RPA Update 2011-Craig Moore_c
advertisement

Optimisation of Computed Radiography
chest imaging utilising a digitally
reconstructed radiograph simulation
technique
Craig Moore
Radiation Physics Service
Hull & East Yorkshire Hospitals NHS
Trust
www.hullrad.org.uk
Introduction - Literature
• Lots of publications have shown that patient
anatomy is the limiting factor in the reading
normal structures, and detection of lesions (lung
nodules) in chest images
–
–
–
–
–
–
–
Bochud et al 1999
Samei et al 1999, 2000
Burgess et al 2001
Huda et al 2004
Keelan et al 2004
Sund et al 2004
Tingberg et al 2004
• European wide RADIUS chest trial (2005)
Introduction - Literature
• Chest radiography is
now generally
considered to be
limited by the
projected anatomy
• Patient anatomy =
anatomical noise
So if we want to optimize digital system for chest
imaging, vital that anatomical noise is present in
the images!!!
Introduction
• However, the radiation dose/image quality
relationship must not be ignored
• Doses must be kelp ALARP
– ICRP 2007
– IR(ME)R2000 – (required legally in the UK)
• We would therefore want system
(quantum) noise present in an image for
dose reduction studies
Digitally Reconstructed Radiograph
(DRR)
• Hypothesis:
– Can use CT data of humans to provide realistic
anatomy (anatomical noise)
• Clinically realistic computerized ‘phantom’
– Simulate the transport of x-rays through the ‘phantom’
and produce a digitally reconstructed radiograph
(DRR – a simulation of a conventional 2D x-ray image
created from CT data)
– Add frequency dependent system noise post DRR
calculation
– Add radiation scatter post DRR calculation
– Validate
– Use for optimization studies
DRR Algorithm: Virtual Patient
•
•
•
Virtual patient derived from chest
portion of real CT datasets
Voxel resolution = 0.34 x 0.34 x 0.8
mm
CT number converted to linear
attenuation coefficient (LAC) using
tissue equivalent inserts
– Measure mean CT No. in each
insert
– We know elemental composition
of each so can derive LAC
– Can derive relationship between
CT No. and LAC
CT dataset reorientated in
the ‘PA’
direction
Final CT axial
batch (i.e. slices
681 to 700)
Energy absorbed in
CR phosphor
of X-rays
Intensity
(E)
A E I ( E ){1 exp
x }dE
exiting
is
calculated
E max
en
0
0
CT axial batch 2
(i.e. CT slices 21
to 40)
PA slice N
CT axial batch 1
(i.e. CT slices 1 to
20)
PA slice 1
X-ray spectra
derived from
IPEM 78
X-ray attenuated
exponentially
through CT
dataset using a
ray casting
method of DRR
calculation
Scatter Addition
• Must add to DRR generated image
– DRR algorithm does not calculate scatter
• Measured scatter in CR chest images using lead pellet
array
• Use chest portion of RANDO phantom
Based on
slightly modified
work by Bath et
al, 2005
Noise Addition
lung
spine
diaphragm
Uniform noise image
Corrected noise image
Lung Nodule Simulation
• Added artificial nodules to the CT data prior to Xray projection
• Baed on work by Li et al 2009
Human DRR
v Human CR
DRR
CR
DRRs: 50 kVp v 150 kVp
Scatter Rejection
• The DRR algorithm can produce images with scatter rejection
DRR No Rejection
DRR Grid
CR
DRR
DRR
(a)
CR Grid
(b)
(c)
Obese Patients
• DRR algorithm can also produce images
of large/obese patients
DRR
CR
(a)
(b)
Validation
• Decided to validate with RANDO and real
patient images:
– Histogram of pixel values
– Signal to noise ratios (SNR)
• Important because signal and noise affects the
visualisation of pathology
– Tissue to rib ratios (TRR)
• Pixel value ratio of soft tissue to that of rib
• Important as rib can distract the Radiologist from
detecting pathology
Phantom Histograms
CR - 60 kVp 10 mAs
CR - 150 kVp 0.5 mAs
Frequency
20000
10000
0
20000
10000
Pixel Value
00
35
00
00
33
00
31
29
DRR - 150 kVp 0.5 mAs
40000
Frequency
30000
20000
10000
0
30000
20000
10000
Pixel Value
b
Pixel Value
d
00
35
00
33
00
31
00
29
00
27
00
25
00
23
00
21
00
19
00
17
00
15
00
35
00
33
00
31
00
29
00
00
27
25
00
23
00
21
00
19
00
0
17
00
00
c
DRR - 60 kVp 10 mAs
15
27
Pixel Value
a
Frequency
00
25
00
00
23
21
00
19
15
00
00
00
00
35
33
00
31
00
29
00
00
27
00
25
23
00
21
00
19
00
00
0
17
15
30000
17
Frequency
40000
115
5000
117 0
7000
119 0
9000
221 0
1000
0
223
3000
0
225
5000
0
227
7000
0
229
9000
0
331
100
00
333
300
00
335
500
0
Frequency
Frequency
1155
0000
1177
0000
1
1990
000
