Clement 2014
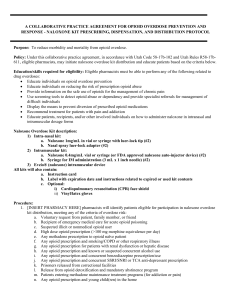
advertisement

Presenters: Cassandra Clement, Pharm.D., BCPS Orlando VA Medical Center Orlando, Florida Chris Stock, Pharm.D., BCPP George E. Wahlen Department of Veterans Affairs Medical Center Salt Lake City, Utah IRB Status: Exempt Status Approved Co-investigators: Christopher Stock, Pharm.D., BCPP Conflicts of Interest: None Project Sponsorship: None Also referred to as Salt Lake City Veterans Affairs Medical Center (SLC VAMC) 121 bed hospital 9 Community-Based Outpatient Clinics Average 64 ED visits per day Serves > 50,000 veterans Opioid overdose deaths continue to be an increasing problem throughout the United States and within Utah.1 Utah is the eighth highest drug overdose mortality rate in the United States (16.9 per 100,000) Some of the risk factors for overdoses have been delineated.3,4 Age • Middle-aged (overdose death) • Young or elderly (overdose) White race Medical diagnoses • Chronic or acute pain (versus pain due to cancer) • Sleep Apnea • Morbid obesity • Preexisting pulmonary or cardiac disease or dysfunction or major organ failure Psychiatric diagnoses • Substance use disorders • Psychiatric disorders Medications • Opioid dose • >50mg, >100mg, and >200mg morphine equivalents • CNS depressants (i.e. anxiolytics, sedatives) 1.Prescription Drug Abuse: Strategies to Stop the Epidemic. Trust for America's Health. October 2013. 2.ASB Bohnert et al. Unintentional overdose and suicide among substance users: A review of overlap and risk factors. Drug and Alcohol Dependence 110 (2010) 183–192. 3.Safe use of opioids in hospitals. The Joint Commission. Sentinel Event Alert. Issue 49, August 8, 2012. 4.ASB Bohnert, et. Al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA, 2011. The veteran population has nearly twice the rate of fatal accidental poisoning compared with adults in the general US population Opioid medications and cocaine were frequently mentioned as the agents causing poisoning on death records More detailed information about veterans experiencing overdose would help to tailor preventative efforts in this population. 1.ASB Bohnert, et. al Accidental Poisoning Mortality Among Patients in the Department of Veterans Affairs Health System. Med Care 2011;49: 393–396. 2.ASB Bohnert, et. al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA, 2011. 3.Gomes T, et al. Opioid Dose and Drug-Related Mortality in Patients With Nonmalignant Pain. Arch Intern Med. 2011;171(7):686-691. To describe veterans who received naloxone rescue therapy for opioid overdose and identify risk factors within this population such as: Demographic information Diagnoses Prescription accessibility of opioids and benzodiazepines on the day of and within 120 days of naloxone rescue therapy Urine drug screen results within 120 days of naloxone recue therapy Data collection Extracted from the VA Data Warehouse Retrospective open chart review Reviewed veterans who received naloxone rescue therapy at the SLC VAMC emergency department (ED) for opioid overdose between 1/1/2009 and 1/1/2013 Tabulations were made using Microsoft® Excel Information collected: Naloxone rescue therapy (ED visit date) Demographic information Diagnoses Sleep apnea, sleep disorders, obesity, cardiac disease, pulmonary disease, mental health diagnoses, and/or substance use disorder Prescriptions accessibility within 120 days and on the day of the ED visit: Morphine equivalents daily (MED) Lorazepam equivalents daily (LED) Urine drug screen (UDS) results Visits stratified by accessibility to: Opioids (OPs) only Benzodiazepines (BZs) only OPs & BZs No OPs or BZs Non-VA documented prescriptions only Day of naloxone therapy Within 120 days prior to naloxone therapy 170 