Anaesthesia Breathing Systems
advertisement
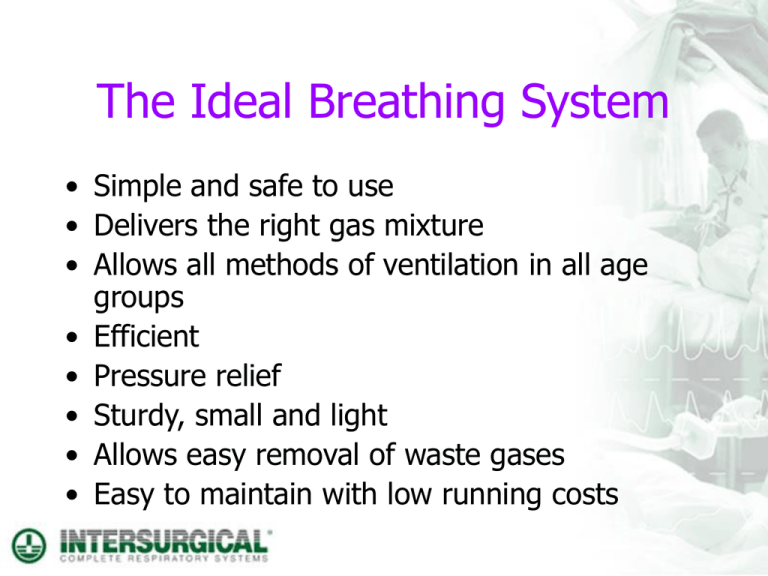
The Ideal Breathing System • Simple and safe to use • Delivers the right gas mixture • Allows all methods of ventilation in all age groups • Efficient • Pressure relief • Sturdy, small and light • Allows easy removal of waste gases • Easy to maintain with low running costs Breathing System Components • Fresh Gas connection • Patient connection • Adjustable Pressure Limiting (APL) Valve • Reservoir (Bag or bellows) • Tubing • Waste gas connection Open, semi open, semi closed? • Open is the old fashioned method of dropping ether or chloroform over a gauze or lint. Later modernised by the likes of the Schimmelbusch mask. • Semi-open I classify as systems used today such as the Mapleson systems. • Semi-closed and Closed systems use a CO2 absorbent so that the gases are re-circulated, the classification is defined by the amount of fresh gas flow. Semi-open Systems • In the early 1950’s, Prof. WW Mapleson from University of Wales, Cardiff, classified the several breathing systems around depending on what components they contained and what position they took in the system. • It is known today as ‘The Mapleson Alphabet’ The Mapleson Alphabet The F was added later to the alphabet Semi-open Circuit Anaesthesia • This is typically used for induction of the patient. It is usually a single limb system that uses an APL valve to control the pressure of the gas, and allows for waste gas to leave the system. • High fresh gas flows (more than patients minute volume) are required with these systems to stop rebreathing of expired CO2. Types of Semi-open Circuit Systems • • • • • • Mapleson Mapleson Mapleson Mapleson Mapleson Mapleson D or Bain System A or Magill System A or Lack System F or Ayres T Piece System F with APL Valve C Bagging System What FGF’s are needed? Mapleson Systems Uses A Magill Lack Spontaneous Gen Anaesthesia B Very uncommon, not in use today C Resuscitation Bagging D Bain Spontaneous IPPV, Gen. Anaes E Ayres T Piece Very uncommon, not in use today F Jackson Rees Paediatric <25 Kg FGF SV 70-100 ml/kg/min FGF IPPV Min 3 x MV Min 15 lpm 150-200 ml/kg/min 2.5 – 3 x MV Min 4 lpm 70-100 ml/kg/min Mapleson A (Magill) System 1950’s • The Mapleson A or Magill system is good for spontaneous breathing patients, so the fresh gas flow can be lower. However as the APL valve is close to the patient, it is regarded by many as difficult to use. Mapleson A (Lack) System 1976 • The Mapleson A or Lack system is a modification of the Magill where the valve is moved to the machine end of the system using another length of tubing. This adds volume to the system and makes it rather heavy at the patient end. Mapleson D (Bain) 1972 • The Mapleson D or Bain System is a co-axial system where the fresh gas is delivered directly to the patient. It requires very high fresh gas flows to prevent rebreathing of CO2. It is very convenient to use, thus is very popular especially for induction, in the UK! Mapleson F (Jackson Rees Modification) Ayres – 1937 JR - 1950 • The Mapleson F or Jackson Rees modification of the Ayres T Piece is a basic system for use with very small patients. It is a big disadvantage that you cannot remove waste gases safely. • Because this has a bag with an open tail, it is technically a Jackson-Rees Modification system Mapleson F with APL Valve 1998 • Intersurgical decided to modify the JacksonRees by using a closed tail bag and a specially modified APL valve. Now the waste gases can be removed safely from the system via the APL valve’s 30mm outlet. Mapleson C Bagging System • The Mapleson C is more than an anaesthesia system. It can be found all over the hospital for use as an emergency bagging system for resuscitation or manual ventilation using oxygen, as well as being a standard induction system in some countries. Semi Closed Circuit Anaesthesia • This type of General Anaesthesia is used mainly for maintenance of anaesthesia following induction. It can be used for induction of anaesthesia, but this is a slower process. • It requires an absorber system containing a CO2 Absorbent to remove CO2 from the expired patient gases, and a high degree level of patient monitoring, especially respiratory gas monitoring to measure levels of inspired and expired CO2 and the volatile agent. Semi Closed Anaesthesia Explained • Semi Closed Anaesthesia is where the expired gases from the patient pass through a canister in the breathing system which contains a CO2 absorbent. This absorbent by an exothermic chemical reaction removes the CO2, so the patients expired gases can be rebreathed. Because of this exothermic chemical reaction, some warmth and humidity is added to the inspired gases. Semi Closed Anaesthesia Explained • Because the patients expired gases are re circulated (where the ‘circle’ comes from), this means that we do not have to add so much fresh gas to the system like an open system. So the fresh gas flow rate can be reduced to low flow, i.e., 1 litre per minute. If the flows were as low as a few hundred cc’s of gas, equivalent to the patients metabolic uptake of gases, this would be closed circuit anaesthesia, or metabolic (basal) flow, or minimal flow. • Circle systems were first used back in 1930 by Brian Sword in the USA Types of Semi Closed Circuit System • • • • Standard Parallel Y System Extendible Parallel Y System Complete Semi Closed Circuit Systems Co-Axial Semi Closed Circuit Systems ‘Tight Connections’ • Remember, it is important with conical connectors such as those used on breathing systems, always connect with a firm push and twist. This will ensure a leak tight connection. Conclusion •The silver ion based anti-microbial additive reduced the potential risk of cross contamination from the outside of the breathing system •This means that the anti-microbial additive in Breathing Systems not only inhibits bacterial growth but will reduce colonisation on the circuit, and therefore can reduce cross infection in the ITU and the operating theatre Well that’s it! I hope you now have a clearer understanding of Breathing Systems and Filtration. It really only leaves me one thing to say: ‘TIGHT CONNECTIONS’