Renal July 2012- Lecture 2
advertisement

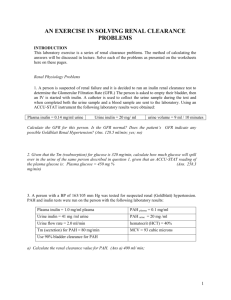
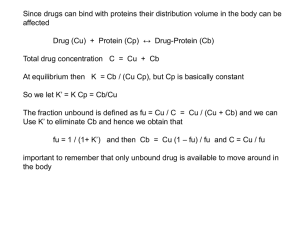
Glomerular Filtration & Factors Affecting GFR A.A.J.Rajaratne Objectives Describe the glomerular membrane, interms of the major layers and its permeability characteristics Explain in terms of size and electrical charges of pores of the membrane and why the glomerular membrane has a high degree of selectivity. •State the glomerular pressure, Bowman’s capsular pressure and colloid osmotic pressure in the glomerular capillaries and explain how these pressures cause filtration of fluid at the glomerulus •State the composition of the glomerular filtrate •Explain the terms of GFR and filtration fraction and give their normal values Describe the effect of the following on the GFR 1. 2. 3. 4. Renal blood flow Afferent and efferent arteriolar constriction Sympathetic stimulation Outflow obstruction Recognize that GFR is kept constant with wide changes in arterial blood pressure by means of autoregulation GLOMERULAR FILTRATION GFR – Males 90-140 ml/min Females 80 -125 ml/min About 180 litres of plasma is filtered per day Glomerular Filtrate Devoid of cells and protein Concentration of salts and organic molecules (glucose and amino acids) are similar in the plasma and ultra filtrate The Glomerulus • Capillary endothelium - pores 100nM • Basement membrane • Tubular epithelium pores - 8nM Filtrate = plasma - protein EFP=(PGC – PBS) – (COPGC-COPBS) GFR = Kf . EFP Kf – Filtration coefficient ml/min/mmHg Starling Forces Starling Forces For Filtration: • Hydrostatic Pressure in Glomerulus (45 mm Hg) • Colloid O.P. in tubule (0 mmHg) Against Filtration • Hydrostatic Pressure in tubule (10 mm Hg) • Colloid O.P. in glomerular blood (25mm Hg) GFR can be altered by changing 1. 2. Kf Any of the Starling forces Factors affecting glomerular filtration 1.Role of hydrostatic and oncotic pressures 2. Role of capillaries 3. Role of mesangial cells Renal Blood Flow 1.25 L per minute = 25% of the CO Indirectly determine GFR Modify rate of water and solute reabsorption by the PCT Participating in concentration and dilution of urine Delivering substrates for the excretion in the urine Autoregulation of RBF & GFR RBF & GFR remains relatively constant between 90 – 180 mmHg Autoregulation of RBF & GFR 1.Pressure sensitive - Myogenic mechanism 2.NaCl concentration dependent mechanism Autoregulation of RBF & GFR 1.Is absent below arterial pressures of 90mmHg 2.Autoregulation is not perfect 3.Despite autoregulation, RBF & GFR can be changed under appropriate conditions by several hormones. Major Hormones that Influence GFR & RBF Vasoconstrictors Sympathetic nerves Angitensin II Endothelin Major Hormones that Influence GFR & RBF Vasodilators Prostaglandin (PGE2, PGI2) Nitric Oxide Bradykinin ANP Tubulo-glomerular Feedback SNGFR is greater in juxtamedullary nephrons – 50 nl/min (others 30 nl/min) The SNGFR is determined by composition of the fluid in the distal nephron. The mechanism is called tubulo-glomerular feed back. Estimation of glomerular filtration rate Clearance: The clearance of a substance is the volume of plasma from which the substance was completely cleared by the kidneys per unit time, (units = vol. plasma/time), CX = UX V PX Clearance of ‘X’, CX = GFR when the substance ‘X’ meets the following criteria, i. freely filterable at the glomerulus ii. not reabsorbed by tubules iii. not secreted by tubules iv. not synthesised by tubules v. not broken-down by tubules These criteria are met by the polysaccharide inulin, so CIN = GFR. However, inulin does not occur naturally in the body and requires several hours of infusion to reach steady state concentration. Therefore, creatinine is used to estimate GFR. Creatinine is formed from muscle creatine and is released at approximately a constant rate. Therefore blood [Cr] changes little per 24 hrs. However, Cr is secreted by the tubules and overestimates GFR by small amount. for freely filterable substances, when, a. CX < CIN net tubular reabsorption b. CX > CIN net tubular secretion Para-aminohippurate PAH Undergoes tubular secretion and is freely filterable. At low [PAH]pl, virtually all PAH escaping filtration is secreted by the tubule. Therefore virtually all plasma supplying secreting nephrons is cleared of PAH. About 10-15% of total renal plasma flow (TRPF) supplies non-secreting portions of the kidney. Thus, CPAH actually measures effective renal plasma flow (ERPF). This is ~ 85-90% of TRPF. This only applies at a low [PAH]pl, at higher levels the TMax is exceeded. The radiographic contrast Diodrast is handled similarly to PAH. urea is freely filterable but ~ 50% is reabsorbed (R: 40-60%). The amount reabsorbed depends on flow rate. Therefore urea is less accurate than creatinine as an estimate of GFR. Fractional Excretion: Fractional excretion, FEX , is the mass of "x" excreted as a fraction of the