Christine Struthers, RN, MScN APN, Cardiac Telehealth
advertisement
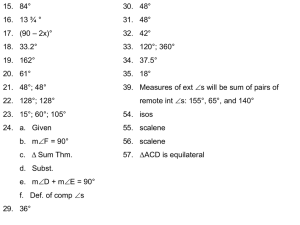
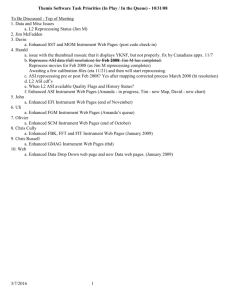
Telehomecare: Outcomes and Patient Experiences Heather Sherrard VP Clinical Services University of Ottawa Heart Institute 2012 • Only tertiary cardiac service provider for the region • Over 50 % of our patients come from outside the Ottawa area • High disease rates outside of the urban areas Telehealth Framework • Strategies using technology to improve the care delivered to patients – Enhances care – Improves access – Assists patients to stay in their communities – Improves patient satisfaction – Efficient use of resources Telehealth Technologies Broadband connection in the region Monitoring of patients in their home Interactive voice response using automated calling to care for patients Why home monitoring • The majority of patients live outside the Ottawa area • Majority of HF care is not in the hands of HF specialists • HF is a chronic condition characterized by episodic clinical deterioration interspersed with periods of apparent stability • HF remains the most common diagnosis that brings a patient to hospital for medical admission • Readmission rates can be as high as 25% at 1 month and 50% within the first year • Congestion is one of the main causes of readmission • Self-care strategies have a positive impact on decreasing readmission • Multidisciplinary approach has produced + outcomes Telehome Monitoring Technology Outcome Evidence Authors Study Outcomes Goldberg, A. et al ( 2002) Wharf Trial RCT n=280 6 month f/u ↓ mortality ↓ ED visits ↑ QOL Cleland, J. et al (2005) RCT n=426 8 month f/u ↓ mortality ↓ LOS Antonicelli, R. et al (2008) RCT n=57 12 month f/u ↓ mortality ↓readmission ↑compliance, BB & statin use, health perception Woodend, K. et al (2008) RCT n=249 ACS & HF 12 month f/u ↓readmission (ACS) ↑QOL & functional status Outcome Evidence • Cochrane Review (August 2010) Structured Telephone Support or Telemonitoring Programs for Patients with Chronic Heart Failure • 25 peer reviewed RCT + 5 published abstracts • 16 evaluated structured telephone support (n=5613) • 11 evaluated telemonitoring (n=2710) • 2 tested both interventions • Telemonitoring reduced all cause mortality (P<0.0001) • Both interventions reduced CHF-related hospitalization, QOL, reduced costs & improved NYHA Heart Institute Outcomes • Heart failure cohort of 121 patients (2008): 69.4% had 1-2 admissions for HF in previous 6 months prior to THM versus 14.8 % in 6 months post THM (each admission has LOS of 7 days at $1000/day) • Case-matched cohort (2009): 91 THM patients matched by EF, age (average 70 yrs.) & gender to usual care showed significant difference in the 6 month readmission rate in THM group (p<0.001) • THM & the elderly (2010): 594 HF patients divided into 2 cohorts <75 (n=350) & >75 (n=244) showed no difference in # of medication adjustments, # of calls, monitoring duration, or outcomes (ER visits, admission, death) between the 2 groups Innovation Diffusion • • • • • • • • Program started 7 years ago as a research initiative Nurse managed with medical lead available for issues 1 APN + 20 monitors (only from the Institute) 5 day operation, 0800-1600 with support from Nursing Coordinators for off hour coverage No home visits, Greyhound bus used for returns Non physician referrals accepted Intake letter to all HCP Monitoring duration 3-4 months on average with lots of flexibility Operations-now… • 1500 patients have been followed to date • 1 RN for ~100 patients/day (40-50 monitors) • Monitoring duration 3-4 months with plan to transitional to less intensive HF IVR follow-up (q 2 weekly automated calls) • Hub and spoke model for the region • 158 monitors & scales, GPRS bridge modems for digital lines or no land lines, 35 pocket ECG, 20 glucose cables, 20 INR units • Transitional Care framework adopted Regional Program Montfort TOH-Civic, OGH QCH UOHI THM THM THM THM THM THM THM THM THM THM THM THM THM THM THM THM THM Funding • 75 % of initial equipment funded through grants & research • Permanent staff funded through operations • Leverage to improve bed capacity @ $1000/day, decrease wait time for admission, improve provider capacity • Cost avoidance model Lessons Learned • Using regular phone lines is easy & cost effective • Patients are successful at connecting equipment in their homes. Equipment return by bus is feasible. No distance barriers. • The technology is reliable, producing valid patient data & EHR • The technology can be adapted to meet individual patient needs: volume, language, frequency of transmissions, clinical questions • Infrastructure promotes collaborative care model • No billing issues Doing the right thing, at the right time, in the right place! cstruthers@ottawaheart.ca