Comp Present and Future 2014 Changes Including the 2013 Reform
STATE OF TENNESSEE
DIVISION OF WORKERS’ COMPENSATION
DEPARTMENT OF LABOR AND WORKFORCE DEVELOPMENT
220 FRENCH LANDING DRIVE
NASHVILLE, TENNESSEE 37243-1002
(615) 741-2395
1-800-332-2667
Workers’ Compensation
Present and Future
2014
Changes including the 2013 Reform
Act
Changes Go Into Effect
1 July, 2014
Causation
Administrative Judges
Permanent Impairment Ratings
Aggravation of Pre-existing Condition
MMI and Pain Management
Panel Rules
1 January, 2016
Treatment Guidelines
Changes Not Retroactive
practitioners, other providers, companies, attorneys, injured workers, adjusters, case managers, therapists, etc.
we will all have to live in two worlds, just like the transition from the 5 th edition to the 6 th edition
Meaning
The meaning and interpretation of these statutes and rules will be determined by the Judges, ultimately a legal and judicial decision.
This presentation is the guidance from the Medical
Director’s Office as of this time.
“ Liberal ” Construction
Now: in favor of the employee
“it happened at work, now I need treatment, therefore my employer should pay.”
Implications
designed as “no fault” temporary disability payments off work light duty job protection
New Construction
“fair and impartial” removed from county courts
Judges appointed by the Administrator of the Division
8 regional courts, when fully implemented administrative procedures
Causation(1)
Now: “in the course and scope of employment”
Except cumulative trauma disorders: rules for these changed in 2011
“primarily within the course and scope”
New: “primarily out of…and in the course and scope of employment…”
Causation(2)
Now: “…was it possibly caused by…?”
New: the employee must show…that the subsequent… need for treatment is “more likely than not” (greater than 50%), due to this injury,
“considering all causes, as opposed to speculation or possibility .”
Causation Opinion
Use of the physician’s opinion:
1. First visit-ER, Occupational Medicine.
2. First Referral: do not assume that the carrier has accepted the claim, even though they made the appointment.
3. Subsequent request for an opinion.
Panels
New: The opinion of the treating physician selected from the employer’s panel is presumed to be correct (causation).
The employer may present the employee with a panel of three physicians…
The employer has three days to object to a referral from one of the panel physicians and present the employee a different panel.
No particular requirements for subspecialty panels.
Injury
“An ‘injury’…means an injury by ‘accident’ that…arises primarily out of and in the course and scope of employment that causes death, disablement, or the need for treatment, provided that it is…caused by an incident, or series of incidents...identifiable by time and place of occurrence…”
Aggravation
“…and shall not include the aggravation of a pre-existing disease, condition or ailment, unless it can be shown to a reasonable degree of medical certainty that the aggravation arose primarily out of and in the course and scope of employment.”
Definitions
Aggravation: a permanent worsening (a condition made permanently worse) with documentable anatomic change.
Exacerbation: temporary with no anatomic change.
Opinion
Treating physician’s opinion is “…presumed to be correct…” if it is based upon a reasonable degree of medical certainty that the “injury” contributed “…more than 50%in causing...the need for medical treatment…more likely than not, considering all causes, as opposed to speculation or possibility .”
Aggravation
New: “J ust because your knee hurt after your
‘injury’ does not necessarily make it covered under Workers’ Compensation.”
Significant implications concerning: disability payments restricted duty off work time ability to “fire”
Exacerbation
No permanent anatomic change.
Temporary decrease in function: limitations (cannot), restrictions (should not).
Implications: limitations restrictions pain temporary disability
Judgment on Causation
Ultimately, the compensability of a claim lies with the Administrative Court.
Physicians’ opinions.
Timing of causation appeal.
Risk to the provider: treatment payment.
Risk to the employee: job.
Treating Physician(1)
Still must be the advocate for the patient.
More requirements for initial evaluation concerning likelihood of causation and relationship to work.
Not likely that a PA or NP can see a patient for the first visit if there is a causation question.
More information is going to be needed to satisfy the new questions about causation.
Treating Physician(2)
More careful questioning.
More careful documentation.
Document verbal communications.
New: Released from disclosure form (C-31).
Communications (all pertinent) to employer/carrier/adjuster/case manager will not be restricted.
MMI, PIR
Now: ‘should’ complete and “scheduled member”
New: The treating physician is required to give
MMI “..conclusively presumed to be at MMI when the treating physician ends all active medical treatment…” except “…treatment of pain …”
New: The permanent impairment rating “shall be assigned by the treating physician…” and is to be converted to “body as a whole.”
MMI(1)
“
a point in time…when further medical or surgical intervention cannot be expected to improve the underlying impairment …not predicated on the elimination of symptoms and/or subjective complaints…stable…or can be managed with palliative measures. MMI does not preclude the deterioration…that is expected to occur with the passage of time…or normal aging process…”
• AMA Guides, 6 th edition
MMI(2)
“…it does not preclude allowance for ongoing follow-up for optimal maintenance of the medical condition in question.”
