Part 2 PM - Metadon.net
advertisement
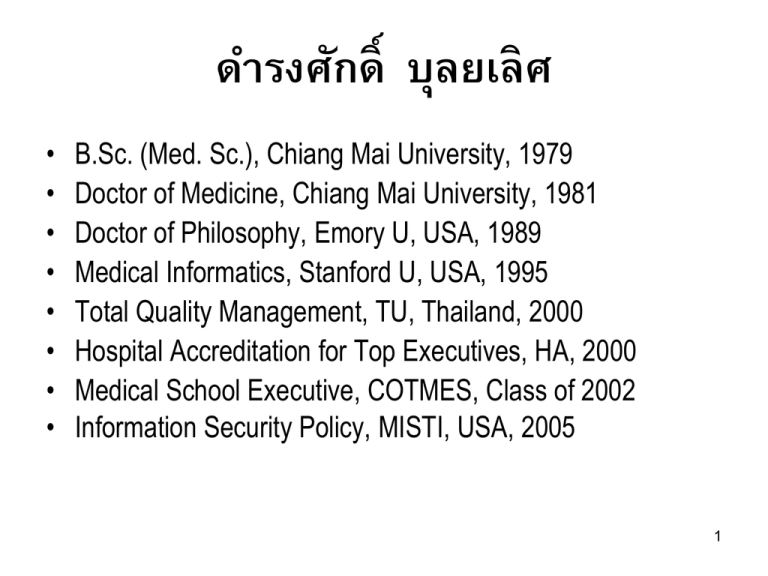
ดำรงศักด์ ิ บุลยเลิศ • • • • • • • • B.Sc. (Med. Sc.), Chiang Mai University, 1979 Doctor of Medicine, Chiang Mai University, 1981 Doctor of Philosophy, Emory U, USA, 1989 Medical Informatics, Stanford U, USA, 1995 Total Quality Management, TU, Thailand, 2000 Hospital Accreditation for Top Executives, HA, 2000 Medical School Executive, COTMES, Class of 2002 Information Security Policy, MISTI, USA, 2005 1 ICT Impacts on Healthcare Sector • Objectives – Patient outcomes remain the same over the past 2 decades – Processes are being improved but without directions. – Your job is to provide recommendation to healthcare providers (hospitals) on what to do to mitigate the situation 2 Healthcare XPD % GDP (World Bank, 2012) 20 18 16 East Asia & Pacific (all income levels) 14 East Asia & Pacific (developing only) European Union 12 10 North America World Japan 8 Malaysia Myanmar 6 4 Philippines Singapore Thailand 2 0 3 GDP (in Billion US$) ผลิตภัณฑ์มวลรวมในประเทศ (มูลค่าทางการตลาดของสินค้าและการบริการทีผ่ ลิตได้) Thailand 400,000,000,000.00 350,000,000,000.00 300,000,000,000.00 250,000,000,000.00 200,000,000,000.00 Thailand 150,000,000,000.00 100,000,000,000.00 50,000,000,000.00 0.00 1993199419951996199719981999200020012002200320042005200620072008200920102011 4 Common Causes of Illness (per 1,000) 600.0 500.0 400.0 2007 300.0 2008 2009 2010 200.0 100.0 0.0 Respiratory D Circulatory D Gastrointestinal Musculoskeletal D D Endocrine and metabolism D Infection, infestation 5 Missions of Healthcare Facility: Public and Private 1. Health promotion (Poor outcome) – Main function receiving little attention. Exercise and diet. 2. Disease prevention (Poor outcome) – Environment, personal hygiene and city sanitation including early disease detection. 3. Treatment (Very poor outcome) – Too much focus due to interest and gain (nepotism and cronyism). 4. Rehabilitation (unacceptable outcome) – Basic obligation for any illness. 6 • Organizations in Public Sector exist because of government mandate and not because of any vision • Mission begets Vision and not the other way around – HA, TQA, etc. on vision vs mission • Practically almost all hospitals have been accredited during the past 20 years, but the situation remains the same. • The authority and hospitals are lost. It is obvious. 7 • The concept of production line applies to hospital operation. • Input > Processes > Output > Outcome > Impact • Input = a patient with high blood pressure • Process = diagnosis and treatment • Output = blood pressure is normalized • Outcome = patient health is restored • Impact = healthy individual is productive, etc. 8 • A lot of processes (mostly campaigns) have been publicized and implemented. • Yet, the outcomes are unchanged or worsening. • How do we know that the situations are not improving? • The health statistics data says so. – Mortality, Complication, Length of Stay, Cost • Composite indices are hard to monitor. We need simple indicators. 9 Basic Indicators Required A. Patient safety indicators 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Foreign Object Retained After Surgery Air Embolism Blood Incompatibility Stage III and IV Pressure Ulcers Falls and Trauma Manifestations of Poor Glycemic Control Catheter-Associated Urinary Tract Infection (UTI) Vascular Catheter-Associated Infection Surgical Site Infection Deep Vein Thrombosis (DVT)/Pulmonary Embolism (PE) B. Drug-related indicators C. Lab-related indicators D. Waiting times for outpatient services and elective interventions E. Personnel indicators F. Customer satisfaction rates and complaint rates 10 • In order to run a hospital we need an information system largely known as Hospital Information System • Basic requirement – – – – Operation Planning Communication Documentation and reporting 11 Hypothetico-deductive Approach Patient presents with a problem Initial hypotheses ID, CC, HPI Ask questions Patient is cured; no further care required More questions PI, PH, FH, Social, ROS Patient dies Observe Results Laboratory tests Refine hypotheses