DRAFT : DO NOT CITE
Long-term Projections of
the Cost of Treatment
Under Various Scenarios –
Opportunities for Efficiency
and Effectiveness?
July 19/20, 2014
Arin Dutta, Cathy
Barker, and Ashley
Kallarakal
Outline
1. Projecting and costing global HIV treatment
Number on treatment
a) Current vs. WHO 2013 need for ARVs
b) Scale-up of programmatic coverage
c) Migration to 2nd line treatment
Cost of HIV treatment
Funding gap analysis for HIV treatment
2. Emerging Themes: E2 in HIV Treatment
3. HPP E2 analyses
Insights from Kenya, Tanzania, and Mozambique
Why focus on HIV Treatment?
Critical intervention in the response: preventing premature
mortality and new infections
HIV treatment requires more resources than any other single
area of the HIV and AIDS response
UNAIDS : 39% of all resources for HIV
Exciting time in the discussion on ART:
90-90-90 call from UNAIDS: 90% diagnosed, 90% on ART; 90%
virally suppressed by 2020
UNAIDS 2014 “Ambitious Treatment Targets: Writing the final chapter of the AIDS epidemic”
Country Inclusion Criteria
93 countries included in the analysis, based on criteria:
More than 1,000 PLHIV in country
Eligible for Global Fund funding for HIV in 2014
Countries grouped into the following 6 regions:
Africa: West and Central (AWC) - 22
Africa: East and Southern (AES) - 20
Latin America and the Caribbean (LAC) - 14
Middle East and North Africa (MENA) - 9
Eastern Europe and Central Asia (EECA) - 12
Asia and the Pacific (AP) - 16
Projecting Global HIV
Treatment Needs
a) ART Need: Methods
Used AIM in Spectrum to estimate projected numbers of adult
and pediatric patients that are eligible for ART from 20142020 in each of the 93 countries.
Spectrum AIM was used individually for each country
Two eligibility scenarios:
Current eligibility#:
Adult: CD4<350 or 250* and Option B+ (all HIV+ PW)
Children: CD4<350 for ages 5-14; CD4<750 for ages 24-59 mo.; all
under 24 mo. (irrespective of CD4)
WHO 2013 eligibility#:
Adult: CD4<500 and Option B+ (all HIV+ PW)
Children: CD4<500 for ages 5-14; all under 5 (irrespective of CD4)
* Depending on current country guidelines as preset in Spectrum.
# HIV & TB co-infected with CD4 above 350 (or 500) are a very small proportion; not included in this round of analysis.
2013
2014
2015
2016
2017
2018
2019
WHO 2013
Current
WHO 2013
Current
WHO 2013
Current
WHO 2013
Current
WHO 2013
Current
WHO 2013
Current
WHO 2013
Current
WHO 2013
Current
Adult ART need (in millions)
Global Need for ART: Adults
30
25
20
15
MENA
EECA
LAC
10
AP
AWC
5
AES
0
2020
Source: Dutta, Barker, Kallarakal (forthcoming, 2014)
Global Need for ART: Pediatric
2.0
1.5
MENA
EECA
LAC
1.0
AP
AWC
0.5
AES
2013
2014
2015
2016
2017
2018
2019
WHO 2013
Current
WHO 2013
Current
WHO 2013
Current
WHO 2013
Current
WHO 2013
Current
WHO 2013
Current
WHO 2013
Current
WHO 2013
0.0
Current
Pediatric ART need (in millions)
2.5
2020
Source: Dutta, Barker, Kallarakal (forthcoming, 2014)
b) ART Coverage: Methods
Coverage: Number on ART on Dec. 31st / Need for ART, Dec. 31st
Step 1: Established 2013 baseline coverage % for adults and
children in each of 93 countries, looking at:
Number on ART from 2013 UNGASS country reports; national reports
& documents*, or value in Spectrum (in this order)
Divided this by current need for ART on Dec. 31st in the country
Step 2: Set possible scale-up paths for countries from this base:
9.17 million on ART in 2012, a 19.8% increase on 2011*
Two scale-up scenarios:
Slow scale-up: 20% annual increase in coverage %
e.g., country’s coverage in 2014: 40%; coverage in 2015: 48%
Fast scale-up: 30% annual increase in coverage %
* Sources: WHO/PAHO 2013 (“ART in Spotlight: LAC”); WHO et al. TUA Progress Report 2013, etc.
