IBD: What drugs in what patients?
Stephen B. Hanauer, MD
Professor of Medicine
Feinberg School of Medicine
Medical Director, Digestive Health Center
Northwestern Medicine
Conflicts
AbbVie, Actavis, Janssen, Pfizer,
Prometheus, Salix, Shire, Takeda, UCB
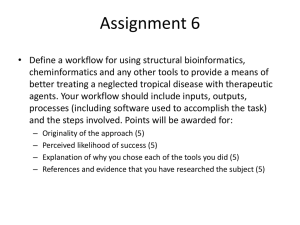
IBD in 2014: Therapeutic Goals
• Rapid and safe induction of remission
Absence of inflammatory symptoms
Normalized laboratory results
Healing of the bowel
Patient feeling healthy and well
• Corticosteroid-free durable maintenance of remission
• Restoration of growth and development; correction of malnutrition
• Avoidance of drug-related and disease-related complications
Kornbluth A, et al. Am J Gastroenterol. 2010;105:501-523; Lichtenstein GR, et al.
Am J Gastroenterol. 2009;104:465-483.
2
IBD in 2014: Medical Therapy Options
• Aminosalicylates
• Corticosteroids
Mesalamine
Balsalazide (UC)
Olsalazine (UC)
Sulfasalazine
• Immunomodulators
Azathioprine
6-mercaptopurine
Cyclosporine (UC)
Methotrexate (CD)
Budesonide
Systemic
• Biologics
TNF-α inhibitors
•
•
•
•
Adalimumab
Certolizumab pegol (CD)
Golimumab (UC)
Infliximab
Anti-integrin
•
•
Natalizumab
vedolizumab
Classification of UC Severity
FULMINANT
SEVERE
• >6 bloody
stools/day
MODERATE • Fever
• ≥4 stools/day • Tachycardia
± blood
• Anemia or
•
Minimal
signs
MILD
ESR
of
toxicity
• <4 stools/day
± blood
• Normal ESR
• No signs of
toxicity
•
•
•
•
>10 stools/day
Continuous bleeding
Toxicity
Abdominal
tenderness/distension
• Transfusion requirement
• Colonic dilation on x-ray
Truelove SC, Witts LJ. Br Med J. 1955;2:1041.
Kornbluth A, Sachar DB. Am J Gastroenterol. 2010;105:501.
Sequential Therapies for Ulcerative Colitis
Disease Severity
at Presentation
Anti-TNF +/IS
Anti-Integrin
Severe
Corticosteroid
Cyclosporine
Colectomy
Anti-TNF/
Thiopurine
Anti-Integrin
Aminosalicylate/
Thiopurine
Moderate
Aminosalicylate
Aminosalicylate
Oral/Topical/Combo
Oral/Topical/Combo
Budesonide
Induction
Maintenance
Mild
Therapy is stepped up according to severity at presentation or failure at prior step
Sequential Therapies for Crohn’s Disease
Disease Severity
at Presentation
Surgery
Anti-TNF +/IS
Anti-Integrin
Severe
Corticosteroid
Anti-TNF/
Thiopurine
Anti-Integrin
Thiopurine/
Methotrexate
Moderate
Budesonide
(Aminosalicylate)
Budesonide/
Thiopurine
Induction
Maintenance
Mild
Therapy is stepped up according to severity at presentation or failure at prior step
5-ASA Agents: Sites of Delivery
Colon
• Sulfasalazine
• Olsalazine
• Balsalazide
Terminal Ileum
Colon
(release at pH 7)
• Delayed release
mesalamine
• MMX mesalamine
Terminal Ileum
Colon
(release at pH 6)
• Granulated
mesalamine
Duodenum
Ileum
Colon
• Controlled
release
mesalamine
Baumgart DC, Sandborn WJ. Lancet. 2007;369:1641-1657.
Sandborn WJ. J Clin Gastroenterol. 2008;42:338-344.
