Warfarin - NL Congressi
advertisement

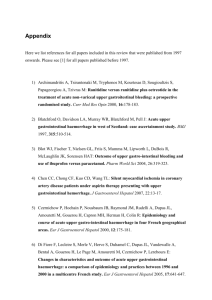
NUOVI ANTICOAGULANTI ORALI DIRETTI: COME NEUTRALIZZARE LA ATTIVITA’ ANTICOAGULANTE DAVIDE IMBERTI CENTRO EMOSTASI E TROMBOSI MEDICINA INTERNA DIPARTIMENTO DI MEDICINA GENERALE OSPEDALE GUGLIELMO DA SALICETO PIACENZA Nuovi anticoagulanti: pratica clinica Monitoraggio laboratoristico “Reverse” dell’effetto anticoagulante Gestione complicanze emorragiche Gestione perioperatoria Switch da VKA (e viceversa) Quali pazienti ESC 2012 guidelines: management of bleeding with new oral anticoagulants Patient on a new OAC presenting with bleeding Check haemodynamic status, basic coagulation tests to assess anticoagulation effect Minor • Delay next dose or discontinue treatment Moderate • • • • • Very severe • Consider rFVIIa or PCC • Charcoal filtration • Dabigatran only: haemodialysis Symptomatic/supportive treatment Mechanical compression Fluid replacement Blood transfusion Oral charcoal if recently ingested Camm, Eur Heart J, 2012 Emivita media dei farmaci attuali Warfarin: 36-42 ore Rivaroxaban: 7-11 ore Apixaban: 12 ore Dabigatran: 12-14 ore Edoxaban 6-12 ore EBPM: 3-6 ore Fondaparinux: 13-21 ore NAO e EMORRAGIE Informazioni cliniche importanti Tipo di farmaco Dose Ora dell’ultima assunzione Eventuale coesistenza di insufficienza renale Monitoring and Antidotes Monitoring Antidote Warfarin INR TTR Vitamin K Dabigatran TT - Hemoclot® Monoclonal Ab ECT (aPTT) FXa Inhibitors Factor Xa activity (PT) Universal antidote in ph 2 (FX analogue: PRT4445) All Hb concentrations HAS-BLED # Fresh frozen plasma Prothrombin complex concentrate FEIBA rFVIIa Weitz , Hematology Am Soc Educ Program, 2012 Concentrati di Complesso Protrombinico (PCC) • Rivaroxaban: significativo allungamento del PT – Allungamento revertito immediatamente e completamentre dal PCC • Dabigatran: significativo allungamento dell‘aPTT – Nessun effetto sull‘aPTT del PCC • Conclusioni – PCC reverte in vivo nell‘uomo l‘effetto anticoagulante di rivaroxaban Eeremberg, Circulation, 2011 Reversal of rivaroxaban by PCC A randomized, placebo-controlled, crossover study in healthy subjects Eerenberg, Circulation, 2011 Marlu, Thromb Haemost, 2012 Apixaban Reversal with PCC, aPCC and rFVIIa In Vitro with Circulating Human Blood Objective Study Design In vitro analysis to test the reversibility of the alterations in hemostasis caused by apixaban using different coagulation factor concentrates Whole Blood from Healthy Donors Apixaban 200 ng/ml added to blood Coagulation Factors Added Measurement of Apixaban Anticoagulant Activity rFVIIa: Novoseven® 270 µg/kg Platelet function at high shear rates (IMPACT-R) aPCC: Feiba® 75 U/kg PCC: Beriplex® 50 IU/kg Thrombin generation (TECHNOTHROMBIN) Viscoelastic parameters (ROTEM) Studies under flow conditions Aliquots of plasma for further testing In vitro analysis demonstrated that apixaban Results Did not interfere with the reactivity of platelets Inhibited thrombin generation Caused moderate reduction in thromboelastometry parameters (TEM) Apixaban-induced alterations of hemostasis were variably compensated or even reversed by the different factor concentrates used in this analysis, including PCCs, active PCCs, and rFVIIa. Effects of these concentrates were not homogeneous in all the tests PCCs demonstrated greater efficacy in reversing apixaban effect measured by thrombin generation rFVIIa demonstrated greater effectiveness in reversing apixaban effect in TEM and perfusion chamber analyses Adapted from Escolar G, Arellano-Rodrigo E, Reverter JC, et al. Reversal of apixaban induced alterations of hemostasis by different coagulation factor concentrates: studies in vitro with circulating human blood. Presented during the American Heart Association-Emerging Science Series webinar; June 20, 2012. Available at: http://my.americanheart.org/idc/groups/ahamah-public/@wcm/@sop/@smd/documents/downloadable/ucm_441679.pdf Prothrombin complex concentrate, activated prothrombin complex concentrate (Feiba), and recombinant factor VIIa (rFVIIa) significantly reversed the anticoagulant effect of edoxaban in vitro. 