22110
000
22330
000
22550
000
2
2770
00
29 0
29 0
00
31 0
31 0
00
33 0
33 00
0
35 0
35 00
00
Frequency
Frequency
Phantom Histograms
CR
CR-- 90
90kVp
kVp14mAs
mAs
30000
20000
10000
10000
00
Pixel Value
Pixel Value
DRR- -90
90kVp
kVp41mAs
mAs
DRR
30000
30000
20000
20000
10000
10000
00
PixelValue
Value
Pixel
PATIENT - Histograms
DRR His togram
Frequency
60000
Typical histogram of
average patient DRR
30000
0
1744
1995
2246
2497
2748
Pixe l Value
Patie nt CR His togram
Frequency
60000
Typical histogram
of average patient
CR image
30000
0
1733
2012
2291
Pixe l Value
2570
2849
SNRs
• Good agreement in lung, spine and diaphragm
areas of chest
• Maximum deviation approx 15%
– Mean deviation = 7%
• Addition of frequency dependent noise not
perfect:
– CR system noise is ergodic (changes with time)
– Noise added here is a snapshot (and so not ergodic)
– However, quantum noise dominates over ‘ergodic
noise’ so not such an issue
– DQE is NOT constant with dose variation in image
Validation - TRRs
• Good agreement
– Within 2%
• As tube potential increases TRR
decreases
– Due to rib attenuating higher percentage in
incident photons at lower potentials than soft
tissue, thus forcing up TRR
Validation - Radiologists
• Have told me DRR
images contain sufficient
clinical data to allow
diagnosis and
subsequent optimisation
• They have scored the
images out of 10
– ‘are the images sufficiently
like real CR images?
– Average score of 7.8
Conclusions – DRR Algorithm
• DRR computer program has been produced that adequately
simulates chest radiographs of average and obese patients
– Anatomical noise simulated by real human CT data
– System noise and scatter successfully added post DRR generation that
provides:
• SNRs
• TRRs
• Histograms
– in good agreement with those measured in real CR images
• Provides us with a tool that can be used by Radiologists to grade
image quality with images derived with different x-ray system
parameters
• WITHOUT THE NEED TO PERFORM REPEAT EXPOSURE ON
PATIENTS
• ACCEPTED FOR PUBLICATION IN THE BJR
– AUGUST 2011
Optimisation of CR Chest Radiography
using DRR Generated Images
• In Hull chest exposure factors were not standardised
(historical reasons!!!!)
• Three main hospital sites:
– 60 kVp & 10 mAs
– 70 kVp & 5 mAs
– 80 kVp & 5 mAs
• In the last 6 months, four expert image evaluators have
scored DRR reconstructed images
– Two Consultant Radiologists
– Two Reporting Radiographers
• Scoring criteria based on European guidelines (CEC)
What to Optimise?
• Optimum tube potential for Average
Patients (70 kg ± 10 kg)
– Without scatter rejection (as per Hull protocol)
– With scatter rejection (grid and air gap)
• Optimum tube potential for Obese patients
– Without scatter rejection
– With scatter rejection
• Is Scatter rejection indicated?
• Dose reduction?
Scoring Criteria
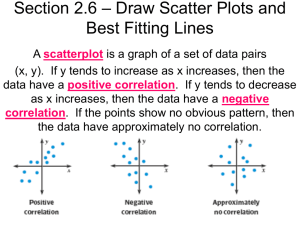
• Images scored on a dual PACS monitor system
• Image on right hand screen held at a constant
kVp
• Images on left hand screen displayed from 50 to
150 kVp in steps of 10kVp (approx)
– Image 1 = 50 kV
– Image 2 = 60 kV
– Image 10 = 150 kV
• Test images scored against reference image
• All images matched effective dose
STUCTURE – NORMAL ANATOMY
GRADING
IMAGE 1
IMAGE 2
IMAGE 3
Vessels seen approx approx 3 cm from the pleural
GRADING
VISIBILITY OF STRUCTURE
margin
-3
Definitely inferior to the reference image
Thoracic vertebrae behind the heart
-2
Reasonably inferior to the reference image
Retrocardiac vessels
Pleural margin
-1
Slightly inferior to the reference image
0
Equal to the reference image
+1
Slightly better than the reference image
+2
Reasonably better than the reference image
+3
Vessels seen en face in the central
area
Definitely better than the reference image
Hilar region
STUCTURE – LUNG NODULES
GRADING
Nodule in lateral pulmonary region
Nodule in hilar region
Are the ribs a distraction? Y/N
[1] European guidelines on quality criteria for diagnostic
radiographic images. CEC European Commission EUR
16260 EN (Luxembourg 1996)
IMAGE 4
Tube Potential Optimisation
Results – Average Sized Patients,
no scatter rejection
0.6
VGAS
0.5
0.4
0.3
0.2
`
0.1
0
40
60
80
100
120
Tube Potential kVp
VGAS = average of Radiologists results
140
160
Results – Average Patients with
scatter rejection - grid
0.3
0.2
0.1
0
VGAS
0
20
40
60
80