7
Aminosalicylates (5-ASA) Monitoring
• Sulfasalazine:
Nausea, vomiting, headache, reversible male infertility, anemia
• Olsalazine:
Diarrhea
• All:
Paradoxical worsening of colitis (rare)
Pancreatitis/Hepatitis/Pericarditis/Pneumonitis (rare)
• Requires Monitoring
Renal Function (~yearly) Interstitial nephritis (rare)
Budesonide Metabolism and Characteristics
Oral budesonide1
pH release: ileum/right colon
MMX: pan-colonic
~10% Budesonide
~90% metabolism in the liver
o
budesonide1
Rectal
Enema/Foam
o
Budesonide characteristics2
o
Non-halogenated corticosteroid,
highly lipophilic
o
Good tissue penetration
o
9x greater receptor binding than
dexamethasone
o
Rapidly absorbed in GI tract
o
Metabolites are almost inactive
o
Terminal half-life 2.7 +/- 0.6 hours
Needs specifically designed release
system
Adapted from 1Brattsand R. Can J Gastroenterol. 1990;4(7):407-414; 2Gross V. Expert Opin
Pharmacother. 2008;9(7):1257-1265.
Mild-Moderate UC
• Most UC patients present with mild to moderate disease
• Aminosalicylates:
Do not have a clear dose response from 2.4 to 4.8 grams
4.8 g/day may be more effective than 2.4 g/day in patients with a
history of more difficult to treat disease (e.g., previous use of oral
5-ASAs, rectal therapies, steroids, or multiple medications)
• Topical steroids:
Effective to treat active UC
Fewer adverse effects than oral corticosteroids
Mild-Moderate UC
• Patients with left-sided UC are most effectively treated
with topical mesalamine therapy
• Topical mesalamine demonstrated to be more effective
than oral mesalamine in left-sided UC
• Budesonide MMX is effective for left-sided colitis and
pancolitis
Positioning will depend upon future clinical trials
Management of Moderate UC:
• Maximize 5-ASA therapy first
– Increase to maximal dose of 5-ASA
– Add topical therapy
– Confirm medication adherence, simplify regimen if
indicated
– ? 5-ASA hypersensitivity
• Rule out Clostridium difficile infection at least
once for change in UC symptoms
Management of Moderate UC:
• If corticosteroids are necessary, plan for an exit
strategy on Day 1
– Recurrent steroid tapers are not efficacious
• Calcium + Vitamin D supplementation while on
steroids
– Bone densitometry if indicated
• Routine vaccinations prior to starting
immunosuppression
Corticosteroid Therapeutic Monitoringdverse
Effects to Steroids
Annual ophthalmologic
exams recommended
Glaucoma
Cataracts
Vaccinations: flu,
pneumonia
Infection
Osteoporosis
Avascular
Necrosis
Myopathy
Diabetes
Palpitations
Hypertension
GI upset
• Calcium + Vit D
Nausea
supplementation
• Bone densitometry
Fatty liver
Monitor for adrenal
insufficiency?
Swelling
Moon facies
Abdominal striae
Easy bruising
Sandborn WJ. Can J Gastroenterol. 2000;14(suppl C):17C-22C.Kornbluth and Sachar. Am JGastroenterol. 2010;105:501-523.
Thiopurines: Azathioprine (AZA) &
6-Mercaptopurine (6-MP)
–Minimal efficacy for induction versus placebo
–More effective for maintenance versus placebo
Thiopurine Pharmacology
Inactive
6-TU
Active
Bone Marrow
Suppression
XO
AZA
HPRT
6-MP
6-TIMP
TPMT
TPMT
6-MMP
Inactive
Elevated LFTs
6-MMPR
6-TXMP
6-TGN
6-TGN
Thiopurines: Therapeutic Monitoring
Allergic reaction:
Fever, rash, arthralgias,
Myalgias, fatigue
Vaccinations: flu,
pneumonia
Infection
Pancreatitis
GI disturbances
Hepatotoxicity, ?
Nodular regenerative
hyperplasia
Bone marrow
suppression
Malignancy/
lymphoma
Routine dermatology exams
Sun protection
Kornbluth A, Sachar DB. Am J Gastroenterol. 2004;88:1371.
deBoer N et al. Nature Clin Pract Gastroenterol Hepatol. 2007;4:686.