2013 ART Coverage %: Adult
Bubble size shows Current ART Need in 2013
Source: Dutta, Barker, Kallarakal (forthcoming, 2014)
2013 ART Coverage %: Pediatric
Bubble size shows Current ART Need in 2013
Source: Dutta, Barker, Kallarakal (forthcoming, 2014)
c) 1st & 2nd line ART: methods
Step 1: Established 2013 split of patients on 1st vs. 2nd line ART,
adults and children separately (if poss.)
By country: UNGASS 2013 country reports, national data, global/regional
reports. WHO regional average used for missing
Step 2: Define region-specific annual migration rate ranges:
% of 1st line moving to 2nd line, per year
A region has countries classified into “high / med. / low.” This range
differs by region. Overall range across regions: 0.5% to 3% p.a.
Country designated within region based on resistance*, LTFU, etc.
Step 3: Migration scenarios by country over 2014-2020:
Base migration: As set above: assumes historical rates continue; increased
detection with VL cancelled by lower proximal factors for failure
Higher migration: Migration increases from base: Increased patient load
stresses systems; higher detection with VL, etc. – greater switching
E.g.: Country with low migration moves to medium; medium moves to high
* Stanford Drug Resistance Database
ScenarioID
Scenario Definition
C20ScaleBM1 Number of patients on 1st line ART regiment based on: current ART guidelines; Scale up of ART coverage by 20%, current migration scheme to
2nd line treatment
C30ScaleBM1 Number of patients on 1st line ART regiment based on: current ART guidelines; Scale up of ART coverage by 30%, current migration scheme to
2nd line treatment
C20ScaleHM1 Number of patients on 1st line ART regiment based on: current ART guidelines; Scale up of ART coverage by 20%,higher migration scheme to
2nd line treatment
C30ScaleHM1 Number of patients on 1st line ART regiment based on: current ART guidelines; Scale up of ART coverage by 30%, higher migration scheme to
2nd line treatment
WHO20ScaleBM1 Number of patients on 1st line ART regiment based on: WHO2013 ART guidelines; Scale up of ART coverage by 20%, current migration
scheme to 2nd line treatment
WHO30ScaleBM1 Number of patients on 1st line ART regiment based on: WHO 20103 ART guidelines; Scale up of ART coverage by 30%, current migration
scheme to 2nd line treatment
WHO20ScaleHM1 Number of patients on 1st line ART regiment based on: WHO 2013 ART guidelines; Scale up of ART coverage by 20%,higher migration
scheme to 2nd line treatment
WHO30ScaleHM1 Number of patients on 1st line ART regiment based on: WHO 2013 ART guidelines; Scale up of ART coverage by 30%, higher migration
scheme to 2nd line treatment
Median_1st_line
Median of all 1st line scenario totals
C20ScaleBM2 Number of patients on 2nd line ART regiment based on: current ART guidelines; Scale up of ART coverage by 20%, current migration scheme to
2nd line treatment
C30ScaleBM2 Number of patients on 2nd line ART regiment based on: current ART guidelines; Scale up of ART coverage by 20%, current migration scheme to
2nd line treatment
C20ScaleHM2 Number of patients on 2nd line ART regiment based on: current ART guidelines; Scale up of ART coverage by 20%, high migration scheme to 2nd
line treatment
C30ScaleHM2 Number of patients on 2nd line ART regiment based on: current ART guidelines; Scale up of ART coverage by 20%, high migration scheme to