veterans received naloxone 92 Indication: OP overdose 39 0 28 19 6 OP only BZ only OP & BZ No OP or BZ Non-VA only 34 4 19 19 6 OP only BZ only OP & BZ No OP or BZ Non-VA only Opioid MED (mg)4 Codeine Fentanyl Hydrocodone Hydromorphone Methadone Oxycodone Tramadol 0.15 3600 1 4 4.5 1.5 0.2 Accessibility within 120 days of rescue therapy (n=92) Accessibility on day of rescue therapy (n=82) Benzodiazepine LED (mg)5 Alprazolam Clonazepam Diazepam Lorazepam Temazepam 0.5 0.25 5 1 5 4. Washington State Agency Medical Directors' Group Second Reference. Online Available: http://agencymeddirectors.wa.gov 5. Lexi-Comp OnlineTM , Benzodiazepine Comparison Table, Hudson, Ohio: Lexi-Comp, Inc.; April 16, 2014. Opioid daily dose accessible within 120 days of ED visit 900 p value = 0.015 Max = 830mg 800 700 MED (mg) 600 500 Max = 525mg 400 300 Average 259mg 200 100 Average 118mg 0 OP Only Min = 7.5mg Min = 15mg OP & BZ Opioid daily doses accessible on the day of ED visit 900 800 Max = 830mg p value = 0.283 700 Max = 650mg MED (mg) 600 500 400 300 Average 183mg 200 100 0 Average 126mg OP Only Min = 20mg Min = 7.5mg OP & BZ Characteristic OP only (n=34) OP and BZ (n=19) No OP or BZ (n=19) BZ only (n=4) Non-VA OP (n=6) Mean Age (yrs) 64.4 56.4 62.5 51 75.2 p=0.08 Average days from last OP prescription pick-up 19 21 n/a n/a n/a Weekend ED visit 32% 44% 21% 0% 0% Other person lives at same address 84% 37% 26% 25% 33% Characteristic OP only (n=34) OP and BZ (n=19) No OP or BZ (n=19) BZ only (n=4) Non-VA OP (n=6) Had > 1 UDS within 120 days 60% 84% 63% 75% 33% UDSs reflective of prescribed regimens 40% 42% 21% 0% 17% MED difference of those who has reflective UDS vs. non-reflective 4.2mg* 44mg* n/a n/a n/a p > 0.5 p > 0.5 Characteristic OP only (n=34) OP and BZ No OP or (n=19) BZ (n=19) BZ only (n=4) Non-VA OP (n=6) Total (N=82) Morbid obesity 9% 26% 5% 25% 33% 15% Sleep apnea 47% 42% 11% 50% 33% 37% Sleep disorder 3% 11% 5% 0% 50% 9% CV disorder 91% 90% 63% 75% 100% 84% COPD 65% 53% 37% 50% 50% 54% Cancer 56% 42% 32% 25% 67% 46% Psychiatric disorder 74% 89% 79% 100% 50% 78% CV disorder > Psychiatric disorder > SUD > COPD > Cancer > Sleep apnea > Morbid obesity Characteristic OP only (n=34) OP and BZ (n=19) No OP or BZ (n=19) BZ only (n=4) Non-VA OP (n=6) Tobacco UD 21% 26% 11% 50% 0% Alcohol UD 26% 11% 16% 0% 0% Sedative UD 0% 0% 5% 0% 0% Opioid UD 0% 0% 0% 0% 0% • 54 veterans (58.7%) had a substance use disorder (SUD) • None of the veterans had a history of opioid use disorder or dependence CV disorder > Psychiatric disorder > SUD > COPD > Cancer > Sleep apnea > Morbid obesity Demographic Information The average age in our sample was 62, which is consistent with literature regarding age risk factors. Prescribed Medications The ED visit date was not immediately proximate to the last OP prescription pick-up date VA’s current opioid safety guidelines6 target > 200mg MED as the “high risk” dose but this would not capture most of the veterans in the OP only group. Veterans prescribed OPs & BZs concomitantly constitutes 23% of those who required naloxone rescue therapy. VHA Memorandum April 2, 2014. Comorbidities Cardiovascular diagnoses and psychiatric disorders were more prevalent than SUD, which is not consistent with previously published risk factor literature. Urine Drug Screens 68% of veterans prescribed OPs and/or BZs had no documented UDSs within 120 days prior to the ED visit date 58% of the UDSs were not reflective of prescribed regimens which may indicate many veterans have aberrant behaviors which are associated with overdose risk VHA Memorandum April 2, 2014. Contact Information: Cassandra Clement, Pharm.D., BCPS cassandra.clement@va.gov Christopher Stock, Pharm.D., BCPP christopher.stock@va.gov