Timing of CBCs with Thiopurine Therapy
• Close monitoring during first 8 weeks of therapy
appears warranted
• If mild leukopenia during the first 8 weeks
and/or large reduction in WBC from baseline,
hold drug and recheck CBC
• After the first 8 weeks, less frequent monitoring
is reasonable
• Continue Monitoring every 3 months!
Risk of Developing Non-Hodgkin’s Lymphoma
Patient with Crohn’s disease
Estimated annual risk =
2 per 10,000 treated patients
Risk of Developing Non-Hodgkin’s Lymphoma
Patient with Crohn’s disease receiving 6MP or Azathioprine
Estimated annual risk =
4 per 10,000 treated patients
Methotrexate Side Effects
• Rash
• Nausea, mucositis, diarrhea
• Bone marrow suppression
• Hypersensitivity pneumonitis
• Increased liver enzymes
• Hepatic fibrosis/cirrhosis
• Known abortifacient
• No documented increased risk of lymphoma or
skin cancer
Methotrexate Therapeutic Monitoring
• Regular counseling regarding birth control
• 1 mg folic acid supplementation daily
• Monitor CBC, liver enzymes every 6 weeks
• Evaluate risk factors for liver disease
Diabetes
Obesity
Alcohol abuse
• Routine dose based liver biopsy no longer
recommended
Anti-TNF biologics:
Fusion protein, antibodies and PEGylated
Fab' fragment
Etanercept
Infliximab
Fab
Receptor
Chimeric
Certolizumab
pegol
Fab′
PEG
IgG1
Fc
IgG1
Fc
Human
recombinant
receptor/Fc fusion
protein
Adalimumab
Golimumab
Human
Monoclonal
antibody
PEGylated
humanized
Fab′ fragment
2 × 20 kDa
PEG
Therapeutic Levels for Anti-TNF Agents
5.0
10.0
50.0
Theoretical threshold
1.0
Adalimumab 160 mg (day 1), 80 mg (day 8)
and 40 mg ev ery tw o w eek s
Adalimumab 40 mg ev ery tw o w eek s
0.5
Simulated anti-TNF biologic conc
Inflix imab 5 mg/k g at day 1, day 15, day 43 and ev ery 8 w eek s
Inflix imab 3 mg/k g at day 1, day 15, day 43 and ev ery 8 w eek s
Subtherapeutic
0
20
40
60
Time (day s )
80
100
120
Therapeutic
DrugMonitoring
Monitoring
of Tumor
Therapeutic Drug
of Tumor
Necrosis
FactorAntagonists
Antagonists
in IBD
Necrosis Factor
in IBD
Drug adjustment empirically based on
clinical symptoms often is inaccurate
and may lead to suboptimal outcomes
Patient-related factors* may influence
the pharmacokinetics of these agents
Recent evidence shows that maintenance of
an optimal therapeutic drug concentration is
associated with improved clinical outcomes
Incorporation of therapeutic drug
monitoring into clinical practice may
allow clinicians to optimize treatment
by maintaining effective drug
concentrations over time
* Sex and/or body size, and disease severity, including TNF burden and serum albumin concentration
Ordás I, Feagan BG, Sandborn WJ. Clin Gastroenterol Hepatol. 2012;10(10):1079-87.
Therapeutic Monitoring for Anti-TNF
• Vaccinations: flu,
Autoimmunity,
immunogenicity
Congestive
heart failure
• Use combination therapy
with thiopurines?
• Check anti-TNF levels?
• Check for antibodies?
pneumonia
Demyelinating
disease,
•
TB
testing
PML*
• Hepatitis screening
Infection
Hepatotoxicity
Bone marrow
suppression
Malignancy/
lymphoma
Infusion reactions,
injection-site reactions
• Switch to another anti-TNF agent?
• Switch to agent with different mechanism of action?
*Reported with natalizumab.
