EPIDEMIOLOGY AND WHO
POSITION ON VACCINE
VIKASH KESHRI
MODERATOR : DR. ABHISHEK RAUT
INTRODUCTION
PROBLEM STATEMENT
EPIDEMIOLOGY
PREVENTION AND CONTROL
HEPATITIS B VACCINE
WHO POSITION ON HEPATITIS B VACCINE
INTRODUTION
Hepatitis b initially called as serum hepatits is an
acute systemic illness with major pathology in liver.
Besides 2 billion infected cases world wide
approximately 36 millions live with chronic
infection.
These chronically infected people are at increased
risk of death from cirrhosis of liver or
hepatocellular carcinoma.
PROBLEM STATEMENT
WORLD:
Hepatitis B is endemic in almost all part of world
60% of world population live in endemic area
Estimated 2 billion people infected
360 million live with chronic infection
600,000 person dies annually as result of consequence
of hepatitis B every year
Estimated 25% child dies in later life as a consequence
of hepatitis B infection.
Vaccine coverage estimated is 69%
Problem statement cont…..
SEAR:
Estimated one third population in the region infected
80 million carrier
Estimated 200,000 death occur annually
vaccine coverage 41% according to 2008 WHO-UNICEF
antigen study
INDIA:
fall in intermediate endemicity group
HBsAg prevalence between 2% to 7%.
Estimated 43-45 million cases per year.
40 million carriers.
100,000 death annually by disease related to HBV infection.
Of 25 million newborn annually, 1 milion runs lifetime
risk of HBV infection
EPIDEMIOLOGY
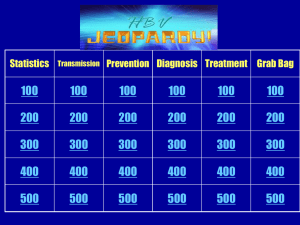
AGENT FACTOR:
Agent :
• Hepatitis B virus belongs to hepadenavirdae family.
• Complex 42 nm. Double stranded enveloped DNA virus.
• Also known as “Dane” particle.
• Has affinity for liver and hepatocytes
Reservoir of infection
Human being only reservoir
Infection spread by cases and carrier
Carrier defined as persistence of HBsAg > 6 months
Resistance of virus:
quite stable , can survive for days in environmental condition.
Can be destroyed by sodium hypochlorite
Also by autoclaving for 30 to 60 minutes.
Period of communicability:
from incubation period upto disappearnce of HBsAg and upto
appearance of antibody.
But can be years.
HOST FACTOR
AGE:
outcome age independent
For acute Hepatitis B occurs in 1% perinatal, 10% early
childhood (1-5 yrs.) and 30% in older children (>5 yrs.
Age)
Development of Chronic hepatitis is inversely
proportional to age
HIGH RISK GROUPS
Health care workers
High risk sexual behavior
Commercial sex worker
Frequent blood transfusion reciepient
Injectable drug users
Immunocompromised individuals
Infant of HBV carrier
Modes of transmission
Infective materials:
Blood and blood products, serous exudates, saliva,
seminal and vaginal fluids, etc.
Routes of transmission:
1. Percutaneous 2. sexual 3. perinatal
4. Others routes
Percutaneous routes
injectable drug users
Nonsexual contacts between individuals
Contact with intimate objects
Contact of open skin or mucous membrane with infected
materials.
Occupational exposure: needlestick injury, surgical
procedure, handling infected materials.
Rituals: circumcision, tatooing, nose and ear piercing.
Sexual routes
Sexual contact with infected person
Favourable factors:
-Contact with a person during active infection
- H/O sexually transmitted disease
- promiscuosity
- Male homosexuals
perinatal route:
important contributor of high prevalence of infection
Mostly around perinatal period.
Acute infection during third trimester increases risk.
In utero transmission very rare
No evidence of transmission via breast feeding
Other routes:
Interpersonal contact specially childhood. May be because of
skin to skin contact.
INCUBATION PERIOD:
Varies from 30 to 180 days
Average 75 days
HBsAg can be detected as early as 30 days and may persist
for several months to years.
Clinical features
Insidious onset
Early symptom : malaise, weakness , anorexia
Ranges from mild asymptomatic infection to fulminant
hepatitis to hepatocellular carcinoma to death.