2nd line treatment
WHO20ScaleBM2 Number of patients on 2nd line ART regiment based on: WHO2013 ART guidelines; Scale up of ART coverage by 20%, current migration
scheme to 2nd line treatment
WHO30ScaleBM2 Number of patients on 2nd line ART regiment based on: WHO2013 ART guidelines; Scale up of ART coverage by 20%, current migration
scheme to 2nd line treatment
WHO20ScaleHM2 Number of patients on 2nd line ART regiment based on: WHO2013 ART guidelines; Scale up of ART coverage by 20%, high migration
scheme to 2nd line treatment
WHO30ScaleHM2 Number of patients on 2nd line ART regiment based on: WHO2013 ART guidelines; Scale up of ART coverage by 20%, high migration scheme
to 2nd line treatment
Median_2st_line
Median of all 2nd line scenario totals
Projected number of Adults on 2nd
Line ART
Range based on 8 scenarios
Number on 2nd line ART (in millions)
4.5
High: 3.9 million
4.0
3.5
2.9
3.0
2.5
2.5
2.0
2.0
1.5
1.3
Range
0.9
1.0
0.5
Low: 2.2 million
1.6
0.5
Median
0.6
0.0
2013
2014
2015
2016
2017
2018
2019
2020
Source: Dutta, Barker, Kallarakal (forthcoming, 2014)
Projected number of Children on
2nd Line ART
Range based on 8 scenarios
Number on 2nd line ART (in thousands)
300
High: 262 thousand
250
191
200
165
139
150
114
Low: 143 thousand
91
100
69
50
37
Range
50
Median
0
2013
2014
2015
2016
2017
2018
2019
2020
Source: Dutta, Barker, Kallarakal (forthcoming, 2014)
Projected numbers on ART: Adult
Based on increasing coverage from current base
Range based on 16 scenarios
Number on ART (in millions)
35
High: 29.2 million
30
25
21.0
24.7
25.4
Low: 22.1 million
18.6
20
Range
15.1
15
10
22.6
23.8
Median
9.9
5
0
2013
2014
2015
2016
2017
2018
2019
2020
Source: Dutta, Barker, Kallarakal (forthcoming, 2014)
Projected numbers on ART: Ped.
Based on increasing coverage from current base
Range based on 16 scenarios
Number on ART (in millions)
2.5
High: 2 million
2.0
1.5
1.3
1.4
1.5
1.5
1.1
Low: 1.3 million
1.0
1.0
1.6
Range
Median
0.7
0.5
0.0
2013
2014
2015
2016
2017
2018
2019
2020
Source: Dutta, Barker, Kallarakal (forthcoming, 2014)
Cost of HIV Treatment
Costing Methods: Annual ARVs
Used regional average patient-year costs by income
category for WHO-preferred regimens
Adult 1st line
Adult 2nd line
Pediatric 1st line
Pediatric 2nd line
TDF + 3TC + EFV
ZDV+3TC+LPV/r
ABC+3TC + LPV/r
ZDV + 3TC + EFV
ZDV+3TC+NVP
TDF+FTC+LPV/r
ZDV + 3TC + LPV/r
ABC + 3TC + EFV
ABC + 3TC + EFV
ZDV + 3TC + LPV/r
ZDV+3TC+EFV
ABC + 3TC +LPV/r
ZDV+3TC+EFV
Annual drug costs from WHO Global Price Reporting
Mechanism database; as regional averages by income level
Most prices are from 2013 (transactions before 2011 excluded)
Assumed regimen prices stable from 2014 to 2020, in 2013 $
Substituted global averages, matching income level, for any missing
region/income level and regimen data
Regimen splits and per year costs reviewed against country-specific costing
studies from HPP (2014) and CHAI (2012)
Costing Methods: Lab and
Facility-Level Costs
Lab costs: 3 scenarios x 3 income levels
Compiled estimates of country-specific unit costs* per test into
averages by low, low-middle and middle income level groups
Three cost scenarios per income level: via # tests and unit cost:
Scenario →
High cost
Medium cost
Low cost
CD4
1 x yr., avg. unit cost
2 x yr., avg. unit cost
2 x yr., lowest unit cost
Viral load
Routine, avg. unit
cost
Targeted (5%), avg.