-0.1
-0.2
-0.3
-0.4
-0.5
Tube Potential (kVp)
100
120
140
160
Results – Average Patients with
scatter rejection – air gap
0.2
0.1
0
40
60
80
100
VGAS
-0.1
-0.2
-0.3
-0.4
-0.5
Tube Potential (kVp)
120
140
160
Results – Obese Patients without
scatter rejection
0.2
0.15
0.1
0.05
0
0
-0.05
-0.1
-0.15
-0.2
-0.25
20
40
60
80
100
120
140
160
Results – Obese Patients without
scatter rejection
• Very weak trend for better image quality with higher kVp
• Lower kVps probably ‘worse’ due to combination of:
– Lack of penetration through obese patient
– Increased scatter from obese patient (scatter to cassette
changes very little with kVp)
• This is not so with average patients
– Less tissue (fat) so more radiation penetration
– Less scatter from fat
• It is likely that poorer radiation penetration and increased
scatter from obese patient outweighs the inherent benefit
of photoelectric contrast obtained from lower kVps
Results – Obese Patients with
scatter rejection - grids
1
0.8
0.6
VGAS
0.4
0.2
0
40
60
80
100
-0.2
-0.4
-0.6
Tube Potential (kVp)
120
140
160
Results – Obese Patients with
scatter rejection – air gap
0.4
0.2
0
40
-0.2
-0.4
-0.6
-0.8
-1
-1.2
-1.4
-1.6
-1.8
60
80
100
120
140
160
Scatter Rejection
Scatter Rejection vs no scatter
rejection – average patients
1.4
1.2
VGAS
1
0.8
0.6
0.4
0.2
0
grid
air gap
Scatter Rejection Technique
Scatter Rejection vs no scatter
rejection – average patients
• Superior image quality with scatter rejection
technique
• Grids performed much better than air gap
• Statistically significant differences
• BUT:
– Image evaluators were asked if increase in dose due
to use of grids was justified, even with better image
quality
– Answer in 100% of cases was NO
– SCATTER REJECTION FOR AVERAGE PATIENTS
IS NOT INDICATED
Exposure time for average patients without
scatter rejection and low tube potentials?
• Scatter rejection not indicated
• Therefore low kVps should be used (remember the
graph)
• European guidance recommends exposure times < 20
ms
• Can we achieve this with low kVps??
• Modern Philips X-ray generator:
– For lgM = 2 (Agfa CR specific Dose Indicator)
– With 630 mA, all kVps are possible
– Max exp time = 16 ms
• At the expense of increased tube loading
Scatter Rejection vs no scatter
rejection – obese patients
1.6
1.4
1.2
VGAS
1
0.8
0.6
0.4
0.2
0
grid
air gap
Scatter Rejection Technique
Scatter Rejection vs no scatter
rejection – obese patients
• Superior image quality with scatter rejection
technique
• Grids performed much better than air gap
• Statistically significant differences
• BUT:
– Image evaluators were asked if increase in dose due
to use of grids was justified, even with better image
quality
– Answer in 100% of cases was YES
– ANTI SCATTER GRID USE FOR OBESE PATIENTS
IS INDICATED
Exposure times for obese patients
with an anti-scatter grid
• Remember that low tube potentials were superior with an
anti-scatter grid!!!!
• Need exposure times < 20ms
• Is this possible with low kVps and scatter grid for lgM =
2??
• Scatter grid is a focused grid so have to use it in a fixed
range of FDD
– Nominal distance = 140 cm FDD
– Range allowed = 115cm – 180cm
• At 140 cm FDD lowest exp time = 17.6ms @ 109 kVp
• At 115cm FDD lowest exp time = 20 ms @ 90 kVp
• So are limited to 90 kVp
Dose Reduction
Dose Reduction?
• Images were also
presented at different
doses
Dose reduction?
• Results suggest doses can be reduced by
around 50% before image quality begins
to suffer and become unacceptable
• Therefore could half exposure mAs
•
Conclusions – Use of DRR
algorithm to optimise CR chest
imaging
Average patients:
– No scatter rejection is indicated
– Therefore, low kVps (< 102 kVp) are indicated
– Can have exposure times < 20 ms for all kVps
• Obese patients
– Anti-scatter grid is indicated
– So low kVps (<102kVp) should be used
– For exposure times < 20ms, are limited to 90 kVp
• Doses
– As low as 50% reduction possible
• ACCEPTED FOR PUBLICATION IN BJR
Optimisation & Standardisation in
Hull?
• Agreed with Consultant Radiologists:
– 60 kVp & 10 mAs
• After a ‘settling in’ period:
– 60 kVp & 8 mAs
– Want to go lower than 8mAs eventually!!!
• Implication on patient dose?
–
–
–
–
Using PCXMC effective dose calculation software:
80 kVp/5 mAs = 0.011 mSv
60 kVp/8 mAs = 0.006 mSv
Approx 45% drop in effective dose