IMI - PSI
advertisement
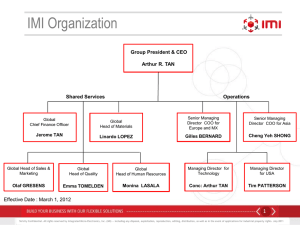
Finding your way through formal benefit-risk approaches for decisionmaking in drug regulation PSI Annual Conference 12th May 2014 London Professor Deborah Ashby School of Public Health Imperial College London The IMI-PROTECT • PROTECT1 (Pharmacoepidemiological Research on Outcomes of Therapeutics by a European ConsorTium) • “Improving and strengthening the monitoring of the benefit/risk of medicines marketed in the EU” including graphical representation of risk-benefit led by EMA with 31 public and private partners, 2009-2014 (www.imiprotect.eu) 1 PROTECT is receiving funding from the European Community’s Seventh Framework Programme (F7/2007-2013) for the Innovative Medicine Initiative (www.imi.europa.eu) 4 Partners in PROTECT Public Private Regulators: EMA (Co-ordinator) DKMA (DK) AEMPS (ES) EFPIA companies: GSK (Deputy Coordinator) MHRA (UK) Sanofi Roche Academic Institutions: University of Munich FICF (Barcelona) INSERM (Paris) Mario Negri Institute (Milan) Poznan University of Medical Sciences University of Groningen University of Utrecht Imperial College London University of Newcastle Novartis Pfizer Amgen Genzyme Merck Serono Others: WHO UMC GPRD SMEs: Outcome Europe PGRx (LA-SER) IAPO CEIFE Bayer Astra Zeneca Lundbeck NovoNordisk Takeda Eli Lilly 5 IMI- PROTECT Work Package 5 Benefit-risk integration and representation 6 Decision makers – who are they? Patients • Make decisions for themselves Healthcare providers • Make decisions based on prescribing lists NICE • Makes decisions on cost-effectiveness EMA/MHRA etc. • Makes decisions on quality, safety, efficacy and benefit-risk balance to individuals and public health Pharmaceutical companies • Makes decisions on what to develop for which licenses to apply 7 Challenges in medical decision-making • Should we formalise decision-making at all? • Which quantitative approach(es) to use? • Whose value preferences take priority – regulators, pharma, physicians or patients? • How do we find these preferences – simple elicitation, decision conferencing, discrete choice experiments….? • Do we need stakeholders’ preference a priori, or should we provide tools to allow individual decision-makers to explore their own preferences and the consequent decisions? • How do we communicate benefits and risks? 8 Methodologies available (and tested) PrOACT-URL NNT QALY INHB NNH BRAT PSM BRR Q-TWiST MCDA Impact numbers ITC DCE MTC SMAA SBRAM http://www.imi-protect.eu/benefitsRep.shtml 9 Disclaimers “The processes described and conclusions drawn from the work presented herein relate solely to the testing of methodologies and representations for the evaluation of benefit and risk of medicines. This report neither replaces nor is intended to replace or comment on any regulatory decisions made by national regulatory agencies, nor the European Medicines Agency.” 10 Recommendation Roadmap Exploration Evidence gathering and data preparation Conclusion and dissemination Analysis Planning 11 Stage 1: Planning • encourages stakeholders to focus on critical issues related to BR assessment • encourages sufficient thinking and thorough discussions between stakeholders to clearly define the purpose and context of the BR assessment • ensures clear detailed summary documentation of discussions and results • allows future analyses and updates to utilise the same foundations 12 Planning Toolbox PrOACT-URL BRAT Problem Define decision context Objective Identify benefit and risk outcomes Alternative Define the decision context Consequence Extract source data Customise framework Trade-off Assess outcome importance Uncertainty Display & interpret key BR metrics Risk tolerance Useful methodologies include: • non-quantitative / descriptive frameworks to organize data • tree diagrams and structured tables providing useful means of visualisation Linked decisions 13 An example of (value) tree diagram from natalizumab case study 14 Recommendation Roadmap Exploration Evidence gathering and data preparation Conclusion and dissemination Analysis Planning 15 Stage 2: Evidence gathering and data preparation • Identifies and extracts evidence relevant to the BR assessment in relation to the set criteria • Determines what data to be collected from anticipated type of BR analysis • Aggregating multiple sources of evidence, may require the use of estimation techniques • Encourages systematic handling of missing data • Requires engagement of clinical, statistical, epidemiological and database expertise 16 Evidence Gathering and Data Preparation Toolbox • Useful methodologies include: – Indirect/Mixed Treatment Comparison (ITC/MTC) – Probabilistic Simulation Method (PSM) – visualisation techniques such as structured and colourcoded tables, and network graphs to enhance the communication of data. 17 An example of MTC network in the natalizumab case study Natalizumab Direct (Polman 2006, EPAR) Indirect Indirect Placebo Direct Direct (Johnson 1998) (Jacobs 1996) Glatiramer acetate Interferon beta-1a Indirect 18 An example of colour-coded tables of data summary Outcome Natalizumab / pts Tysabri Risk Risk / 1000 Benefits 