Dr Damodar Bachani_NCDs & Eye Health
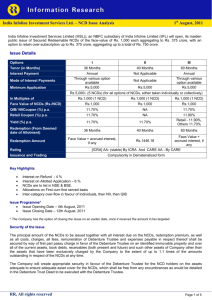
advertisement
NCDs & Eye Health Converging interests and opportunities for collaboration Course 17: Neglected Tropical Diseases & NCDs 9th GA of IAPB Hyderabad; 19th September 2012 Dr. Damodar Bachani, MD Percentage of NCD deaths, by cause in WHO Regions, 2008 100% Other NCDs % of Death 80% Diabetes 60% Respiratory diseases 40% Cancers 20% Cardiovascular diseases Ea s te Source: WHO global Health observatory 2011 http://apps.who.int/ghodata/ cif ic sia W es t er n Pa tA So ut hEa s rn M Eu ro pe n ed ite rr an ea ica Am er Th e Af ric s a 0% Four major NCDs cause 80% of deaths due to NCDs in all WHO Regions Distribution of deaths by major causeIndia 2001-2003 Others 9.9% (N=11,242) Injuries 9.6% (N=10,890) Noncommunicable disease 42.4% (N=48,170) Communicable disease, maternal & perinatal conditions, nutritional deficiencies 38.2% (N=43,390) Deaths due to NCDs outnumber deaths due to communicable diseases, maternal and perinatal causes and nutritional conditions combined Source: RGI-CGHR Million Death Study Causes of Death (%) in Urban Population (25 to 69 years) India: 2001-2003 Cardiovascular Diseases 17 32.8 Malignant & other Neoplasms COPD, Asthma & other Respiratory Diseases Diabetes Mellitus 4.3 Motor vehicle accidents 7.7 Unintentional Injuries 3.3 Digestive Diseases 5.8 Genito-urinary diseases 3.6 11.3 3.7 2.8 7.7 Tuberculosis Symptoms, signs & ill defined conditions Other causes 4 major NCDs- Cardiovascular diseases, Malignant & other Neoplasms, COPD, Asthma & other respiratory diseases & Diabetes Mellitus contributes to 55% of the total reported deaths in urban area Source :Special Survey of Deaths, Registrar General of India Causes of Death (%) in Rural Population (25 to 69 years) India: 2001-2003 Cardiovascular Diseases 19.6 COPD, Asthma, other Respiratory Diseases 22.9 Malignant & other Neoplasms Unintentional Injuries Intentional Self harm 5.5 Digestive Diseases 5.5 10.9 3.1 Tuberculosis Malaria Diarrhoeal Diseases 10.7 8.9 4.9 3.1 4.9 Symptoms, signs & ill defined conditions Other Causes 3 major NCDs-Cardiovascular diseases, COPD, Asthma & other respiratory diseases, Malignant & other Neoplasms contributes to 43% of the total reported deaths in rural area Source :Special Survey of Deaths, Registrar General of India National Health Programs for NCDs initiated before 2007 National Cancer Control Program National Blindness Control Program National Mental Health Program National Iodine Deficiency Disorders Control Program National Tobacco Control Program Trauma Care Facility on National Highways National Deafness Control Program National Health Programs initiated since 2007 National Program for Prevention and Control of Fluorosis Pilot Project on Oral Health National Program for Prevention and Control of Cancer, Diabetes, CVD, Stroke National Program for Health Care of the Elderly Pilot Program for Prevention of Burn injuries Upgradation of Department of PMR in Medical Colleges Disaster Management/Mobile Hospitals/ CBRN Organ and Tissue Transplant Strategies to address NCDs 2012-17 1. 2. 3. 4. 5. 6. 7. 8. 9. Health Promotion for healthy life styles that preclude NCDs and their risk factors Specific prevention to reduce exposure to risk factors Early Diagnosis through periodic/opportunistic screening of population and better diagnostic facilities Infrastructure Development and facilities required for management of NCDs Human Resources and their capacity building for prevention and treatment of NCDs Establish Emergency Medical Services with rapid referral systems to reduce disability and mortality due to NCDs Treatment and care of persons with NCDs including rehabilitation and palliative care Health Legislation and population and evidence based interventions wherever applicable through multisectoral approach for prevention of NCDs Building evidence for action through surveillance, monitoring and research. Services in Public Sector Health System Tertiary level Institute Medical Colleges, Tertiary Cancer Centres, Regional geriatric Centres, Centres of Excellence [Tertiary care, Training, Research] District Hospital NCD Clinic, Geriatric Clinic, Cardiac Care Unit, Cancer Care Facility etc. [Health Promotion; Early diagnosis & Management; Home Based Care; Day Care Facility] Community Health Center NCD Clinic, Geriatric Clinic [Health Promotion, Early diagnosis & Management; Laboratory Investigations, Home Based Care, Referral] Sub Center Screening Services [Health Promotion; Opportunistic Screening; Referral] Referral National Health Programmes A. Life Style Chronic Diseases Cancer 2. Tobacco Control 3. Diabetes, Cardiovascular Diseases (CVD) & Stroke 4. Chronic Obstructive Pulmonary Diseases* 5. Chronic Kidney Diseases* 6. Organ and Tissue Transplant 7. Mental Disorders 8. Prevention and Management of Nutritional Disorders & Obesity* 9. Iodine Deficiency Disorders 10. Fluorosis 11. Oro-dental disorders* * New 1. B. Disability Prevention & Rehabilitation 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. Trauma (including Road Traffic Accidents) Burn Injuries Disaster Response* Emergency Medical Services* Musculo-skeletal (Bone and Joint) Disorders* Physical Medicine & Rehabilitation Blindness Deafness Health Care of the Elderly (Geriatric Disorders) Neurological Disorders (Epilepsy, Autism, Dementia)* Congenital Diseases* Hereditary Blood Disorders (Sickle Cell Anaemia, Thalassemia, Haemophilia)* * New Experiences & Issues for Effective Implementation Health promotion and prevention need to be given more attention to reduce the incidence of NCDs and their risk factors. As NCDs are prevalent across the country, the programmes need to be expanded to the entire country to cover urban, rural and slum population The States need to be given flexibility in implementation of the programmes based on their public sector health system, prevalence and needs. The flexibility would be within broad policy framework. Experiences & Issues… (contd.) Convergence and integration would be critical in implementation of large number of interventions with a unified management structure at various levels Integration of cross cutting components like health promotion, prevention, screening of population, training, referral services, emergency medical services, public awareness, programme management, monitoring & evaluation etc. would save on costs and make implementation more effective. Opportunities & Challenges Political will Healthy Public Policy Resource Mobilization Sustainable Infrastructure & Systems Human resources & their capacity building Convergence & Integration Partnership & Collaboration Quality assurance, M&E for evidence Thanks