Presentation by Dr. Tia Pham on the IHBPC Model

Photo Credit - Toronto Star , 2011
The Integrated Home-Based
Primary Care (IHBPC) Project
Dr. Sabrina Akhtar
TWFHT
Dr. Mark Nowaczynski
House Calls
Dr. Tracy Smith-Carrier
King’s, Western
Dr. Thuy-Nga Pham
SETFHT
Dr. Samir Sinha
UHN/MSH Geriatric s
Dipti Purbhoo
TC-CCAC
2
Rationale for our Collaborative – Why?
•
93% of Canadians aged 65 and older live at home, > 100,000 of them are homebound
•
Since 2000, five English systematic reviews published on home-based primary care with conflicting results on mortality, functional status and health care use and costs
Source: Stall et al, 20 th IAGG WORLD CONGRESS OF GERONTOLOGY AND GERIATRICS 2013
3
Background
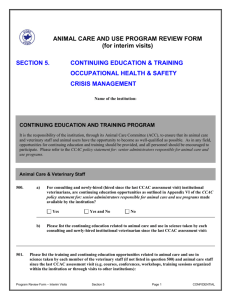
FEATURE HOME-BASED PRIMARY CARE OUTREACH HOME VISITS
Functional
Model
Ongoing comprehensive primary care in the home
Care Focus Complex and interrelated chronic disease management and social care issues
Time Course Ongoing
Home-based multidimensional
Geriatric assessments
Needs assessments
Personnel
Goals of
Care
Primary care provider–led interprofessional teams
Improve access to primary care
Consultation with possible limited follow-up
Varied, but typically nursing and allied health professionals
Assess needs and develop care plan
Source: Stall N, Nowaczynski M, Sinha SK. Back to the future: home-based primary care for older homebound Canadians: part 1: where we are now. Canadian family physician Medecin de famille canadien 2013;59(3):237-40.
4
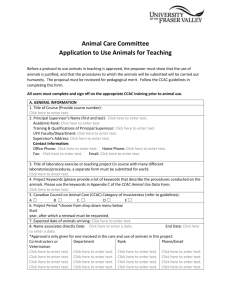
Who are our patients?
Integrated Home Based Primary Care Catchment
Taddle Creek FHT
MSH FHT
6
Patient Site Totals
Site
Mount Sinai Hospital
SMH
SETFHT
Sunnybrook
Taddle Creek
TWH
SPRINT
*TOTAL
*Totals as of March 26, 2014
Current Total
25
31
61
57
62
73
425
734
IHBPC Models of Primary Care
7
FHT Model:
Family Health Teams taking care of homebound patients that benefit from an interprofessional team delivery model (FPs, NPs, SW, OTs, Pharmacists)
CSS Model (SPRINT House Calls Model):
Primary Care Team (3 FPs, 1 NP, 2 OTs, 1 PT, 1 SW, 1 Team Coordinator etc.) embedded in a Community Support Services Agency
Early Analyses show 67% Die at Home Rate , and 14% and 29% lower hospital readmission rates at 30 and 90 days .
Emerging CHC/Hospital/CCAC Models:
In development! One of the FHT graduating PGY3 Care of the Elderly Fellows has joined a West End CCAC interprofessional team in providing IHBPC.
Program Objectives – What are we doing?
8
Patient Care Objectives Integrated Care Team Objectives
Provide a comprehensive and integrated approach to patient and client care
Develop shared understanding of roles, responsibilities and accountabilities between providers
Improve transitions in care between acute, primary care and community care settings
Improve communication among team members and across the continuum of care and organizations
Establish a network of specialists to support home-based primary care with recent urban telemedicine expansion
“Skype in your specialist”
Enhance care management partnerships between primary care and community care providers
9
What are we measuring?
