Overview of Evidence-Based Self-Management Programs, October
advertisement
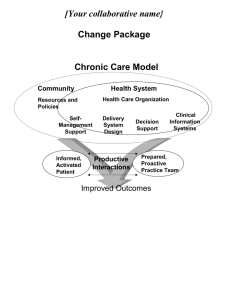
Overview of Evidence-Based Self-Management Programs October 7, 2013 Outline • • • • • Overview of Partners in Care Chronic Disease Self-Management Programs Los Angeles Caregiver Resource Centerd HomeMeds Program Home Support Program Mission To serve as a catalyst for shaping a new vision of health care by partnering with organizations, families and community leaders in the work of changing health care systems, changing communities and changing lives Partners in Care Who We Are Partners in Care is a transforming presence, an innovator and an advocate to shape the future of health care We address social and environmental determinants of health to broaden the impact of medicine We have a two-fold approach, creating and using evidence-based models for: provider/system practice change and enhanced patient self-management Changing the shape of health care through new community partnerships and innovations Building the New HCBS Services Model: Focus Areas Evidence-Based Self Management Assessments & Care Coordination Collaboratives /Networks/TA Care Transitions Intervention Evidence-Based Leadership Council Chronic Pain CBAS Eligibility Determination Care Coordination Network Diabetes (billable) Home Safety Evaluation Care Transitions Intervention Network Chronic Disease Matter of Balance Savvy Caregiver Powerful Tools for Caregivers Arthritis Foundation Exercise Arthritis Foundation Walk with Ease UCLA Early Memory Loss HomeMeds Care Coordination What is Self-Management? The actions that individuals living with chronic conditions must do in order to live a healthy life. Physical Activity Problem-Solving Medications Planning Using Your Mind Manage Fatigue Communication Better Breathing Healthy Eating Working with Health Professionals Understanding Emotions Managing Pain Chronic Disease Self-Management Education (CDSME) Program Overview Evidence based programs developed & licensed by Stanford University Patient Education Research Center Self-Management Programs • Chronic Disease Self- • Tomando Control Management* de su Salud (Spanish) • Diabetes (Eng/Spanish) • Chronic Pain *Leader manual available in Arabic, Bengali, Chinese, Dutch, French, German, Greek, Hindi, Italian, Japanese, Korean, Khmer, Norwegian, Punjabi, Russian, Somali, Swedish, Tagalog, Tamil, Turkish, Vietnamese Diabetes Self-Management Program • Developed at Stanford University by Kate Lorig, RN, Dr.PH • Patients with Type 2 diabetes learn to take charge and control of their diabetes. • Develop tools to understand and deal with: – Emotions – Manage medications – Worth with health care providers – Make weekly action plans for exercise and healthy eating Designed to empower participants through a mutually supportive and interactive education process Added benefit – socialize with new people! Chronic Pain Self-Management Program • Developed at Stanford University by Kate Lorig, RN, Dr.PH • Patients with Primary or Secondary Diagnosis of chronic pain learn to manage & lower their chronic pain. Participants Report: – Less Pain – Lower Dependency on Others – More Energy – Improved Mental Health – Increased satisfaction with life – More involvement in every day activities Designed to empower participants through a mutually supportive and interactive education process Added benefit – develop relationships with others suffering from chronic pain! CDSME Program Goals To build self-confidence & provide: Social Interaction Shared Experiences & Support Identification of Problems Reinterpretation of Symptoms Skill Development to Control Symptoms Program Design • 12 -16 participants – Two Trained Leaders – People with different conditions Six-week Program 2 ½ hours, one day a week Includes: Group discussions Activities Short lectures Book: Living a Healthy Life with Chronic Conditions Target Population People with at least one chronic condition – OR – A family member, friend or caregiver of someone with a chronic condition Stamina to attend 2 ½ hour session Cognitive function to participate CDSME Workshop Participant Health Outcomes Randomized, controlled trial of 1,000 participants Increase in Exercise Energy Psychological well-being Decrease in Pain and fatigue Depression Shortness of Breath Limitations on Social and role activities Overall Improved health status & quality of life Greater self-efficacy and empowerment Enhanced partnerships with physicians Sources: Lorig, KR et al. (1999). Med Care, 37:5-14; Lorig, KR et al. (2001). Eff Clin Pract, 4: 256-52; Lorig, KR et al. (2001). Med Care, 39: 1217-23. Health Care Utilization Effects • Results showed more appropriate utilization of health care resources through decreased: • • • • Outpatient visits Emergency room visits Hospitalizations Days in hospital Ultimate Result: Reduction in health care expenditures Testimonials • “Because I have been afflicted with Parkinson’s for over 20 years, I have suffered a great deal of depression. The skills you've taught me in maintaining positive thinking and combating depression have really helped to improve my condition.” John, age 69 • “I found the interaction with the other students in the class to be most enlightening. I realized that although I have a chronic illness I am not alone. Thank you for all the lessons in