total mass filtered, where FEX = UX ´V GFR ´PX and if, 1. FEX < 1.0 reabsorption 2. FEX > 1.0 net tubular net tubular secretion Estimation of glomerular filtration rate: This may be done using the clearance of a substance present in plasma that is filtered freely at the glomerulus, but is neither reabsorbed nor secreted by the tubules. Inulin, a polysaccharide of MW » 5000, satisfies these criteria. PA(inulin)x RPF Inulin clearance No reabs; No secretion. Filtered = Excreted PV(inulin)x RPF Filtered = Pin X GFR Pin X GFR = Uin X V Excreted = Uin X V Since inulin cannot be absorbed or secreted, all inulin that is filtered at the glomerulus must appear in the urine. In the steady state, the rate of filtration (moles/min) of inulin must be equal to its excretion in the urine (moles/min). Rate of inulin filtration (moles/min) = Pinulin (moles/ml) x GFR (ml/min) Rate of excretion of inulin (moles/min) = Uinulin (moles/ml) x V (ml/min) where Uinulin and Pinulin represent the concentrations of inulin in urine and plasma, respectively, and V represents the rate of urine flow. 2. inulin filtration rate = inulin excretion rate Pinulin x GFR = Uinulin x V So that GFR = UinV/Pin 3. The right-hand-side of equation = the clearance of inulin. (The clearance of any other substance is UV/P for that substance.) 4. The GFR is equal to the clearance of inulin, or of any other substance that is freely filtered, but neither reabsorbed nor secreted. 5. The "normal" value of GFR for a 70 kg human is about 125 ml/min. Creatinine clearance: In clinical practice creatinine clearance may be used to estimate GFR for the following reasons. 1. Inulin is not produced endogenously. Therefore, it must be infused intravenously if it is to be used in renal function tests. It is much more convenient to use a substance that is normally present in plasma that is freely filtered, but neither secreted, nor reabsorbed. 2. Creatinine, a normal breakdown product of creatine, is an endogenous compound that fulfils these criteria. Creatinine clearance - contd: However, in humans, a small amount of creatinine is secreted into the urine in the proximal tubules. Consequently, the rate of excretion of creatinine exceeds its rate of filtration by 5 to 10%. The clearance of creatinine thus exceeds the true GFR by 5 to 10%. Creatinine clearance - contd: All that is required is a single plasma sample and 24 hour urine collection. In most renal diseases substantially reduced. the GFR is This is detected by a diminished creatinine clearance or, more frequently, by elevated Pcreatinine. PAcr x RPF No reabs; No secretion. Filtered = Excreted Pcr X GFR = Ucr X V PVcrx RPF Filtered = PcrX GFR Small amount is secreted Excreted = Ucr X V Estimation of renal plasma flow rate: Certain substances are extracted from peritubular capillary plasma and secreted into the proximal tubular fluid in large amounts. The concentration of such substances in renal venous plasma is therefore, much less than in renal arterial plasma. In such cases, the direct Fick Principle (blood flow = rate of excretion/(A-V) concentration difference) can be used to estimate renal plasma flow rate. PAH (para-aminohippuric acid) might be used for this purpose. 1. In the steady state, the rate at which PAH enters the kidney (moles/min) in the renal arterial plasma is equal to the rate at which PAH leaves the kidney in the urine and in renal venous blood. PAH (moles/min) entering kidney in renal arterial plasma = Pa PAH x RPF PAH (moles/min) leaving kidney in renal venous plasma = Pv PAH x RPF PAH (moles/min) leaving kidney in the urine = UPAH V PAPAH x RPF Near-complete extraction in one passage through kidney. UPAH V PVPAHx RPF = 0 2. The rate at which PAH enters the kidney is equal to the rate that it leaves. Then, 3. Note that this last expression is the Direct Fick formula for measuring plasma flow: the blood flow is equal to the rate of consumption (excretion) divided by the arterio-venous concentration difference. 4. It is common to make the approximation that the concentration of PAH in renal venous blood is zero. Substituting zero for venous [PAH], allows us to compute a quantity called the effective renal plasma flow (ERPF). 5. Note that the ERPF is equal to the clearance of PAH and that it underestimates the true renal plasma flow by approximately 10%. 6. The "normal value" of ERPF in a 70 kg human is about 625 ml/min. Since the PAH clearance underestimates renal plasma flow by about 10%, the true renal plasma flow (RPF) is about 700 ml/min. 7. The renal blood flow (RBF) is then RBF = RPF/1 - Hct ml blood/min, so that if the hematocrit is 45%, and RPF = 700 ml/min, then RBF is 1273 ml/min. This is 20 to 25% of cardiac output. 8. The filtration fraction is defined as the ratio of GFR/RPF. If GFR = 125 ml/min and RPF = 700 ml/min, then the filtration fraction is 0.179. The filtration fraction is typically between 0.15 and 0.20.