1000 pts Convenience Benefits Risk Difference (95% CI)/ 1000 pts - - - (-, -) Relapse (weight 3.9%) 280 450 -170 (-, -) Disability Progression (weight 5.6%) 110 140 -30 (-, -) Reactivation of serious herpes viral infections (weight 6.7%) PML (weight 55.9%) 80 2 70 0 10 2 (-26, 45) (-, -) Liver Toxicity Transaminases elevation (weight 11.2%) 50 40 10 (-16, 38) Reproductive Toxicity Congenital abnormalities (weight 5.6%) - - - (-, -) Neurological Disorders Seizures (weight 5.6%) 0 11 -11 (-23, 0) 236 312 -76 (-, -) Medical Benefits Infection Risks Convenience (weight 0.6%) Comparator Risk / 1000 pts Infusion/Injection reactions (weight 2.8%) Other Hypersensitivity reactions (weight 1.1%) 90 40 50 (20, 82) Flu-like reactions (weight 1.1%) 399 608 -209 (-320, -98) Higher for Drug A Higher for Tysabri Higher for Comparator 19 Recommendation Roadmap Exploration Evidence gathering and data preparation Conclusion and dissemination Analysis Planning 20 Stage 3: Analysis • Evaluates data collected at previous stage in a BR assessment • Quantifies the magnitudes of benefits and risks • Weighs or integrates quantitative measures of the BR balance depending on the type of analysis 21 Analysis toolbox - methodologies • Useful methodologies include – metric indices which provide numerical representations of benefits and risks e.g. Number Needed to Treat / Number Needed to Harm (NNT/NNH), Impact numbers – quantitative frameworks which model benefit-risk trade-off and balance benefits and risks e.g. MultiCriteria Decision Analysis (MCDA), Stochastic Multicriteria Acceptability Analysis (SMAA) – utility survey techniques which elicit stakeholders’ preference information e.g. Discrete Choice Experiment (DCE) 22 Analysis toolbox – example visualisations Different visuals for different tasks… …and how to produce them 23 Recommendation Roadmap Exploration Evidence gathering and data preparation Conclusion and dissemination Analysis Planning 24 Stage 4: Exploration • Assesses the robustness and sensitivity of the main results to various assumptions and sources of uncertainties • Assesses further consequences of a decision • Considers any impact or added value to the RMPs • Requires both statistical and clinical input 25 Exploration toolbox • Useful methodologies include: – ITC/MTC, PSM, SMAA – Utility survey techniques e.g. DCE, AHP, Swingweighting, MACBETH • Preferred visualisation techniques include: – the box, distribution, scatter, and forest/interval plots; tornado diagram; and techniques that are interactive with the user. 26 Natalizumab: Probabilistic MCDA Distribution of benefit-risk score P(natalizumab ranked 1st) ≈ 1 27 Recommendation Roadmap Exploration Evidence gathering and data preparation Conclusion and dissemination Analysis Planning 28 Stage 5: Conclusion and dissemination • The point at which a conclusion is reached • The results and consensus from the BR assessment are communicated to a wider audience • Explicitly states findings and conclusions that could influence future actions • Emphasises a transparent audit trail of the whole assessment process i.e. brings everything together and sets the course of action • Ensures the "big picture" overview is not lost 29 Summary • Choice of approach should match the complexity of the problem. • In most simple problems, simple descriptive framework is likely to be sufficient. • For more complex problems, a framework supplemented by quantitative models can facilitate consideration of trade-offs amongst the benefits and risks, address uncertainty, and potentially lead to a more comprehensive overall assessment. • To understand the perspective of a particular stakeholder, elicitation of preference values for weighing benefits and risks may be required. 30 Final remarks • Benefit-risk assessment methodologies support decision-making and are not intended to replace medical expertise. • It is not a linear or sequential but an iterative process. • Stakeholders such as patients and public involvement may add value and would lead to more clinically relevant decisions. 31 Acknowledgements • The research leading to these results was conducted as part of the PROTECT consortium (Pharmacoepidemiological Research on Outcomes of Therapeutics by a European ConsorTium, www.imiprotect.eu) which is a public-private partnership coordinated by the European Medicines Agency. • The PROTECT project has received support from the Innovative Medicine Initiative Joint Undertaking (www.imi.europa.eu) under Grant Agreement n° 115004, resources of which are composed of financial contribution from the European Union's Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution. 