helping me to deal with this.” - Suzanne, age 57 • “The workshop put me back in charge of my life, and I feel great. I only wish I had done this sooner.” - Robert, age 68 Los Angeles Caregiver Resource Center (LACRC) Established in 1989, the LACRC provides information, support, training and respite assistance to families caregiving for a person with a brain impairment or chronic condition residing in Los Angeles county. This program is one of a network of 11 similar CRCs across California. As a program of Partners in Care Foundation, the LACRC helps identify caregiving individuals and links them with culturally and linguistically appropriate programs in their communities. LACRC Programs and Services: • Information and Referral • Support Groups (face to face and via the telephone) • Community Education (weekly or monthly events held in partnership with senior centers and other community-based organizations) • Caregiver Education: Evidence-based programs including Savvy Caregiver and Powerful Tools for Caregivers workshops. • Respite Assistance: Limited short –term grants to allow caregiving individuals to get relief from the many stressors related to providing care for their loved one. • Family Consultations: Assistance to caregivers in resolving and planning for immediate and long term care-related issues. Care Transitions • Health reform Section 3026 addresses high Medicare readmits in 30 days after discharge • CMS is funding tests of a new Medicare benefit – 101 nationally and 11 in California • The hospital partnerships fund CBOs – high risk are identified and seen in hospital/home and follow up calls • Forming a regional delivery system What a Home Visit Looks Like • Medication Risk Assessment – Room by room “Treasure hunt” – Assessment of possible adverse effects • Recent falls, dizziness, confusion, BP, pulse – Assessing client understanding and adherence • Environmental Assessment – Safety, cleanliness, maintenance, barriers to mobility – Evidence of problems – Fall Risks 22 The Problem- Medication Errors • Serious: Over 700,000 people go to ED each year for adverse drug events • Costly: Drug-related morbidity/mortality > $170 billion • Common: Up to 48% of community-dwelling elders have medication-related problems • Preventable: At least 25% of all harmful adverse drug events are preventable 23 Medications Related to Emergency Hospitalizations • Frequency and rates of hospitalization after ADE-related ED visits by older adults aged 65+* • Nearly half aged 80+ • 2/3 of hospitalizations due to unintentional overdose • Four medications/classes implicated alone or in combination in 67% of hospitalizations – Insulin and hyperglycemic medications – Anticoagulants & antiplatelets • High-risk-designated drugs implicated in 1.2% of hospitalizations * Emergency Hospitalizations for Adverse Drug Events in Older Americans. Daniel S. Budnitz, M.D., M.P.H., Maribeth C. Lovegrove, M.P.H., Nadine Shehab, Pharm.D., M.P.H., and Chesley L. Richards, M.D., M.P.H. N Engl J Med 2011;365:2002-12 24 The Importance a Home Visit • Uncovers many “secrets”… that prescribers may not know about – – – – – – – – – – Over-the-counter medications & supplements Medications prescribed by other providers Adverse effects such as falls, dizziness, confusion Assessment information Incorrect self-dosing Adherence issues “Un-manageable care” $4 co-pays at Wal-Mart < Part D co-pay $ Medications from other countries Medications “borrowed” from friends and family 25 Evidence-based Protocols • Protocols identified by national expert consensus panel* • Target problems that can be identified and resolved in the home • Likely to get a positive response by prescribers and minimize “alert overload” • Protocols • • • • Unnecessary therapeutic duplication Use of psychotropic drugs in patients with a reported recent fall and/or confusion Use of NSAID in patients at risk of PUD/gastrointestinal bleeding. Selected Cardiovascular medication problems » Sub-optimal blood pressure control » Orthostatic changes/low systolic BP » Slow pulse *"A model for improving medication use in home health care patients " Brown, N. J., Griffin, M. R., Ray, W. A., Meredith, S., Beers, M. H., Marren, J., Robles, M., Stergachis, A., Wood, A. J., & Avorn, J. (1998). Journal of the American Pharmaceutical Association, 38 (6), 696-702. 26 Further Evidence • USC Evaluation in nursing-home eligible communitydwelling population • Population: 615 Dual Eligibles, 65+ • Social workers & nurses collected data in home visit • Results ¹ ² • 49% had potential medication problems • 29%- pharmacist recommends intervention • 61% of clients referred to MD after pharmacist review had medication use improvement [1] Prevalence of Potential Medication Problems in Dually-Eligible Older Adults in Medicaid Waiver Services. Alkema GE, Wilber KW, Enguidanos SM, Frey D. An Pharmacotherapy. 12/07 [2] “The Role of Consultant Pharmacists in Reducing Medication Problems Among Older Adults Receiving Medicaid Waiver Services”. Alkema GE, Enguidanos SM, Wilber KW, Trufasiu M, Frey D. . The Consultant Pharmacist. February 2009, Volume 24, No. 2 27 Always looking for new partnerships Contact: June Simmons, CEO Partners in Care Foundation 818-837-3775 jsimmons@picf.org www.picf.org Bertha Sandoval Partners in Care Foundation 818-837-3775 x134 bsandoval@picf.org www.picf.org