Clinical infection
-jaundice
-flu like symptom
Acute hepatitis B infection
Recovery
Or
Immunity
Chronic
Carrier
Fulminant
hepatitis
Death
Asymptomatic
Or
Subclinical
infection
Minimal
liver
Disease
Primary
hepatocellular
carcinoma
Chronic
Hepatitis
cirrhosis
DEATH
PREVENTION AND CONTROL
GOALS OF PREVENTION:
to decrease prevalence of chronic carrier and chronic liver
disease
prevention of acute hepatitis B infection
Strategies:
Hepatitis B vaccination.
Screening of blood, plasma, organ and semen donor.
Universal precautions.
HEPATITIS B VACCINATION
Active immunization
Passive immunization
ACTIVE IMMUNIZATION
Two types of vaccine available
1. Plasma derived vaccine
2. Recombinant DNA vaccine
PLASMA DERIVED VACCINE:
Based on HBsAg derived from plasma of human carrier.
Formalin inactivated
Intramuscularly administered
Dose = 1 ml. (contains > 20 mcg. HBsAg.)
costlier
Recombinant DNA vaccine
Introduced in 1987 in USA.
Has replaced plasma derived vaccine.
Cost effective and equally effective
Available as monovalent or combined vaccine
Active substance:
-HBsAg derived from culture of yeast or mammalian cells
Adjuvant:
- Alum or thiomersal
Storage:
-2 to 8°c
- freezing avoided
-vaccine survive for 7 day at 45°C and for 1 month at 37°c
Administration
Age :
Ideal first dose at birth ( within 24 hours)
Next 2 or 3 dose according to immunization schedule
Can be given at any age
No. Of doses:
3 or 4
First at birth , second and third with DPT1 and DPT3.
First at birth, second, third and fourth with DPT and OPV
routine
Older child and adults 3 doses at day o, 1 month, 2 month
no need of booster dose.
Dose :
- 0.5 ml. for child < 10 years
- 1 ml. For adults
Route :
- intramuscularly
Site :
- left upper arm for adults
- anterolateral thigh for young infants
Hepatitis B vaccine in immunocompromised state:
- not contraindicated but special attention required
Immunogenicity and Duration of protection
Usually life long immunity
Hepatitis B or even chronic carrier stage rarely occur.
Role of natural booster by sub- clinical infection is yet to be
proved
Adverse reaction:
infrequent and rare
Myalgia , transient fever , local pain
No serious adverse effect
Very rarely anaphylactic reaction
No relation with G.B. syndrome or multiple myeloma
GACVS recommends excellent safety profile
Contraindications:
H/O allergic reaction to component of vaccine.
Pregnancy and lactation no contraindication.
HIV positive individual and premature babies can be given vaccine
CATCH UP STRATEGY:
Vaccinate older children and adults in low and intermediate
endemicity area for population immunity
Target age specific cohort and high risk individual
Strategy may be mandatory vaccination at school and college entry
and before joining job.
Target strategic point i.e. STD clinics, centre for IDUs.
Continuous surveillance.
PASSIVE IMMUNIZATION
Hepatitis B immunoglobulin used for temporary post-exposure
prophylaxis.
Combined active and passive vaccination better in following cases:
- Newborn of HBsAg +ve mother specially if baby +ve
- Percutaneous exposure
-Sexual exposure
- After liver transplant in case of recurrent HBV
infection
Time :
within 6 hours of exposure and maximum upto 48 hours.
Dose: 0.05 to 0.07 ml. / kg. body weight.
Provides short term passive immunity for 3 months.
WHO POSITION
All newborn should receive birth dose of hepatitis B within 24
hours of birth, in all countries irrespective of their immunity
status.
Immunization programme must include HBV.
Proper Reporting and monitoring
MCH care needs to be strenghthened
Schedule include :
- First birth dose within 24 hours of birth , followed by either
-2 dose schedule with 2 nd and 3rd dose with -DPT 1 and
DPT3
-Or 3 dose schedule with routine DPT 1 , 2 and 3.
No need of booster dose
Catch up compaign for older age group is important in
intermediate and low endemicity area.
Catch up compaign for infants and young children is important
in high endemicity area.
Other target group for catch up strategy can be high risk group.
GACVs confirms excellent safety profile.
WHO recommends all countries should develop goal for HBV
control according to their epidemiological situation
References
Park k., text book of preventive and social medicine, 20th
edition page no. 186 - 189
Manson’ text book tropical disease
Maxcy- rosaneu- last text book of public health
heahttp://www.who.int/immunization/topics/hepatitis_b/
en/index.htmllth
http://www.who.int/immunization/topics/hepatitis_b/en
/index.html