Risk of Developing Non-Hodgkin’s Lymphoma
Patient with Crohn’s disease receiving combination anti-TNF + 6MP or azathioprine
Estimated annual risk =
6 per 10,000 treated patients
α4β7 Integrin–MAdCAM-1 Is One of the
Interactions that Contributes to Chronic
Inflammation in UC and CD
Gut lumen
Dendritic cells
Infiltrating
lymphocytes
Chemokines/ILs
Inappropriate and sustained
recruitment of
inflammatory cells
Macrophage
Vedolizumab Binds to α4β7 Integrin and
Blocks Its Interaction With MAdCAM-1
Endothelial cell
MAdCAM-1
Vedolizumab:
A humanized monoclonal
antibody (mAb) that binds to
the α4β7 integrin
α4
subunit
β7
subunit
Vedolizumab
blocks the
interaction of α4β7
integrin with
MAdCAM-1
α4
subunit
Memory T lymphocyte
β7
subunit
Artist’s rendition
Please see Important Safety Information contained on slides 33-34.
29
Anti-Integrins inhibit inflammatory cells from
getting into the (gut) tissues
Entyvio
Memory T lymphocyte
migration inhibited
Memory T lymphocyte
homing to gut tissue inhibited
Artist’s rendition
Vedolizumab inhibits the migration
of memory T lymphocytes across the
endothelium into inflamed
gastrointestinal parenchymal tissue.
Entyvio does not bind to or inhibit
function of the α4β1 or αεβ7
integrins.
Therapeutic Monitoring and Adverse Events with
Vedolizumab
• Rare Infusion-related reactions & hypersensitivity
30 minute infusion and no post-infusion monitoring
• Not recommended in patients with active, severe infections until
the infections are controlled
• No cases of PML have been observed
• Rare reports of elevations of transaminase and/or bilirubin
• All patients should be brought up to date with all immunizations
Patients may receive non-live vaccines and may receive live
vaccines if the benefits outweigh the risks.
• Most common adverse reactions (incidence ≥3% and ≥1% higher
than placebo): nasopharyngitis, headache, arthralgia, nausea,
pyrexia, upper respiratory tract infection, fatigue, cough,
bronchitis, influenza, back pain, rash, pruritus, sinusitis,
oropharyngeal pain, and pain in extremities.
High Risk Patients
• Older
• Multiple co-morbidities
• Concomitant steroids and/or narcotics
• Long-standing disease
• Young “healthy” patients are not in the clear, but probably much less at risk
• ? Prior malignancy
Vaccinations in the IBD Patient
Titers to check at first office visit:
MMR
Varicella
Hepatitis A
Hepatitis B
If vaccination history unknown
If vaccination history or history of chicken pox/zoster
unknown
Except those with evidence of protective titer within 5
years of vaccine administration
Except those with evidence of protective titer within 5
years of vaccine administration
Vaccinations to administer
in specific patient groups
regardless of immunosuppressive
drug use:
Vaccinations to consider
if NO plans to start
immunosuppressive
therapy in 4-12 weeks:
Tdap
HPV
Influenza
Pneumococcal
MMR
Varicella
Zoster * OK for thiopurines
Hepatitis A
Hepatitis B
Meningococcal
Wasan SK, et al. Am J Gastroenterol. 2010;105(6):1231-8.
DiPalma J, et al. Gastroenterol Hepatol (N Y). 2011;7:163-9.
Summary of Selective Therapeutic
Monitoring
5-ASAs
CBC1,2
x
Liver enzymes3,4
x
Creatinine/Urinalysis/BUN3
x
Eye examination1
Opportunistic infections
(e.g., TB, Hep B, and
varicella)
Immunizations1,4
TPMT
Bone mineral density for
>3 mo use
Corticosteroids
x
Immunomodulators
x
Biologics
x
x
x
x
x
x
x
x
x
x
x
x
x
1. Kornbluth A, et al. Am J Gastroenterol. 2010;105:501-23. 2. Lichtenstein GR, et al. Am J
Gastroenterol. 2009;104(2):465-83.
3. Agency for Healthcare Research and Quality (AHRQ). http://guidelines.gov/content.aspx?id=15231.
4. Sands BE, et al. Inflamm Bowel Dis. 2004;10:677-92.