Laurie A. Huryk RN, BSN - New Jersey Primary Care Association
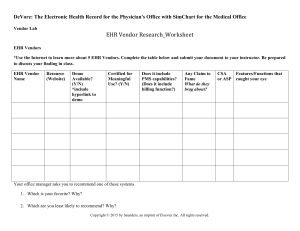
advertisement

Laurie A. Huryk RN, BSN VNACJ Community Health Center Family Medicine Residency Program at CentraState Cell phones: Please turn them off or set them to vibrate Questions: Please reserve your questions until the end of the presentation Determine the level of involvement end users should have in an IT project. Determine an acceptable level of decreased productivity throughout the development and implementation process. Provide appropriate support for end users post implementation. Modernize our nation’s infrastructure Enhance energy independence Expand educational opportunities Provide tax relief Preserve and improve affordable health care. Goal: Improve quality and value of American health care Method: Expanded use of health information technology (HIT) *2008 only 4% physician offices and 2% hospitals fully utilize Electronic Health Records (EHR) Plan: Accelerate the adoption of HIT HOW......? Eligible Providers and Hospitals who are Meaningful Users of certified HIT. Beginning with financial year 2011 and ending with financial year 2015. Penalties of reduced payments will begin in financial year 2015. Must use certified EHR technology in a meaningful manner Must be able to electronically exchange information from the certified EHR. Must submit clinical quality measures to the Secretary of the US Department of Health and Human Services. Systems that are fully functional but inadequate for meeting meaningful use requirements Systems that are not being used to their full potential Upgrades and core functionality modifications from the vendor Perceive problem with current process and believe that an improved process exists. The individual or group must be willing to learn the new process, and must feel safe in the learning environment. New process must be congruent with individual’s other tasks and responsibilities. User must be aware that an innovation exists and persuaded that the idea is beneficial. A conscious decision must be made to use the innovation. The user must be provided with feedback to verify that the new innovation is beneficial in order to sustain change. Innovators Early Adopters Early Majority Late Majority Laggards Retrieved from http://en.wikipedia.org/wiki/File:Diffusionofideas.PNG Reduction in medical errors Expert support for clinical decisions Reduction in re-hospitalization Ability to reach rural patients Access to experts around the clock Consistency in documentation Portability and redundancy of medical records Ability to create and maintain a complete patient centered health record Enhanced reporting capabilities Improved patient follow-up Where is the evidence? Longhurst, C. A., Parast, L., Sandborg, C. I., Widen, E., Sullivan, J., Hahn, J. S., … Sharek, P. J. (2010). Decrease in hospital-wide mortality rate after implementation of a commercially sold computerized physician order entry system. Pediatrics. Advance online publication. doi: 10.1542/peds.2009-3271 Poon, E. G., Keohane, C. A., Yoon, C. E., Ditmore, M., Bane, A., Levtzion-Korach, O., … Gandhi, T. K. (2010). Effect of bar-coded technology on the safety of medication administration. New England Journal of Medicine, 362(18), 1698-1707. Chumbler, N. R., Haggstrom, D. A., & Saleem, J. (2010). Implementation of health information technology in veterans health administration to support transformational change: Telehealth and personal health records. Medical Care 48(12), Advance online publication. Evidence-based practice Diligent healthcare providers Improved quality through focusing on chronic conditions and other factors The potential is unimaginable with paper processes. Identify innovators Designate specific meeting times Develop timeline for project Purpose: Allow IT staff the opportunity to understand the workflow requirements of clinical operations. Methods: Individual key IT personnel observe patient encounter through entire visit cycle current documentation processes of clinical staff current system report usage Purpose: To familiarize IT staff with current forms so that new system may be analyzed for congruency with documentation requirements and formatting may be customized to be similar to current forms whenever possible. Method: IT staff members will analyze clinical documentation forms external forms (i.e. referral forms for particular programs) reports compiled under current system Purpose: Allow clinical staff the opportunity to further explain and clarify workflow and documentation needs and to offer suggestions for process improvement that may be incorporated into the new system. Method: IT Analyst will interview clinical staff members administrators clerical staff Thorough testing done in stages Involve all staff, not just committee members Be prepared to rework some components of system Encourage constructive criticism Onsite vendor support Onsite super–user support Method depends upon comfort level of provider Plan on decreased productivity Emergencies only Six month rule Utilize the IT Committee Thoroughly test all changes Train all users on changes Super-users Continuing education IT department Vendor support IT Committee Required changes to system Standards of care Medications Vaccines Patient education documents Electronic features Electronic standards ENHANCEMENT REQUEST FORM NAME: ______________________________ PHONE: ___________________________ DATE: _______________ TEMPLATE REQUEST DOCUMENT REQUEST REPORT REQUEST DETAILED DESCRIPTION OF ENHANCEMENT REQUEST ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ______________________________________________________________________ Implementing an EHR is a big investment. Including your staff and physicians throughout the planning, development, and implementation processes and providing adequate support post “go-live” enhances the probability of success. Leiber, H. S. (2009). Overview of the American Recovery and Reinvestment Act of 2009. Powerpoint presentation from a virtual conference of the Health Information Management Systems Society. Retrieved May 1, 2009 from http://www.himss.org/. Lewin, Kurt (1997). Resolving social conflict/ Field theory in social science. Washington, D.C.: American Psychological Association. McGonigle, D., & Mastrian, K. (2009). Nursing Informatics and the Foundation of Knowledge. Sudbury, MA: Jones and Bartlett Publishers. Medicare and Medicaid Programs; Electronic Health Record Incentive Program; Proposed Rule, 75 Fed. Reg . (proposed Jan. 13, 2010) (to be codified at 45 C.F.R. pt. 412, 413, 422, and 495). Rogers, E. M. (2003). Diffusion of innovations (5th ed.). New York: Simon & Schuster. Schein, E. H. (1996). Kurt Lewin’s change theory in the field and in the classroom: Notes toward a model of managed learning. Systemic Practice and Action Research 9(1), 27-47. Shelly, G. B., & Rosenblatt, H. J. (2010). Systems analysis and Design (8th Ed.). Boston, MA: Course Technology, Cengage Learning. U.S. Department of Health and Human Services. Health IT Adoption Initiative. Retrieved June 11, 2009 fromhttp://healthit.hhs.gov/portal/server.pt?open=512&objID=1152&parentname=Comm unityPage&parentid=11&mode=2&in_hi_userid=10741&cached=true To be published in the Journal of Nursing Management within the next 6 months.