unit cost
Targeted (5%), lowest
unit cost
Hematology and
clinical chemistry
2 x yr., avg. unit cost
2 x yr., avg. unit cost
2 x yr., lowest unit cost
Facility-level costs**
Average % of direct commodity costs (ARV and lab) that is spent on
personnel and overhead (building utilities and contracted services)
Percentages differ by income level group
Assumed stable percentage of costs from 2014-2020
Sources: * HPP 2014, CHAI 2013, MSF 2013; many others; Sources: ** Gallaraga et. al 2011, PEPFAR 2013, many others
Total costs: Three Scenarios
Highest cost scenario
Highest numbers on treatment
WHO 2013 eligibility, 30% annual scale-up rate in coverage, highest
2nd line migration scenario
Highest unit cost for lab
Medium cost scenario
Median numbers on treatment
Medium unit cost for lab
Lowest cost scenario
Lowest numbers on treatment
Current eligibility, 20% annual scale-up rate in coverage, current 2nd
line migration scenario
Lowest unit cost for lab
Total Annual ART Costs (93 countries):
ARVs, lab, personnel, and facility-level costs
Total cost of HIV treatment (in USD billions)
$9
High: $8.5 billion
$8
$7
$6
$5.1
$5
$4
$5.6
$6.0
$6.4
$6.7
Low: $5.5 billion
$4.4
$3.6
$3
Range
$2
Medium
cost
scenario
$1
$-
2014
2015
2016
2017
2018
2019
2020
All costs in 2013 US$. Source: Dutta, Barker, Kallarakal (forthcoming, 2014)
Disaggregating total costs of ART for
93 countries: Medium Scenario
Total medium-scenario costs (in USD billions)
$8
$7
$6
Overhead
$5
Personnel
Lab
$4
Pediatric ART 2nd Line
$3
Pediatric ART 1st Line
$2
Adult ART 1st Line
Adult ART 2nd Line
$1
$-
2014
2015
2016
2017
2018
2019
2020
All costs in 2013 US$. Source: Dutta, Barker, Kallarakal (forthcoming, 2014)
Proportion of Total Costs 20142020: Medium Scenario
Overhead
6%
Personnel
16%
Lab
10%
Adult ART
63%
Pediatric ART
5%
Source: Dutta, Barker, Kallarakal (forthcoming, 2014)
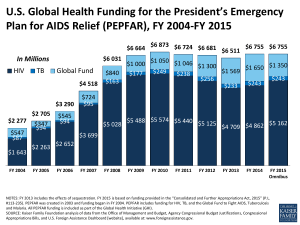
Funding gap analysis: Methods
Annual level of GFATM funding for HIV
Based on late 2013 and 2014 funding disbursements for all open
HIV grants, excluding civil society organization PRs
Global total: $558.7 million/year
Annual level of PEPFAR funding for ART
2013 funding commitments for treatment and care for 31 countries
Total: $1.95 billion/year
3 funding gap scenarios:
Largest gap: Highest cost scenario, current GFATM funding stays
constant, subtracted 30% from PEPFAR funding (overhead)
Medium gap: Median cost scenario, current PEPFAR and GFATM
funding, constant over time
Smallest gap: Lowest cost scenario, current PEPFAR and
GFATM funding, constant over time
Sources: PEPFAR 2013 COPs (sum of budget codes HBHC, HKID, HLAB, HTXD, HTXS, HVTB, PDCS, PDTX only); GFATM
2014 disbursement report (July 2014 update)
Annual funding gap across 93
countries (prior to domestic contribution)
Includes ARV, lab, personnel and overhead costs
$7
High: $6.6 billion
Funding gap (in USD billions)
$6
$5
$4
$2.6
$3
$3.1
$3.5
$3.8
Low: $2.9 billion
$1.9
$2
$4.2
Range
$1.1
$1
$-
2014
2015
2016
2017
Year
2018
2019
2020
Medium
cost
scenario
All values in 2013 US$. Source: Dutta, Barker, Kallarakal (forthcoming, 2014)
Annual funding gap across 93
countries (prior to domestic contribution)
Includes ARV and lab costs only
$6
High: $4.8 billion
Funding gap (in USD billions)
$5
$4
$3
$2
$1
$1.5
$1.9
$2.2
$2.5
$2.7
Low: $1.7 billion
$1.0
Range
$0.3
$-
2014
2015
2016
2017
2018
2019
2020
Medium
cost
scenario
$(1)
Year
All values in 2013 US$. Source: Dutta, Barker, Kallarakal (forthcoming, 2014)
Emerging Themes: E2 in HIV
Treatment
Key Findings
Need to increase cost-efficiency:
Continue to reduce ARV prices and wider use of low-cost WHO-
recommended regimens
Example: A 5% reduction in ARV prices could save as much as $1.5
billion from 2014-2020
Reduce facility-level costs
Example: Reducing proportion of direct costs spent on personnel and
overhead by 5% would save as much as $485 million from 2014-2020
Reduce lab costs
Example: Reducing unit costs of all lab tests to the lowest current price
would save as much as $2.5 billion from 2014-2020
Need to increase effectiveness:
How to increase coverage by 20-30% per year on existing base?
