substance during pregnancy. (Tobacco, alcohol or other drugs) All pregnant women should be screened for substance abuse. See text for the effects of drugs on the fetus and neonate and pregnancy For now