PCA - Agency for Clinical Innovation
advertisement
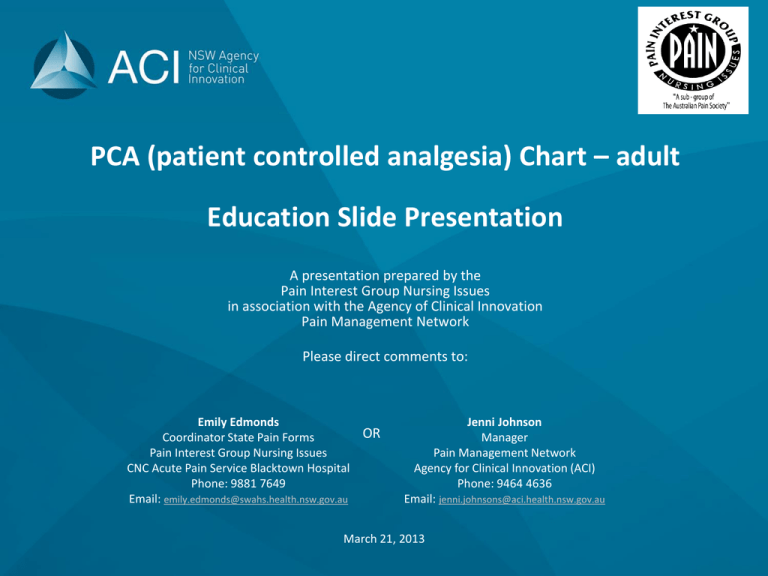
PCA (patient controlled analgesia) Chart – adult Education Slide Presentation A presentation prepared by the Pain Interest Group Nursing Issues in association with the Agency of Clinical Innovation Pain Management Network Please direct comments to: Emily Edmonds OR Coordinator State Pain Forms Pain Interest Group Nursing Issues CNC Acute Pain Service Blacktown Hospital Phone: 9881 7649 Email: emily.edmonds@swahs.health.nsw.gov.au Jenni Johnson Manager Pain Management Network Agency for Clinical Innovation (ACI) Phone: 9464 4636 Email: jenni.johnsons@aci.health.nsw.gov.au March 21, 2013 PCA (patient controlled analgesia) chart - adult The PCA prescription and observation chart for adult patients has been developed by a team of experts in the field of acute pain including clinical nurse consultants, anaesthetists and pharmacy representatives. This PCA chart is not suitable for use in paediatric patients. Standardisation of this chart promotes best practice in prescribing, pain assessment and management of adverse effects in those patients receiving an opioid via PCA. 2 Aim of this presentation: This presentation aims to explain how to use the chart for prescribing a PCA how to record the administration and discard of drugs used for PCA how to complete the clinical observations guidelines on the management of patients receiving PCA including the management of adverse effects 3 Booklet format Prescription valid for 4 days Observation pages for 4 days PCA chart - adult Page 1 Management guidelines Page 2 PCA prescription - PCA program - Neuraxial opioid + PCA - Naloxone prescription 4 Page 3 PCA drug administration - Drug discard - Naloxone administration PCA chart - adult Inside pages: Observation pages for up to 4 days Back page: Clinical Review and Rapid Response Criteria 5 (Between the Flags) Prescription page: Patient label and allergy adverse reactions PCA prescription PCA program - Allows for 2 further changes to the program Record of administration of a neuraxial opioid 6 Prescription for naloxone OR ‘sticker affixed’ stating existing standing order PCA prescription: Below is an EXAMPLE prescription Refer to hospital PCA policy for local guidelines on PCA prescribing Handwrite patient details OR affix patient label Prescriber to complete patient allergy and ADR section in full PSmith SMITH (First prescriber to check patient label is correct) Private patients: require a signature from the referring Doctor to the Pain Service 22/4/13 PLEASE REFER TO YOUR LOCAL HOSPITAL POLICY FOR PCA DRUG SOLUTIONS 7 PCA prescription: IV Morphine Below is an EXAMPLE prescription Refer to hospital PCA policy for local guidelines on PCA prescribing 60 mg A PCA prescription is for one opioid only. When changing from one opioid to another, a new PCA chart must be commenced 60 mL NIL TSmith 22/04/13 SMITH Space is provided for an additional drug to be added if necessary PCA prescription to include route, primary drug (e.g. morphine or fentanyl), total amount in mg or microgram and total volume Prescriber’s signature and printed name 8 Space provided for pharmacist reconciliation PCA program: 23/04/13 10:00 09:00 Lockout interval in minutes PCA bolus dose (state unit of drug and volume) Primary drug and concentration State: mg or microgram per mL Date and time 22/04/13 Below is an EXAMPLE program Refer to hospital PCA policy for local guidelines on PCA prescribing Background infusion (State mg or microgram and mL per hour) Morphine 1mg 1mg 1 5 mins NIL Morphine 1mg 2mg 2 5 mins 1mg When changing from one opioid to another, a new PCA chart must be commenced Two additional rows are provided for changes to the PCA program 9 1 TSmith SMITH S.Jack JACK Prescriber’s signature and print name Neuraxial opioid + PCA: IF a dose of opioid has been administered via the spinal or epidural route during a procedure, AND the patient is to receive a PCA, the following is to be completed The frequency of observations (hourly for 6 hours or hourly for 12 hours) must be determined by the medical officer who administered the opioid dose 22/04/13 10:00 Morphine Spinal 10 200 micrograms TSmith SMITH Naloxone prescription: 02/04/13 Naloxone Naloxone is indicated for SEDATION SCORE 3 (difficult to rouse or unresponsive) OR SEDATION SCORE 2 (constantly drowsy unable to stay awake) and a RESPIRATORY RATE LESS THAN OR EQUAL TO 5 breaths per minute. IV 100 micrograms X4 This section MUST be completed in full OR a sticker affixed which states the standing order PRIOR to any administration of naloxone. 