Better use of viral load testing to detect and switch on failure
Prevent large rise in future 2nd line treatment need
Potential E2 Gains across ART
cascade
Interventions that reduce ART
costs
Interventions that promote sustained viral
suppression up to 90%
Decentralize, but maintain viable facilitylevel patient loads
Treatment simplification: new methods to deliver
ARVs with lower pill burden; long-term dosing
Task shifting: reduce per-patient personnel
costs
Better patient monitoring whether via virological or
immunological testing
Further expansion of FDC formulations
Community-based models of patient monitoring and
adherence support
Consolidation of lower cost platforms for
viral load testing, even at POC; reduction
of reagent costs
Treat comorbidities, including malnutrition, to keep
patient healthy and in care
Interventions that help increase
coverage up to 90% or more
Eliminate losses across ART cascade
(75% lost from test to treat? Mugglin et al. 2012)
Reduce cross-cutting delivery challenges
Treatment site positioning and strengthening; timing;
family-based approaches, structural/social enablers.
Critical short-term investments (e.g., new VL equipment) may lead to
long-term efficiency and effectiveness gains
Limitations of analysis
Assessment of needs
Serodiscordant couples (also recommended) not included
Coverage projections
Not able to use UNAIDS/WHO 2014 Country Progress Reports, data not
released
Costs of ART missing
Costs of OI treatment (non-TB), psychosocial support, nutrition, where
these are available
Above-facility level costs (programmatic support, training)
Gap analysis issues
Overestimation of both GFATM and PEPFAR funds - values are not
specific to cost categories included. Data not available
HPP Studies on E2
Lessons Learned from Kenya
Efficient interventions
Effective interventions
HIV testing; MoH switched testing algorithm to
yield highest cost savings while maintaining
accuracy
Option B+; averts more infant and adult
infections than Option B, but at a significant
additional cost
HCW training; harmonized in-service training
curriculum with long-term mentoring is costefficient
Harm reduction services for key populations;
combination package (NSP, MAT, HCT, and ART
for PWID) is cost-effective (ICER of $1,600)
Screening blood supply for transfusions; costbenefit ratio of 3 for additional costs to screen all
blood vs. averted TTI treatment costs
Oral PrEP for sex workers; cost-effectiveness
ratio in Kenya is $25 per HIV infection averted;
costs could decrease through task shifting
New ART guidelines; adopting WHO 2013
guidelines would result in a significant reductions
in new HIV infections and premature deaths
Workplace interventions; mainstream HIV
response, promote prevention programs, fight
stigma and discrimination
Lessons Learned from
Mozambique
Need to increase allocative efficiency:
Target geographic regions and population groups contributing the
most to HIV incidence
Need to scale-up biomedical and behavior change
interventions to achieve greatest health impact
Revised HIV acceleration plan could avert 113,927 new infections
and 145,668 AIDS-related deaths
Need both types of interventions to reach goal of halving HIV
incidence by 2017
Thank You!
www.healthpolicyproject.com
The Health Policy Project is a five-year cooperative agreement funded by the U.S. Agency for International
Development under Agreement No. AID-OAA-A-10-00067, beginning September 30, 2010. The project’s HIV
activities are supported by the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR). It is implemented by
Futures Group, in collaboration with Plan International USA, Futures Institute, Partners in Population and
Development, Africa Regional Office (PPD ARO), Population Reference Bureau (PRB), RTI International, and the
White Ribbon Alliance for Safe Motherhood (WRA).