The Process for Prescribing for Minor Ailments
advertisement

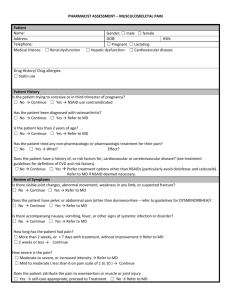
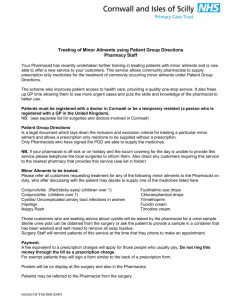
Jane Gillis B.Sc.(Pharm), Pharm.D. Disclosure I have no real or potential conflicts of interest to disclose. Minor Ailment Prescribing How do I fit this into my already busy workflow? How long does this take? Will patients pay? Will there be a demand for this service? How does this “fit” into the delivery of health care in NS? Do I have the knowledge to do this? What will physician’s think? How is this different from what we do already when recommending OTCs? Evaluation of the Provision of Minor Ailment Services in the Pharmacy Setting Pilot Study Q: What are the measurable benefits of pharmacists lead minor ailment services to patient, the pharmacy and the health system as a whole? Evidence to help • Support the implementation of these service • Demonstrate the value of these service • Educate public and other health care providers of the role of the pharmacist Study Timeline • January & February – study design and background • • • • research March –pharmacy recruitment (27) April & May – study set-up and preparation May 21- Aug 16 –study duration Aug 16- Sept 30 – data evaluation Study implementation Geographic Distribution of Participating Pharmacies 52% independent/banner : 48% large chain 52% urban : 48% rural Pharmacy Preparation and Support • Training and orientation session • Documentation and data collection materials (study protocol) • Website and online forum • Including access to online references • Promotional material – public/physician • Regular teleconferences and access to research team for help Preparation: Review therapeutics and assessment knowledge • Identify the minor ailments you are comfortable addressing • Identify resources available • Discuss with colleagues • Review your provincial standards and requirements • Documentations • Consent • Additional training • Other requirements Why should pharmacists prescribe? • Minor Ailment assessment is within a pharmacist’s area of expertise: • Pharmacists are generally under-utilized • Recognized by regulations in Nova Scotia for all pharmacists • Minor ailments are usually non-emergent • Appropriate use of sometimes limited resources • Pharmacists are able to assess whether treatment would be beneficial – either OTC or prescription OR when to refer to a MD because of red flags • Helps make sure people are seeing the doctor who may have otherwise gone without medical care • Helps make sure the right people are seeing the doctor Access to Care Sooner • 96% of respondents said the service helped them gain access to care sooner Where would you have gone if this service was not available? n=58, 10% n=26, 4% n=51, 9% Your family physician Walk-in clinic Emergency room Other Sought no help n=116, 20% n=335, 57% “Allowing pharmacists to treat minor ailments will provide patients with faster, high quality care without compromising patient safety.” Ryan R. Persuad, Pharmacy Student-Manitoba , Pers J RP The Process of Minor Ailment Prescribing Identify patient’s needs Explain the process Obtain consent Establish the environment Conduct an appropriate detailed assessment Recommendation 1. 2. 3. 4. 5. 6. • • Write the prescription, OTC recommendation or refer Joint decision making Establish monitoring parameters and plan Notify primary care provider Complete follow-up 7. 8. 9. • Notify primary care giver again – if necessary 10. Document and maintain documentation 1. Identify the Patient’s needs • Patients will either: • Self identify OR • Be identified by a pharmacist 52% self-referred 43% pharmacist recruited 2% MD referred 4% other Comparison OTC recommendation • Semi private • Quick assessment • OTC Product recommendation or referral • No (minimal) follow up • No (minimal) documentation • No (minimal) communication with primary care giver Minor Ailment Prescribing • Private • Semi-detailed assessment • OTC, Prescription written +/- dispensed or referral • Follow-up • Documentation • Communication with primary care giver Prescription or OTC??? Quickly figure out: What are they trying to treat? (i.e. is it a minor aliment) What was already tried? When? And did it work? Is a minor ailment assessment appropriate? Outcome