End of life care for people with advanced dementia

End of life care for people with advanced dementia - Bromley
Jo Hockley RN PhD MSc SCM
Nurse Consultant, Care Home Project Team
St Christopher's Hospice
BROMLEY
• Higher than average older population and 2,600 die each year
• Higher than average population with dementia mention dementia as a contributing cause of death
– 21% (national average 17.3%)
• Rates of hospital deaths in Bromley are around 56% with
36% of people dying in their own home/care home
• For patients cared for by St Christopher’s and Harris
Hospiscare:
– 20% in hospital and 55% dying at home/care home
– Care home (with nursing) deaths in Bromley have increased by 10% since St Christopher’s started implementing the Gold Standards
Framework.
Dementia progression: FAST staging
• 1 No functional decline
• 2 Personal awareness of some functional decline.
• 3 Noticeable deficits in demanding job situations.
• 4 Requires assistance in complicated tasks eg finances, planning dinner for guests etc
• 5a Cannot recall address, tel no, family members' names etc
• 5b Frequently some disorientation to time and place
• 5c Cannot do serial 4s from 40, or serial 2s from 20.
• 5d Retains many major facts re self
• 5e Knows own name
• 5f No assistance toileting, eating but may need assistance choosing proper attire
• 6a Difficulty putting clothes on properly without assistance
• 6b Unable to bathe properly eg adjusting water temperature.
• 6c Inability to handle mechanics of toileting eg forgets to flush, does not wipe properly.
• 6d Urinary incontinence
• 6e Faecal incontinence
• 7a Speech limited to about 6 words in an average day.
• 7b Intelligible vocabulary limited to single word on average day.
• 7c Cannot walk without assistance
• 7d Cannot sit up without assistance
• 7e Unable to smile
When is end of life reached for the person with dementia ?
Cancer Trajectory
Function
High
The Dementia Trajectory
Function
High
Death
Low
Time
Low
Time
Death
Where do people with dementia die?
Hospital
Old people’s home
Nursing home
Own home
Hospice
Elsewhere
Deaths from Alzheimer’s disease, dementia and senility in
England. National End of Life Intelligence Network
November 2010
Hospitalised patients with endstage dementia receive…
• More inappropriate interventions
• Less symptom management
• Fewer referrals for specialist palliative care
• Less recognition of their spiritual needs
• Families are asked to make decisions in times of crisis
(Morrison & Siu 2000; Sampson et al 2006)
Main symptoms at end of life for someone with dementia
(McCarthy and Addington Hall 1997)
• Pain ( 64% )
• Confusion ( 83% )
• Loss of appetite ( 57% ) and/or swallowing difficulties
• Low mood ( 61% )
• Incontinence- ( 72% ) pressure area risks
• Delirium
• Terminal agitation
• Excess secretions especially if has pneumonia
• Constipation
What are the challenges in EOLC for people with advanced dementia?
Professionals unskilled at symptom assessment where there is little communication from the resident/patient i.e. pain assessment
Poor recognition of dementia as a terminal illness
Failure to plan while the person has capacity
Difficulty in recognising the dying phase
Last minute panic leading to hospitalisation
Quality of life? Social and spiritual care?
An exploration of the palliative care needs of people with dementia & their families –
St Christopher’s Croydon Dementia Project
Dementia team was 1 FTE clinical nurse specialist. 0.2 medical consultant
FINDINGS:
• 121 patients taken on by the project team
• Pain was present in 98/121 patients at referral:
– mainly arthritis, contractures, pressure sores
– in all but 6 the pain was easy to control
• Common symptoms:
– drowsiness, weakness, anorexia, weight loss, dysphagia.
• Very little advance care planning had been done with families and decisions had not been made about resuscitation prior to involvement by the team
• 89% died in their usual place of residence/home/care home
CONCLUSION:
• Neglected group
• Most care could be managed by generalist health care providers (GP’s, DNs); however, not being achieved.
Looking
Ahead document
..documenting wishes and preferences in the event of a
‘best interest’ meeting for people with dementia.