186 Fukuda, Thromb Haemost, 2012 Use of PCCs for urgent reversal of dabigatran in the Emergency Department Quintana-Diaz, Haematologica, 2013 Use of PCCs for urgent reversal of dabigatran in the Emergency Department Quintana-Diaz, Haematologica, 2013 Reversing the NOACs with PCCs: what is the evidence ? - Systematic review about dabigatran, rivaroxaban, apixaban, edoxaban. - PCCs (including activated PCCs) show promise for reversing the anticoagulant effects of the new oral anticoagulants. - Conventional laboratory assays do not correlate well with bleeding or reversal of anticoagulation in this setting; thrombin generation assays appear to have the best predictive value. Dickneite , Thromb Haemost, 2014 Dabigatran antidote: characteristics • Fully humanized antibody fragment (Fab) • Potently binds dabigatran • No prothrombotic or anti-thrombotic effects • Short half-life • No endogenous targets • Allows for intravenous administration van Ryn J, Circulation, 2012;126:A9928 Reversal of anticoagulation ex vivo: results • Antidote reverses the anticoagulant activity of dabigatran within 1 min of i.v. bolus injection to rats Plasma levels Dabigatran (nM) 125 100 75 50 25 8000 7000 6000 5000 4000 3000 2000 1000 0 8000 7000 6000 5000 4000 3000 2000 1000 0 Fab Level (nM) Thrombin time (seconds) Thrombin clotting time 0 -20 -20 0 5 10 15 20 25 30 Time (min) 0.3 + 0.1 mol/kg/hr BIBR 953 BI 655075 0.3 µmol/kg Control + BI00655075 0.3 µmol Control 0 5 10 15 20 25 30 Time (min) Dabi 0.3 + 0.1 umol/kg/hr Dabi+Fab Vehicle+Fab Dabi (+0.3 umol Fab) Dabigatran: bolus (0.3 mol/kg) + infusion (0.1 mol/kg/hr) (0.141mg/kg) + (0.047mg/kg/hr) SE, n=4. Schiele, Blood, 2013 Dabigatran bolus (0.3 mol/kg) + infusion (0.1 mol/kg/hr)Data expressed as mean Thrombin time: 3.0 U/ml thrombin used in the assay A specific antidote for dabigatran: immediate, complete and sustained reversal of dabigatran induced anticoagulation in healthy male volunteers Glund, OC17765, AHA, Dallas, 2013 r- Antidote (PRT064445) has a high affinity for Xa inhibitors Antidoto: ANDEXANET ALFA (Portola) • Analogo ricombinante del FXa • Non partecipa alla formazione del complesso della protrombinasi e all’attivazione del FII – Elevata capacità legante per gli inibitori del FXa (rivaroxaban, apixaban, betrixaban, ecc.) Management of major bleeding events in patients tretaed with rivaroxaban vs warfarin: results from the ROCKET AF Pharmacologic management post-major bleed (0-24 hours) Rivaroxaban Warfarin (n=431) (n=409) Vitamin K 32 (7.4%) 54 (13.2%) Protamine 0 (0.0%) 0 (0.0%) Desmopressin 0 (0.0%) 0 (0.0%) Epsilon-aminocaproic acid 2 (0.5%) 3 (0.7%) Tranexamic acid 2 (0.5%) 11 (2.7%) Prothrombin complex concentrates 4 (0.9%) 9 (2.2%) Recombinant factor VIIa 0 (0.0%) 1 (0.2%) Factor VIII concentrate 1 (0.2%) 1 (0.2%) Factor IX concentrate 0 (0.0%) 3 (0.7%) Piccini, Eur Heart J, 2014 Outcomes following ISTH major bleeding Stroke or systemic embolism Events Riva Warfarin (N=431) (N=409) 20 (4.7%) 22 (5.4%) Interaction P Value 0.888 (0.420, 1.876) 0.5135 HR (95% CI) Composite of all stroke, non-CNS embolism, MI/UA, and all-cause death 104 (24.8%) 120 (29.9%) 0.758 (0.530, 1.082) 0.0975 All-cause death 86 (20.4%) 105 (26.1%) 0.688 (0.455, 1.042) 0.1098 MI/UA 11 (2.6%) 1.848 (0.572, 5.971) 0.5597 