Rabies Presentation
advertisement
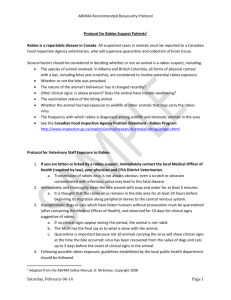
Rabies Rhabdovirus Doriann Prasek RN, BSN, CIC Manager Infection Prevention Overlook Medical Center Case Study: On 30 June 2011, a 73 year-old Haitian female with history of hypertension and diabetes mellitus type II presented to Emergency Department at OMC with right shoulder pain, chest pain, headaches , increased blood pressure and dysphasia. Ischemic heart disease was suspected, but ruled out. Emergency Department requested to evaluate patients dysphasia, however patient declined and said was able to drink water. She was released with pain medication, but returned to the Emergency Department the following day with shortness of breath, insomnia, and hallucinations. She was subsequently hospitalized due to deteriorating mental status. Case Study: On July 7, the NJDHSS was notified of patient hospitalized with acute encephalitis in which rabies was being considered but no known animal exposure had occurred as family had no recollection. Once arboviruses and other potential etiologies were ruled out, clinical samples were sent to the CDC for testing. Rabies virus antigens were identified in a nuchal (neck by hair line) skin biopsy on the 18th of July. Saliva was later found to be positive. The patient’s neurologic status continued to deteriorate leading to her death on the 20th of July. Case Study: After the rabies diagnosis was confirmed, family members in Haiti remembered that in April 2011, approximately 1 month before arriving in the United States, the patient had been bitten by a stray dog she had adopted. She did not consider the bite severe and did not seek medical attention. Rabies strain dog/mongoose variant from Dominican Republic and Haiti. Pathology Report CDC Specimen Test Results Pituitary, Spinal cord Rabies Virus Positive Liver, Spleen, Pancreas, Gallbladder Rabies Virus Negative Kidney, Adrenal Rabies Virus Negative Esophagus, Stomach Rabies Virus Negative Muscle, Skin Rabies Virus Negative Cervix, Uterus, Ovary, Fallopian Tube Rabies Virus Negative Cortex, Paraventricle, Cerebellum, Brain Stem, Spinal Cord, Hippocampus Rabies Virus Positive Evaluation of Healthcare Workers Exposure Starting on July 18, the risk for rabies virus exposure to healthcare workers were assessed through a questionnaire by NJDHSS and the hospital’s infection prevention program. Healthcare questionnaire was based on Risk Levels: Nil to Zero- no exposure at all Low-some known exposure or potential contact with infectious materials Medium- Definite contact with infectious materials, but PPE practices were followed High- Definite contact with infectious materials, with breaks in PPE practices. Or exposure to direct wound or mucosal contact with infectious materials, bites or scratches from patient. Recommendations for PEP: High- yes Medium- yes or no dependent on assessment of exposure Low- probably not Nil to Zero- no Summary of Results: Two hundred and forty-six (246) healthcare workers were identified as having possible contact with the patient during ED visits and hospitalization. 10 (4%) received PEP Of 10 healthcare worker: 5 had not followed standard infection prevention practices 2 had potential exposure to patient saliva at an open wound or mucous membrane 3 received PEP despite assessments of infection risks which were nil to low. Things That Worked Well: Rapid response and assistance from NJDHSS, Local Health Department and the CDC. Open communication and education with Administration, Physicians and Staff. Screening tool developed by the NJDHSS and CDC Continuous feedback by regulatory agencies Team work All efforts combined decreased the numbers of worried well. Lessons Learned: This is the third report of human rabies in the US acquired in Haiti and highlights the importance of a detailed history of a patient with travel from a rabiesendemic country, and the utility of consultation with medical and public health professionals related to animal bites regardless of perceived severity. Healthcare workers do not follow standard precautions CDC recommended respiratory precautions with any respiratory inducing procedures. When you say it can’t possibly be rabies, it is….. Important Websites: http://nj.gov/health/cd/documents/faq/rabies_faq.pdf http://www.cdc.gov/rabies/exposure www.uptodate.com http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6051a2.htm Questions?