32 Click or scan me! http://www.imi-protect.eu/results.shtml# 33 Introducing the IMI “Get Real” project PSI Conference May 12-14 2014 Chrissie Fletcher, Amgen The research leading to these results has received support from the Innovative Medicines Initiative Joint Undertaking under grant agreement no [115303], resources of which are composed of financial contribution from the European Union’s Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution. www.imi.europa.eu Disclaimer • The views expressed herein represent those of the presenter and do not necessarily represent the views or practices of Amgen or the views of the general Pharmaceutical Industry. The research leading to these results has received support from the Innovative Medicines Initiative Joint Undertaking under grant agreement no [115303], resources of which are composed of financial contribution from the European Union’s Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution. www.imi.europa.eu Two problems needing a joint solution R&D decision • What combination of possible studies will provide the most valuable information to HTA/payers? • What is the feasibility of the study options pre-launch and what would be commitments post launch? • How do options reconcile with the regulatory process? HTA decision • Would we predict an improvement in patient outcome or care pathway efficiency over and above current practice in my healthcare? • Would we accept the uncertainty for a period of time while waiting for studies to complete? The research leading to these results has received support from the Innovative Medicines Initiative Joint Undertaking under grant agreement no [115303], resources of which are composed of financial contribution from the European Union’s Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution. www.imi.europa.eu Background and motivation 1. HTA / healthcare decision making require additional information to Regulatory to address the “efficacy – effectiveness” gap 2. Current initiatives on relative/comparative effectiveness research show how real world data can be harnessed post launch 3. There is an opportunity to adapt such techniques pre-launch... but there are practical issues – HTA <-> regulatory objectives – Ethical and legal obligations – Managing cost and operational feasibility 4. Integrating heterogeneous trial and observational data to inform predictive modelling of effectiveness requires new analytical techniques The research leading to these results has received support from the Innovative Medicines Initiative Joint Undertaking under grant agreement no [115303], resources of which are composed of financial contribution from the European Union’s Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution. www.imi.europa.eu 38 GetReal: Project Vision For pharmaceutical R&D and healthcare decision makers to better understand how real-world data and analytical techniques can be used to improve the relevance of knowledge generated during development, e.g., through innovation in clinical trial design. Lasting impact of the project To provide a methodological and analytical framework that informs policy and process evolution beyond the project and at an international level; and to provide tools, techniques and training that ensure that the potential of real world data can be exploited in drug development. The research leading to these results has received support from the Innovative Medicines Initiative Joint Undertaking under grant agreement no [115303], resources of which are composed of financial contribution from the European Union’s Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution. www.imi.europa.eu 39 39 Innovative Medicines Initiative: Joining Forces in the Healthcare Sector The research leading to these results has received support from the Innovative Medicines Initiative Joint Undertaking under grant agreement no [115303], resources of which are composed of financial contribution from the European Union’s Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution. www.imi.europa.eu Nat Med 2014;20:5. 41 The research leading to these results has received support from the Innovative Medicines Initiative Joint Undertaking under grant agreement no [115303], resources of which are composed of financial contribution from the European Union’s Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution. www.imi.europa.eu Nat Med 2014;20:5. 42 The research leading to these results has received support from the Innovative Medicines Initiative Joint Undertaking under grant agreement no [115303], resources of which are composed of financial contribution from the European Union’s Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution. www.imi.europa.eu Public/SME partners Universities, research organisations, public bodies, non-profit groups Universitair Medisch Centrum Utrecht, the Netherlands Academisch Ziekenhuis Groningen, the Netherlands College voor Zorgverzekeringen, the Netherlands European Medicines Agency, UK European Organisation for Research and Treatment of Cancer, Belgium Haute Autorité de Santé, France London School of Hygiene and Tropical Medicine, UK National Institute for Health and Care Excellence, UK Panepistimio Ioanninon, Greece Universität Bern, Switzerland University of Leicester, UK Small and medium-sized enterprises (SMEs) LA Santé Epidemiologie Evaluation et Recherche, France Patients’ organisations International Alliance of Patients' Organizations, UK The research leading to these results has received support from the Innovative Medicines Initiative Joint Undertaking under grant agreement no [115303], resources of which are composed of financial