Radiologic studies Chronic diseases Treat patient accordingly PE Examine patient Select most likely diagnosis EKG, etc. 12 Medical Informatics: Computer Applications in Healthcare and Biomedicine, 2nd edition. • To serve a patient, information recording requires an equivalent of 1,600 tables (in relational database approach) • Many issues to be considered in developing a hospital information system 13 Relational Concept and the Real World 14 15 Systems Design Some issues to be considered 1. Quality and style of interface 2. Convenience 3. Speed and response 4. Security 5. Integration 16 Systems Design: Network • Network infrastructure – – – – How many subnets in a hierarchical network? VLAN? How many functional subnets (intranets)? Public vs private IP address scheme (IP V4 vs V6) Intranet bandwidth requirement: core, distributive and access – Wireless for mobile computing? 17 • Internet bandwidth requirement – Personal access, e.g., online journals, Google, etc. – Personal communication: email, Skype, etc. – Public access: webpage presence 18 Systems Design: Hardware • Server: mainframe, mini or microcomputer • Input device: keyboard, mouse, barcode reader, RFID • Output device: monitor, pooled vs stand alone printer, etc. • Storage device with RAIDs (what RAID level) – Speed vs redundancy – Dedicated device such as SAN 19 • RAID 0: block striping, no parity • RAID 1: mirroring without parity or striping (duplexing with separate controller) • RAID 10: mirroring and striping (many 1ry and 2ry) • RAID 2: bit level striping • RAID 3: byte level striping with dedicated parity • RAID 4: block level striping with dedicated parity • RAID 5: block level striping with distributed parity • RAID 6: block level stripping with double distributed parity 20 Systems Design: Software • Operating system: proprietary v.s. open source • Applications: – Buy proprietary products (ผูผ้ ลิตทรงสิทธิ ์) off the shelf with/without add-on programming – Build in-house application from scratch – Implement a public domain software, e.g., VistA (Veterans Health Information Systems and Technology Architecture) – Outsourcing completely: Theresa system of Grady M. 21 Systems Design: Software • Source code management: – Software escrow (สัญญาซอฟท์แวร์) option • Information exchange functionality – Information useless if not exchangeable – HL7 protocol should be standard and built-in 22 Systems Design: Computing Model Centralized, modular and distributed computing • Centralized computing: all functions in a single homogeneous application. • Modular computing: subsystems working together in one application, each can be enabled/disabled. • Distributed computing: many stand-alone systems working together in an integrated environment 23 • Database model: relational vs. non-relational • Computing architecture: – Data management, business logic and user interface model – 2-tier client/server: thick client vs thin client – 3-tier client/server: scalability – N-tier client/server • Any role of mobile computing? 24 Depressing Fact • Almost all (99.99%) of healthcare personnel in charge of ICT in public sector are ICT illiterate. – Self improvement, probably little reading – Most books read are on programming but not systems designs and development. • Most of them are computer hackers (geeks). • They don’t easily take consultancy. 25 For hospital information system: 6 major functions. 1. 2. 3. 4. 5. 6. Patient management Departmental Management Care delivery and clinical documentation Clinical decision support Financial and resource management Managed care support 26 Basic Functional Modules • • • • • • • • Medical record system Outpatient system Laboratory system Radiology system including PACS Pharmacy system Patient financial system Physician workbench Nursing workbench • Inpatient system • Operating theater/room system • Labor room system • Anesthesiology system • Dietetic system • Central Sterile Supply System • Laundry Service System 27 Two Integration Requirements • Data integration: a single piece of information is generated once and then shared amongst various healthcare