of Assessment 2. Explain the process • As a pharmacist, I am able to prescribe medications such as (specific medication/ medication category) for (specific condition). • We would need to sit down in private for about 10-15 minutes. • Your input is important so we are able to determine the best course of action for you, which may involve a prescription therapy. Study findings • 1002 patients • Evenly distributed independent/chair AND uran/rural (approx 50:50) • Per store recruitment range 11-87 patients • 64% female • Bulk 19-65 yo Facilitating factors: no cost to patient; lack of access to MDs, marketing material from PANS, online resources, whole team approach, and “it got easier the more you did”. All pharmacy staff have a role! THE HAND OFF: The patient agrees- consider hand off to the Pharmacy Assistant to (1) obtain consent and (2) collect/reconcile medication history and allergies Good chance to refresh knowledge and get papers organized. It was really helpful to have the technicians involved, so the technicians could explain what the minor ailment assessment was, and how the pharmacist could do it. And they could also take some of the history, so it helped to decrease the time once you got into the counselling room to do the assessment. We’re constantly talking about it every day throughout the day, and it’s a reminder to our pharmacy cashiers or to our technicians, FYI, we’re looking for a minor ailment today. 3. Obtain Consent Guidelines in provincial standards. In NS patients must agree to: • the pharmacist completing an assessment • prescription therapy if appropriate as well as authorization to dispense the medication • the pharmacist communicating with other health care providers for information as required and to notify their primary care giver of the prescription and any follow-up results • the pharmacist monitoring therapy • the pharmacist maintaining documentation required by law NSCP Standards of Practice: Prescribing of Drugs by Pharmacists 24 Must also be Noted here 4. Establish the Environment • Make sure the room/counselling area is • professional (looks like a consult room not a broom closet) • clutter free • private 5. Conduct an Assessment (or confirm patient’s self-diagnosis) • Confirm contact info, medications, medical conditions and allergies • Symptoms • Objective and Subjective, physical findings if applicable • Duration and severity? • Recurrent vs new? Presence of risk factors? • What was tried for treatment? • Any red flags? • Drugs, medical conditions, severe or inconsistent sx, etc Pharmacists Resources- feedback from PhCs • We really appreciated the subscription to e-Therapeutics Complete. • The Saskatchewan guidelines were a good starting point, for sure, just to help you feel comfortable initially prescribing. • I’ve been out for 20 years, and I find it very helpful . . . I think for people who have any reluctance at all to undertake prescribing and feel like, oh well, I’ve been dispensing for so long, how do I step out of the dispensing, and how do I move into more of a clinical perspective? Having those simple tools will really make it easier, so I think that would be valuable. • They [treatment algorithms] really limit you though, while they’re great to have, it really locks you in to particular drugs and particular questions. 6. Make the recommendation • Pharmacist should create a shared decision making environment • Involve the patient in the decision making • Pharmacists will likely be required to write and sign if a prescription is written • Patients are not required to have it filled in your dispensary • Review non-pharm recommendations and medication information when prescribing • Referral is just as important as an outcome!! Minor Ailments Assessed Smoking Cessation Warts (excluding facial and genital) Nausea Nasal Congestion Mild Headache Dandruff Calluses and Corns Dysmenorrhea Non-infectious Diarrhea Cough Sore Throat Threadworms and Pinworms Impetigo Minor Sleep Disorders Mild Acne Xerophthalmia (dry eyes) Oral Ulcers Hemorrhoids Oral Fungal Infection (thrush) Minor Muscle Pain Mild Urticaria (including bites and stings) Contact Allergic Dermatitis Vaginal Candidiasis Gastro-ecophageal Reflux Disease Fungal Infections of the Skin Mild to Moderate