Cooperating Parties for ICD-9-CM
advertisement
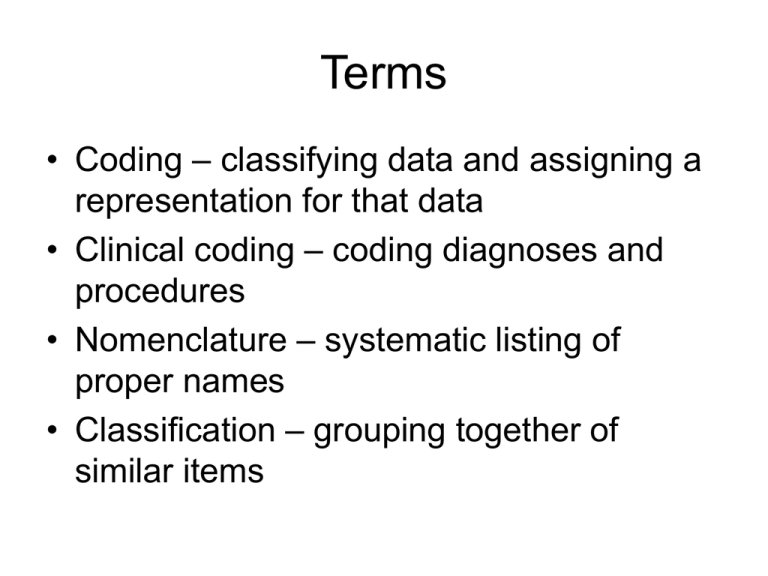
Terms • Coding – classifying data and assigning a representation for that data • Clinical coding – coding diagnoses and procedures • Nomenclature – systematic listing of proper names • Classification – grouping together of similar items Other systems • Diagnostic and Statistical Manual of Mental Disorders – DSM • ICD-O • Systemized Nomenclature of Human and Veterinary Medicine International – SNOMED – Topography; morphology; function; living organisms; chemicals, drugs, and biological products; physical agents, activities, and forces; occupation; social context; disease/diagnosis; procedures; general • Read codes (specifically for use in computerized formats) • LOINC (Logical Observation Identifier Names and Codes) – for laboraory (mapped to SNOMED) • Case Mix and Severity of Illness – DRGs, RUGs, Atlas Cooperating Parties for ICD-9-CM Organization Responsibilities National Center for Health Statistics • Maintains the disease classification • Approves official coding guidelines Health Care Financing Administration • Maintains the procedure classification • Approves official coding guidelines American Hospital Association • Maintains Central Office on ICD-9-CM • Approves official coding guidelines • Publishes Coding Clinic American Health Information Management Association • Certifies coders • Provides coding education • Sponsors Council on Coding and Classification and the Society for Clinical Coding • Approves official coding guidelines Menu Coding Process • Review of medical record • Selection of diagnoses and procedures to code • Assignment of code numbers • Sequencing codes (esp. inpatients) • Entry of coded data into database (abstracting) • Generation of indexes and Entry of codes on patient’s bill DRG’s Notice to Physicians: Medicare payment to hospitals is based in part on each patient’s principal and secondary diagnoses and the major procedures performed on the patient, as attested to by the patient’s attending physician by virtue of his or her signature in the medical record. Anyone who misrepresents, falsifies, or conceals essential information required for payment of Federal funds, may be subject to fine, imprisonment, or civil penalty under applicable federal laws. Encoder • Logic – asks questions • Automated codebooks Ethical coding • http://www.ahima.org/infocenter/guidelines /standards.cfm Quality of Coding • National Correct Coding Intitiative (NCCI) – Fiscal intermediaries – Medicare Code editor • Peer review organizations – now Quality Improvement Organization (QIO) – South Dakota Foundation For Medical Care http://www.sdfmc.org • Fraud and Abuse – compliance plans Quality of Coding • Reliability – get same results – Same coder is intrareliability – Different coders is interreliability • Validity – accurately reflect diagnosis/procedure • Completeness – • Timeliness – Cause of Errors • • • • • Failure to review entire record Selection of incorrect principal diagnosis Selection of incorrect code Coding dx/proc not validated in record Errors in data entry Improve Quality • Coding policies – – – – – – – – Instructions on what to do about conflicting documentation Instructions on what to do when a code cannot be found Directions for reviewing the record Use of optional codes (e.g., outcome of delivery, M codes) List of UHDDS definitions Directions for keeping books updated Use of reference materials (e.g., Coding Clinic) Requirements for abstracting • Quality improvement studies • Documentation guidelines Hiring Coders Coding time per record x number of discharges and/or visits for period ___________________________________ Number of paid hours worked per coder for the time period 30 minutes x 10,000 discharges/year = 300,000 minutes or 5000 hours ______________________________________________________ 1800 hours/year (2080 is full time, figure for time off, breaks, etc.) 5000/1800 = 2.78 coders needed Other Issues • Retention of coders – Incentive system – CE opportunities – Benefits (work setting, flex time) • • • • Resources Contract coding and review services Concurrent/Retrospective coding Specialization