personnel, e.g., drug prescription – Patient arrives at the hospital and is registered by medical record department – Patient arrives at the outpatient clinic – Physician enters clinical information – Through computerized order entry system, physician places an order for a drug – Cashier system receives the payment – Pharmacy system dispenses and releases the drug – Nurse could view what the patient receives 28 Two Integration Requirements • Process integration (process improvement) – Only a few ways to get a job done, not indefinite ways. • Patient registration: by MR personnel, nurses, physicians using standard operating procedures. Everyone will do the same approach, same user interface. – Transactions can be carried out by more than one authorized individual. • Cashier functions may be performed by financial/accounting personnel as well as authorized users such as management. 29 MoPH Report Requirement • All stakeholders perform data entry according to individual roles. • All stakeholders get relevant data from the pool. • Each hospital sends a set of data to the MoPH and stakeholders retrieve relevant data. – One change request per year from a central location and each hospital responds/submits information to that body. Other Department retrieve relevant data from this central location. 30 Dept. A Hospital X Dept. B Hospital Y Dept. C Hospital Z Dept. A Dept. B Dept. C Current mode of operation (Poor system, no audit) Hospital X MoPH Data Center Hospital Y Hospital Z 31 • Change management inefficiency coupling with lack of integration knowledge may lead to a complete implementation failure – Legacy pharmacy system story from KKU – Legacy lab system story from Ramathibodi Hospital 32 Software Issues • Build: can be 100% customized but time consuming, failure rate approaching 100% • Buy: customization almost impossible, but ready to serve. Major problem in patch management. • Best approach is to use integration engine to solve legacy issues, e.g., clearinghouse, rhapsody, ensemble, etc. 33 Uses of Medical Data 1. Create the basis of historical record – Medical record for life long service provision but patient health record for patient self-management and interagency exchange 2. Support communication among providers, internal and external (coding standards and standard for information exchange) 3. Anticipate future health problems 4. Record standard preventive measures 34 Uses of Medical Data 5. 6. 7. 8. Identify any deviations from expected trends Provide a legal record Support clinical research Serve as a source for indicator calculation – Mortality rate, complication rate, length of stay, expense 9. Etc. 35 Information Audit • International Standard – ISO 27001, 27002 36 ISO 27002 • • • • • • • • security policy: 99% of public hospitals have no policy organization of information security: ditto asset management: ditto human resources security: minimal physical and environmental security: partial communications and operations management: minimal access control: minimal and mostly password scheme information systems acquisition, development and maintenance: ditto • information security incident management: none • business continuity management: emergency power mostly • Compliance: none 37 Buying Issues • Procurement – How to establish a sound TOR as systems analysis takes forever. – Competition and e-auction requirement • Acquisition and maintenance – The project does not end at contract signing. It is just the beginning. Most agencies falsely mark this milestone as an indicator (process). • Project management 38 Project Management Quality PIC of CHRiST = 9 areas • Quality • Procurement, Integration, Communications • Cost, Human resources, Risk, Scope, Time • I Saw the Car Quickly Hit Charlie’s Rear Plate 39 Waterfall Model of SDLC 40 Implementation Issue • Scanning of medical records 41 Medical Record (paper vs. electronic) • • • • • • Availability Remote Access Simultaneous Access Legibility Information organization Completeness • Timely analysis • Research & education support • Initial Investment • Security issues • Reliability • Human errors 42