11 2 -3 minutely TSmith SMITH Administration and discard of PCA opioid and administration of naloxone: PCA commenced The fold out section includes space for the documentation of : - PCA commenced Discard of remaining PCA opioid or drug Naloxone administration Discard of any remaining PCA opioid or drug Naloxone that may have been administered 12 Administration and discard of PCA drug: 22/04/13 22/04/13 10:00 20:00 THall BLoh Any opioid or drug remaining from a syringe or bag MUST be recorded on the corresponding row from its administration SRose 22/04/13 20:00 NIL JLucas 23/04/13 09:00 15 mL IF a PCA syringe or bag is empty when the next one is commenced, document ‘NIL’ discarded 13 BLoh JLucas Plambert TBuckley There are 14 rows provided to record PCA administration and discard Record of naloxone administered: Naloxone may only be administered when the prescription section of the PCA chart has been completed in full OR if a standing order sticker is affixed 02/03/13 08:30 IV 100 micrograms Plambert TBuckley 02/03/13 08:33 IV 100 micrograms Plambert TBuckley 02/03/13 08:36 IV 100 micrograms Plambert TBuckley 02/03/13 08:39 IV 100 micrograms Plambert TBuckley 14 Clinical Review & Rapid Response Criteria: The back page of the PCA chart displays instructions explaining when to make a Clinical Review or a Rapid Response. These instructions incorporate Track and Trigger color zones (from the Between the Flags Program) to promote the recognition of the deteriorating patient associated with the administration of opioids 15 Clinical Review Criteria: 16 Rapid Response Criteria: 17 PCA Management Guidelines are provided on the ‘fold-out’ front page of the PCA chart For detailed information regarding PCA prescribing and management refer to local hospital PCA policy or procedure PCA can be ceased according to instructions in the medical record: Date and time prompt provided (Check local policy for use of this prompt) 18 There is space provided for the contact details of your Acute Pain Service or equivalent medical officer who manages PCA Observations: A patient label must be affixed or details written on each page that records observations The PCA chart provides observations for a maximum of 4 days. If the PCA continues beyond 4 days, a new PCA chart must be started and a new prescription written. 19 Documenting observations: Pain Assessment: ‘R’ for rest ‘M’ for movement 22/04/13 M M R M R R R M R R 20 Documenting observations: A sedation score or a respiratory rate in the ‘Yellow Zone’ requires a Clinical Review by the Acute Pain Service Sedation, respiratory rate & oxygen therapy (or equivalent medical officer) A sedation score or a respiratory rate in the ‘Red Zone’ requires a Rapid Response to be initiated AND contact the Acute Pain Service (or equivalent medical officer) 2L NP 2L 2L NP NP Oxygen Device Key shown on front PCA Management Guidelines page 21 2L NP 6L FM Assessments must be recorded graphically as shown Documenting observations: Nausea or vomiting, PCA delivery 2 mg 10 mg 1 mg 1 mg 2 13 10 2 13 mg 20 mg 25 mg 1 mg 1 mg NIL 16 25 30 13 20 25 JS Nausea or vomiting assessment Total primary PCA dose (cumulative) Circle the unit that is being used Background infusion rate (if in use) Total demands / good demands (different pumps use different words to describe how many times the button is pressed) Ondanestron given JS JS JS 22 TJ PCA program checked: once per shift and on patient transfer - to ensure the pump program matches the prescription Comments section blank for free text Assessor’s initial The next two slides detail the front page PCA Management Guidelines 23 24 25 The standardisation of this chart promotes best practice in prescribing, pain assessment and management of adverse effects in those patients receiving an opioid via PCA. Comments or questions can be directed to your implementation officer or the project leaders Emily Edmonds or Jenni Johnson (for contact details see introduction slide) The feedback register can be located on the ACI website: http://www.aci.health.nsw.gov.au/networks/pain-management/acute-pain-forms 26