Scott Barlow, MBA CEO - Governor`s Health Summit
advertisement

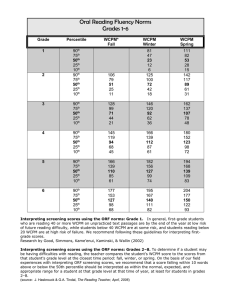
Early Lessons from an Accountable Care Organization Scott D. Barlow Chief Executive Officer September 30, 2014 1 Central Utah Clinic • • • • • • • Founded in 1969, largest independent medical group in Utah. Operate 101 offices - Utah, Mesquite NV and Paige, AZ. Currently employ over 1,400 professionals and staff. Medical staff of 170+ physicians, 100+ midlevel providers. Completely paperless in all care locations since 2002. Certified Medicare quality reporting registry. Participating in the Medicare Accountable Care MSSP program and five other commercial value based pilots. 2 Operational Flows • • • • • • Improving the reliability, safety and value of care is about designing consistent operational flows - logistics. An EHR is a tool to help create consistent designs, but is not itself an answer. Data sets mineable, relevant and actionable. “HPN” – provider/system competency, manageable. Sustained improvement does not rely on “I’ll remember to do it the next time”, or hard work. Design operational flows so the care we should provide happens every time. 3 Primary Care Report Card Cardiology Report Card MSSP Program Projections as of June 30, 2014 N = 14,000 Meeting all 32 Quality Metrics. 8 Payer 2 – NCQA Quality Scores Clinical Service Gen. Pop. Percentile Target Pop. Percentile Medicare Patients: n=347 Breast Cancer Screening COL Screening CMC – LDL Screening CDC – LDL Screening CDC – Eye Exam CDC – Kidney Disease Monitor CDC A1C Test 50th 25th <10th 10th 25th 10th 50th 90th 50th 90th 10th 25th 50th 75th Commercial Patients: n=3,041 Breast Cancer Screening COL Screening CMC – LDL Screening CDC – LDL Screening CDC – Eye Exam CDC – Kidney Disease Monitor CDC A1C Test 75th 50th <10th <10th 25th <10th 25th 90th 90th <10th 10th 50th 25th <10th 9 Payer 3 - Quality Measures • Population = 2,300 • Overall measures remained unchanged 2012 to 2013. • Satisfaction survey scores improved: 3Q = 87% 4Q = 94% • Population = 89% Readmission rate (50% GI Diagnosis): Regular pop. = 14% Participating pop. = 8% Savings generated above expected $986,724 Savings $429 per member Bonus Earned 10 CY 2013 vs. CY 2012 Clinic Utilization Improvement over Benchmark Change in Utilization/1000 Members Util/1000 INPATIENT FACILITY Surgical Medical, Non-Maternity Maternity Total IP Facility OUTPATIENT FACILITY Surgical Emergency Room Rad/Pathology Other OP Facilty Total OP Facility % Total Spend 20.0% -42.1% 4.3% -12.9% days 3.6% days 17.1% days 2.6% days 23.3% -9.2% -4.8% -3.9% -8.0% -6.4% cases 9.6% cases 4.8% cases 4.2% cases 9.2% cases 27.9% Util/1000 % Total Spend PROFESSIONAL IP Professional OP Surgical Professional PCP/Preventive Rad/Pathology All Other Professional Total Professional -12.6% -3.1% -5.5% -1.8% 3.4% -1.4% RX/OTHER Prescription Drugs Other Medical Benefits Ancillary Benefits -4.0% scripts -6.6% units -30.5% units TOTAL MEDICAL • • • Payer 3 - Impact -3.1% proc. proc. visits proc. visits 3.0% 4.3% 7.0% 4.3% 12.3% 30.9% 14.8% 2.8% 0.3% 100.0% Data shows change in CY2013 vs .CY2012. Paid claims run-out through March 2014. Utilization is on a risk-adjusted basis. Observed trends can reflect many variables other than Program Impacts, random fluctuation and utilization changes due to other programs 11 Payer 4 • N = 1,900 + 3,050 commercial • No bi-directional data feed. • Savings 7.8% of expected. • Shared savings earned • Missed quality targets so no payment. 12 Payer 5 N = 1,100 Measurement: PPO HMO Admits per 1,000 TARGET 213.4 189 166.8 189 ER per 1,000 TARGET 345.1 305 272.1 305 Readmit Rate TARGET 8.41% 11.3% 16.13% 11.3% Bonus Earned = 2.3% of total claims costs saved! 13 Payer 6 • • N = 11,300 Quality Measures: Total Cost of Care – MET BP Control of those with Hypertension – MET Cholesterol management, Cardiac patients – NOT MET Bonus Earned 14 Challenges • Patient attribution – who is accountable for whom? Medicare claims review 1.79M beneficiaries: Beneficiaries saw a median of 2 PCP & 5 Specialists. Median level of 4 different entities or practices. Median of 35% of PCP visits with their attributed PCP. (“Care Patterns in Medicare and Their Implications for Pay for Performance”, NEJM, March 15, 2007) (JAMA Internal Medicine, April 2014 – 145 ACO’s attribution, one-third switched 2010 to 2011) • Past care challenges: Review period, SNF or Consulting Care, Validate and refresh process. 15 Challenges • • • • • • • • • • Patient attribution – who is accountable for whom? Start with key partners (willing, capable, critical mass) – system of care – LOGISTICS! Data value – complete costs, mineable to the provider and patient. Data exchange to be bi-directional – 60%+ data missing. Relevant data – complete, variation amongst peers, timely. Golden Few – Care Management, Care Transitions. Risk Stratification – Coding intelligence. Patient & Family involvement/engagement? Set and manage to targets – quality, budgets “VALUE”. Maintaining the model? Improvements become new target?16 Lessons Learned • • • • • • • Aligning the interests of the payers, patients and providers can improve Quality & Costs. Models of success require a Holistic patient focus. Providing enhanced information enables better care. Need to start with a limited cohort of Providers. Need critical mass to be a “system of care”. Programs will be different, but need to be consistent and relevant to the care model. We can improve the system of care! 17 Questions? sbarlow@centralutahclinic.com 801-429-8034 18