• AMA guides, 6 th edition
“…patient may decline recommended treatment…or choose not to comply with recommended life style changes (weight reduction, smoking cessation)…physician may explain…and comment…”
• AMA Guides Newsletter: Brooks, 2014.
Pain
“…shall not consider complaints of pain in calculating the degree of impairment, notwithstanding allowances for pain provided by the applicable edition of the AMA guides…”
(50-6-204(k)(2).
“…is not entitled to a second opinion on…pain management.”
U/R after 90 days of any schedule II, III, IV.
referral to “pain specialist”
Guidance on Pain Ratings(1)
Ultimately the Judge’s Decision
This is not a causation statute. It is designed to remove some subjectivity from the rating process.
1. Do not use Chapter 3 or PDQ.
Very few circumstances.
2. In nerve injury, use sensory deficit as opposed to pain assessment.
Guidance on Pain Rating(2)
There are three grade modifiers: a. Physical Examination b. Clinical Studies c. Functional History
No change in first two.
Guidance on Pain Rating(3)
3. In the Functional History Grade Modifier:
Do not consider complaints of “pain” in using this modifier.
Use concepts such as limited motion or weakness in assessing functional abilities and limitations.
Guidance on Pain Ratings(4)
In the Upper Extremity and in the Spine Chapters:
4. If the diagnosis is non-specific chronic pain, such as wrist pain or neck pain, by definition there are no physical examination or clinical studies modifiers that apply.
Do not use the functional history modifier.
Use only the default value.
Treatment Guidelines
Effective January 1, 2016
“The Administrator shall develop…”
“…for the most commonly occurring…”
“…shall presumed to be medically necessary…and not subject to utilization review.”
Practice Guidelines
Treatment Guidelines
Institute of Medicine(2011)
“…statements that include recommendations intended to optimize patient care that are informed by a systematic review of the evidence and an assessment of the benefit and harms of alternative care options.”
Easily Accessible, user friendly
Reasonable acquisition and use cost
Potential Decisions
1) Most numbers of procedures
2) High cost-length of disability
(indemnity and medical)
3) Payment under “open medical”
Administrator decides.
(in consultation with the
Medical Advisory Committee)
Timeline look for preliminary announcement on the
Workers’ Compensation Website:
http://www.tn.gov/labor-wfd/wcomp/providers.shtml
Timeline(2)
First Guideline:
Management of Chronic Pain
Coordinating with the Department of Health:
http://health.tn.gov/Downloads/ChronicPainGuidelines.pdf
Other Topics
Medical Fee Schedule
ICD-10
MIRR
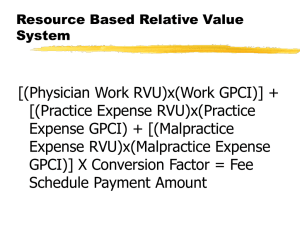
Medical Fee Schedule(1)
Adjustments made by CMS to conversion factors and RVUs January 1, 2014.
No change in the (combined) Tennessee conversion factor (GPCI, facility, etc) to calculate the RVUs, remains at 33.764. even though CMS raised the (combined)
Tennessee conversion factor but lowered some of the RVUs.
Medical Fee Schedule(2)
The conversion factor and the calculations were written into the rules (0800-02-18-.02(4)), so that if CMS reduced their conversion factors (SGR) below that level, the practitioners would not be affected without a hearing.
Effect of 2014 CMS RVU changes: orthopaedic impact (99204): -$10.00)
Medical Fee Schedule(3)
Tennessee-specific service (specialty) percentages unchanged
(Ortho-Neuro = 275%)
Calculation unchanged.
Since the Medical Fee Schedule follows CMS,
Watch for NCCI edits: new: shoulder bundles for 2014
ICD-10
The Division does not pay bills
It collects data and uses it for:
1. Case Management
2. Utilization Review
3. Benefits review and awards
4. Mediation
5. Compliance
6. Penalties
ICD-10
1. The Division of Workers’ Compensation is considering accepting the use of ICD-10 codes on all submissions for Date of Service (DOS) on of after 1
October, 2014.
2. It will not be necessary to convert codes from ICD-9 to ICD-10.
3. For the special circumstance where DOS includes before and after 1 October, 2014(5), such as an inpatient admission, the Division will accept either or both codes, in accordance with CMS guidelines.
4. As this issue in in flux, the Division has not made a determination yet. We are still gathering information.
Watch for further information on the web site.
MIRR
Medical Impairment Rating Registry
Function: independent review when an appeal is made by any party to a dispute about an impairment rating.
Stipulated before a hearing.
Recruiting.
Requirements: certification and review.
Reference List
Workers’ Compensation Law: http://www.lexisnexis.com/hottopics/tncode/
Rules: http://www.tn.gov/sos/rules/0800/0800-02/0800-
02.htm
Website: http://www.tn.gov/labor-wfd/wcomp/providers.shtml
Department of Health: http://health.tn.gov/Downloads/ChronicPain
Guidelines.pdf
Changes
“Nothing is constant except change”
-Heraclitus-
500BC.