Eczema Allergic Rhinitis Herpes Simplex n=1, 0.1% n=2, 0.2% n=2, 0.2% n=2, 0.2% n=2, 0.2% n=3, 0.3% n=3, 0.3% n=4, 0.4% n=5, 0.5% n=5, 0.5% n=8, 0.8% n=10, 1.0% n=17, 1.7% n=20, 2.0% n=26, 2.6% n=32, 3.2% n=39, 3.9% n=43, 4.3% n=48, 4.8% n=56, 5.6% n=56, 5.6% n=58, 5.8% n=59, 5.9% n=60, 6.0% n=62, 6.2% n=63, 6.3% Average time of assessment : 15 minutes n=149, 14.9% n= 167, 16.7% 0 20 40 60 80 100 120 140 160 180 7. Establish Monitoring Parameters and Plan Identify: • Therapeutic goal or outcome (WHAT is monitored and WHEN goal should be reached) • Should be measurable • Monitoring process (WHO will monitor) • Patient communication requirements (WHAT to do IF….) • Follow up date • Who is responsible for follow-up 8. Notify Primary Care Provider • This can be done with a form (may be provided as part of the provincial standards) • Communicate: • Patient information • Prescription information (date, details, rational and communication/instructions) • Follow-up plan • Pharmacist information 32 9. Complete Follow-up Determine process to pre-book follow-up • Calendar (Outlook) • Pharmacy Software • iphone, blackberry device Best if there was a reminder…. • Alarm • Print report every morning Average time for follow-up: 5 minutes; 89% report problem resolved 10. Document Documentation is a must – standards may vary from province to province but should include: • General patient information and documentation of consent • Assessment findings • Prescribing decision and rationale • Instructions given to patient • Monitoring plan • Information to allow other pharmacist to provide continuing care • Date and method of notifying primary health care provider • Follow-up notes (date and what was discussed/outcomes) Preparation Team Engagement • Everyone has a role • Pharmacists • Pharmacy Assistants • Others who work in the pharmacy • Think about your work flow – how do you incorporate this into a busy dispensary • Create awareness – talk it up! • Collaborate with other health care providers Workflow –what helped with implementation? • Change patient expectations • Being organized (materials ready to go) • Pharmacy technician involvement • Adding the assessment to the regular workflow – queued with Rx It was still identified as one of the largest barriers – especially pharmacies without PhC overlap Pharmacist Confidence “The ease at which it was integrated into the regular workflow routine at our store was great. At first, there was a bit of hesitation as to how we’re going to do this, you know, especially at times that didn’t have much overlap. But we quickly found that it can be very easily integrated into workflow routine, the identification, the performing of the assessments with great positive feedback from the patients. The more you did, the easier it got.” What did patients think? • 59% of participants completed and submitted a survey How beneficial was the Minor Ailment Assessment Service? Not Beneficial 0%, n=1 Neutral 1%, n=4 Somewhat Beneficial 99% said they would use the service again! 3%, n=18 Beneficial 17%, n=98 Very Beneficial 79%, n=464 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% Patient feedback (qualitative) • They recognized the value of the service • They appreciated that it was very accessible, fast and convenient • Many said it was their only option for immediate care • Patient’s valued the pharmacist’s skills and knowledge and trusted them as health care providers “I was really thrilled with this as it was an ailment that I had before and knew how well the Rx worked. It was going to take ages to see my family doctor and a large piece out of my day for a non-life-threatening illness that nevertheless makes me completely miserable.” Patient’s ability to pay • 30% said they WOULD NOT pay out of pocket • Two tiered health care – should be covered • Fixed or low income – should be provided by provincial medical insurance • They would just wait and go to the doctor where it is free • 70% said they WOULD be willing to pay for the service • On average $18.95 (range $3 -$120) Two closing thoughts from patients: “Awesome program. Wonderful service that will free up physicians to deal with more serious matters.” “This is a brilliant service. A step in the right direction for our health care system.”