Qualitative
Analysis
Quantitative and
Economic
Analysis
Quality
Improvement
Measures
Training &
Education
Interviews with
Patients,
Caregivers,
Team
Members &
External
Stakeholders
Analysis of
Hospitalizatio ns, ED visits using ICES data
Immunization rates, 7 day follow up after hospitalization, medication reconciliation, team conferences,
Advance Care
Planning
Operations and Education
Toolkits &
Curriculum
Development for
Competency
Based Training of Family
Medicine
Residents in
IHBPC
10
Qualitative Research
11
Interprofessional Team Experience
Explored
Team members ’ experiences providing IHBPC services vis-
à-vis providing usual care
The key characteristics of successful team functioning within the IHBPC environment
The facilitators of effective IHBPC service delivery
Areas of improvement (barriers)
Analysis Information
Grounded theory methodology
Sample = 7 sites (6 FHTs + 1 IHBPC
CSS team) in Toronto - winter of
2013
Purposive sampling approach
(Patton, 2002) by team member role
Team Members (n=17)
CCAC Care coordinators
Social Workers
Physicians
Occupational Therapists
Physician Assistant
Nurse Practitioners & Nurses
Pharmacists
12
Dimensions of IHBPC Service Delivery to
Team Members
Figure 1: Dimensions of IHBPC Service Delivery According to Team Members
Benefits
Provider Satisfaction
Enhanced Care Planning
Smooth Access to Services
Perception of Deferred Hospital Visits
Perceived Effectiveness in Improving Patient Outcomes
Improved Medication Management
Perceived Patient Satisfaction
Barriers
Demands on Time and Energy
Lack of Resources & Equipment
Administrative Load
Travel
Coordination Challenges
Negotiating the Home Environment
Integrated
Home-Based
Primary Care
Structural Context
Growing Population Requiring Care
Complexity of Patients
Recognition that Service is Necessary
Funding Restraints
Reluctance of Care Providers to Engage in IHBPC
Context of Team
Variety of Sizes & Composition of Teams
Differing Team Leads
Embedded in Diverse Organizational
Structures
CCAC/CSS Agency Supports
Facilitators of Interprofessional Working
Positive Relationships
Mechanisms for Communication
Organizational Supports in Place
Team Learning
Obstacles to Interprofessional Working
Conflict
Turf Issues
Unclear Roles
13
Context of IHBPC
The Population & Necessity of the
Service and CCAC Involvement
There are a significant number of seniors who can ’ t access their family doctors office for a variety of reasons:
Can’t access transportation
Dementia and cognitive impairments
Can ’ t sit in an office and wait for hours
Mental health
CCAC
…The introduction of CCAC in house, has streamlined the process which is amazing.
Types of Teams
Now, I would say my role is more of a team player. I am letting our nurse leader take more of the leadership of this & coordination role. So for me it is easier.
Well the doctor is the lead …I mean we all have roles…But there has to be somebody in charge of all of that, because if we all had control it would be not doable for anybody…
It ’ s, from what I can tell, it ’ s all through our physician assistant. So she ’ s sort of the quarterback & she gathers all of us together & whoever she needs help with, & then she helps carry out the plan.
14
Benefits of IHBPC
Benefits of the Context of
Home
…(I)t is making it easier because you can visually understand what their needs are:
you can tell if they are taking their medications you can tell if they have safety issues
the extent of their dementia becomes more rapidly obvious to you you can see where they keep their medications and can tell whether they can take their medications as you prescribed do they have dexterity issues with the blister packs, can they read the pills bottles, do they have somebody to administer them
are they living in a second floor bedroom & they can ’t access food on the main floor or a bathroom on the main floor & they are living on the 2nd floor
So you can address multiple issues quickly, so from that respect I find it easier to create a care plan that works for the patient.
Sense that IHBPC Defers
Hospital Visits
I love the population and I think that we are stemming some emergency visits although that remains to be born out, that’s a difficult thing to measure as we all know. But based on the kind of presentations, and the phone calls we get from their providers, and the treatments that we’re giving, I think that probably we’re deferring visits…
I went out to see this guy last week and I could see something was brewing on his foot so I could deal with it before he went to emergency, you know?
That’s the one major change, that they can actually manage their care through us now without having to access emergency department services on every occasion.
15
Barriers
Administrative Load Travel
…After seeing the patient there ’ s a lot of kind of paper work & stuff that needs to be attended to, you know, you ’ re not seeing people with colds, you know.
One of the biggest barriers would be how far away the doctor or the person has to drive, right. It really should be no longer than 15 minutes, because than that ’ s a half hour for the drive, not including wherever you have to park.
16
Facilitators & Barriers of Team Collaboration
Variety of Communication
Mechanisms (Facilitators)
Using our computers and our blackberries, which everything goes into the client ’ s file…We are not missing anything using the interdisciplinary approach.
We also have biweekly meetings where we sit down & discuss new referrals, we discuss current cases, issues, good stories, bad stories, & housekeeping…
The weekly rounds seem to be the venue where things are discussed. I know there ’ s also some email correspondence that I have been part of as well around plans & they are sort of an on going dialogue.
We use a program called One Note for our patient charting. If a patient has passed away or needs urgent attention usually that warrants a phone call to another team member or at the very least an email. Communication folder is just a
“
Hey I just wanted to give you the heads up about this… ”
Turf Issues (Barrier)
I guess one of the other challenges…was that some of our physicians are not as embracing of a nurse going out to see their patients, or not their nurse going out to see their patient. I find that one of the very frustrating things, that there ’ s this protectionism of
“ my practice
” attitude, & we really have to move away from that. We need to remember it
’ s the patient that
’ s at the center of what we do, not the physician or the physician
’ s views. And that ’ s a challenge. It ’ s a challenge I have had in complex continuing care, it
’ s a challenge being out here.
17
System Wide Gains Thus Far
Family Health Teams
• Annual FHT ministry reports now require number of home visits provided by MDs and team members
CCAC
• Dedicated care coordinator embedded within primary care team highly effective
Communication with specialists and hospitals
• OTN urban telemedicine access to specialists, team conferences with specialists and hospital teams in case of admissions beneficial for complex patients
Increasing number of Family Medicine Trainees exposed to IHBPC
• Academic curriculum expansion in competencies in home-based and team based care
18