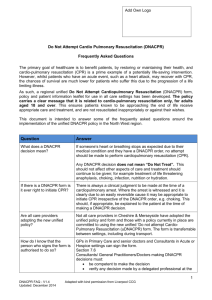
Liverpool Care Pathway
• LCP – m/disciplinary Care Plan
• Created to empower the generalist by Prof John
Ellershaw
• Goal orientated
• Three sections:
– Initial assessment
– 4hrly assessments
– 12hrly assessments
– Care after death
Liverpool Care Pathways leaflet
(St Christopher’s leaflet ‘13)
• What is the Liverpool Care Pathway (LCP)?
• Must the LCP be continued once started?
• Does the LCP make you give sedatives and other powerful drugs?
• Does the LCP stop a person having food or drink?
• Does the LCP ban drips?
• Since going on the LCP, medicines have been stopped and everything is given by injections. Why?
• Does the LCP make people die faster?
Comparison of data on DNaCPR; ACP & ICP – 2009 to 2012
Care Home Project Team, St Christopher’s, London
PCT 1 PCT 2 & 3 PCT 4 PCT 5 Total
DNaCPR:
2009/10
2010/11
2011/12
43% (n=155)
45% (n=218)
75% (n=214)
41% (n=265)
74% (n=329)
84% (n=284)
68% (n= 384)
75% (n= 435)
86% (n= 492)
54% (n=271)
71% (n=397)
76% (n=361)
52%
66%
80%
ACP:
2009/10
2010/11
2011/12
48% (n=155)
62% (n=218)
76% (n=214)
44% (n=265)
61% (n=329)
60% (n=284)
ICP for last days:
2009/10
2010/11
2011/12
33% (n=155)
59% (n=218)
70% (n=214)
5.5%(n=265)
30% (n=329)
51% (n=284)
60% (n= 384)
74% (n= 435)
83% (n=492)
51% (n=271)
63% (n=397)
79% (n=361)
44% (n=384)
60% (n= 435)
72% (n= 492)
17% (n=271)
37% (n=397)
59% (n=361)
51%
65%
75%
25%
47%
63%
Comparison of place of death across nursing homes
Care Home Project Team, St Christopher’s
Hospice [2007 to 2012]
2007/2008 2008/2009 2009/2010 2010/2011 2011/2011
Percentage of deaths occurring in NHs
[numbers of deaths]
57% 67% 72% 76% 78% n=324 deaths across
19 NHs n=989 deaths across
52 NHs n=1071 deaths across
53 NHs n=1375 deaths across
71 NHs n=1351 deaths across
71 NHs
Action Evaluation implementing Namaste in five nursing homes in SE
London –
Min Stacpoole & Jo Hockley
Cited by Alzheimer’s Society (2012)
‘My life until the end: dying well with dementia’
The Power
Of
Loving Touch
namastecare.com
NAMASTE CARE - KEY ELEMENTS
(Simard, 2013)
“Honouring the spirit within”
Sensory stimulation: 5 senses
Sight, touch, taste, hearing, smell
The presence of others
Meaningful activity
Life history
Comfort and pain management
Family meetings
Care of the dying and after death
Care staff education
Namaste family meetings (i)
Entry to Namaste triggers family meeting to open conversation about future plans around end of life
Seeks help of family “to honour the spirit within”
Life story – especially sensory triggers for reminiscence
Person’s likes & dislikes
e.g. favourite music
Namaste family meetings (ii)
Acknowledges disease progression early and in a positive context
Establishes comfort and pleasure as the aims of care
Opens conversation around DNACPR, hospitalisation, preferred place of death
Ultimate goal is peaceful, dignified death
BROMLEY END OF LIFE (EOL) CARE
PARTNERSHIP
6 weeks of personal care for discharges from PRUH or patients deemed to be in last year of life now + volunteer support
Bid into enablement board
PRUH
Palliative care team
PACE Team
Discharge Team
Community
Nursing
(Bromley
Health)
Multi visit personal care for continuing care patients (New) volunteer support
Future aspiration
Planned night care
(Marie Curie)
EOL Co-Ordination Centre
• Co-ordinates care
• All referred patients get an assessment visit
By a nurse
• Advance care planning
• Decision on keyworker
• Keeps CMC registering to date
• Administrates
• equipment
• 24/7
Mental
Health
Services
(Oxleas)
Nursing &
Residential care home programme
Co-ordination centre proposal being developed by the ProMise programme
Thank you
j.hockley@stchristophers.org.uk