contribution from the European Union’s Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution. www.imi.europa.eu EFPIA partners GlaxoSmithKline Research and Development Amgen AstraZeneca Bayer Pharma Boehringer Ingelheim Bristol Myers Squibb Eli Lilly F. Hoffmann-La Roche Janssen Pharmaceutica Merck KGaA Merck Sharp & Dohme Corp. Novartis Pharma AG Novo Nordisk Sanofi-Aventis Takeda Development Centre The research leading to these results has received support from the Innovative Medicines Initiative Joint Undertaking under grant agreement no [115303], resources of which are composed of financial contribution from the European Union’s Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution. www.imi.europa.eu Structure and topics of GetReal WP3 WP1 WP2 WP3 WP2 WP3 Choice of comparator Innovative Development options / study designs WP2 Drivers of relative effectiveness III a options / study designs WP4 Operational cost/ feasibility / solutions Ethics & Regulations Full Evidence Integration Predictive Modelling WP4 Predictive power / residual uncertainty WP1 Frameworks of relative effectiveness assessment International Acceptable Reg & HTA uncertainty? policy implications The research leading to these results has received support from the Innovative Medicines Initiative Joint Undertaking under grant Reg + HTA Process Simulations agreement no [115303], resources of which are composed of financial contribution from the European Union’s Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution. www.imi.europa.eu WP1: The WP1 case study approach Development strategy redesign workshops Summaries Information Sources Workshop 1 Outputs Company Governance • Publicly available documents (reg, HTA) • Stakeholder interviews • Company commentaries & presentations • Original company source documents Simulations • Discussion summary / minutes • Key scientific questions (sources of bias and uncertainty in REff) • Alternative development design options Workshop 2 Outputs • Discussion summary / minutes • Stakeholder insight & reactions to potential options • Scenario Summary • Contribute to decision framework • Publications The research leading to these results has received support from the Innovative Medicines Initiative Joint Undertaking under grant agreement no [115303], resources of which are composed of financial contribution from the European Union’s Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution. www.imi.europa.eu Slide 46 WP 2: better understand the gap between efficacy & effectiveness Clinical trials (efficacy) Real world (effectiveness) The research leading to these results has received support from the Innovative Medicines Initiative Joint Undertaking under grant agreement no [115303], resources of which are composed of financial contribution from the European Union’s Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution. www.imi.europa.eu WP3: overcoming practical barriers in undertaking pre-launch RE research. The research leading to these results has received support from the Innovative Medicines Initiative Joint Undertaking under grant agreement no [115303], resources of which are composed of financial contribution from the European Union’s Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution. www.imi.europa.eu WP4: Promote best practice in evidence synthesis and predictive modelling The research leading to these results has received support from the Innovative Medicines Initiative Joint Undertaking under grant agreement no [115303], resources of which are composed of financial contribution from the European Union’s Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution. www.imi.europa.eu Developing a predictive model for relative effectiveness The research leading to these results has received support from the Innovative Medicines Initiative Joint Undertaking under grant agreement no [115303], resources of which are composed of financial contribution from the European Union’s Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution. www.imi.europa.eu 50 Project deliverables and benefits • Frameworks developed jointly by Regulatory, HTA and Industry experts for use in: • Practical Solutions to enable implementation of studies with greater value of information for relative effectiveness assessment • Advances in methodology to reliably predict effectiveness from available data • Aligning innovation in evidence generation with evolution of regulatory and HTA processes The research leading to these results has received support from the Innovative Medicines Initiative Joint Undertaking under grant agreement no [115303], resources of which are composed of financial contribution from the European Union’s Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution. www.imi.europa.eu 51 For more information: • Visit the GetReal website: imi-getreal.eu The research leading to these results has received support from the Innovative Medicines Initiative Joint Undertaking under grant agreement no [115303], resources of which are composed of financial contribution from the European Union’s Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution. www.imi.europa.eu