7 (1.7%) 0.1 Favors rivaroxaban 1 10 Favors warfarin Piccini, Eur Heart J, 2014 Strategies used for management of major bleeding: RE-LY® trial – results Dabigatran* Warfarin 741 (100) 421 (100) Blood transfusion, n (%) 439 (59.2) 210 (49.9) 0.002 Fresh frozen plasma, n (%) 147 (19.8) 127 (30.2) <0.001 70 (9.4) 115 (27.3) <0.001 Prothrombin complex concentrate, n (%) 5 (0.7) 5 (1.2) 0.36 Recombinant Factor VIIa, n (%) 8 (1.1) 3 (0.7) 0.53 Patients with major bleeds, n (%) Vitamin K, n (%) P value Major bleeds in the dabigatran groups were more frequently treated with blood transfusions than those on warfarin but less frequently with plasma Data derived based on the randomized set of RE-LY® *Data combined from dabigatran 150 mg and 110 mg BID treatment groups Mayeed, Blood, 2012 Short-term consequences of major bleeding: RE-LY® trial – results Dabigatran* Warfarin P value Patients with major bleeds, n (%) 741 (100) 421 (100) Patients with hospitalization,† n (%) 456 (61.5) 254 (60.3) 0.68 Length of stay, days, mean (SD) 8.4 (9.1) 8.9 (9.8) 0.48 Nights in ICU/CCU, mean (SD) 1.6 (4.3) 2.7 (6.6) 0.01 Nights in step-down unit, mean (SD) 1.0 (2.5) 1.0 (2.7) 0.84 Patients with major bleed requiring surgery, n (%) 90 (12.1) 63 (15.0) 0.17 Length of stay in ICU is shorter with dabigatran treatment than with comparator Data derived based on the randomized set of RE-LY®; *Data combined from dabigatran 150 mg and 110 mg BID treatment groups; †First reported hospitalization is given for a major bleeding event, if admission to hospital was between 1 day before event and 7 days after event Length of stay, night in ICU/CCU, night in step-down unit was obtained from all hospitalization events (dabigatran = 510; warfarin = 273) CCU = coronary care unit; ICU = intensive care unit; SD = standard deviation Mortality after a major bleed: five Phase III trials – results Warfarin Dabigatran Mortality rate (%) 0.2 0.1 0.3 0 5 10 15 20 Time (days) 25 30 35 The Kaplan–Meier analysis indicated a reduced risk for death with dabigatran* vs warfarin during 30 days from the bleeding (P=0.052) *Data combined from dabigatran 150 mg and 110 mg BID treatment groups. Only first major bleed included. Analysis not adjusted for covariates Major Bleeding in Patients with Atrial Fibrillation Receiving Apixaban or Warfarin in the ARISTOTLE Trial: Predictors, Characteristics, and Clinical Outcomes Characteristics of major extracranial hemorrhage Characteristics of ISTH Major Extracranial Hemorrhage Overall Apixaban Warfarin Hazard Ratio (95% CI) Event Rate (%/yr) Event Rate (%/yr) Event Rate (%/yr) Apixaban vs. Warfarin Led to hospitalization 1.23 (374) 1.05 (162) 1.41 (212) 0.75 (0.609–0.917) 0.0052 Fall in hemoglobin 2 g/dL 1.25 (381) 1.06 (164) 1.44 (217) 0.74 (0.603–0.905) 0.0035 Led to transfusion 1.06 (325) 0.89 (137) 1.25 (188) 0.71 (0.571–0.887) 0.0025 Required a medical or surgical consultation 1.74 (527) 1.54 (236) 1.94 (291) 0.79 (0.668–0.941) 0.008 Required a medical or surgical intervention to stop 0.77 (236) 0.65 (100) 0.90 (136) 0.72 (0.555–0.930) 0.012 Associated with hemodynamic compromise 0.32 (97) 0.26 (40) 0.38 (57) 0.69 (0.459–1.029) 0.069 Caused changed in antithrombotic therapy 1.31 (398) 1.14 (176) 1.47 (222) 0.78 (0.636–0.945) 0.012 P Value Hylek, JACC, 2014 Major Bleeding in Patients with Atrial Fibrillation Receiving Apixaban or Warfarin in the ARISTOTLE Trial: Predictors, Characteristics, and Clinical Outcomes Major bleeding followed by death within 30 days 237 Hylek, JACC, 2014 Hemorrhagic complications in ED patients receiving dabigatran compared with warfarin Berger, Ann Emerg Med, 2013 Emorragie minori in corso di NAO - Considerare sede e severità della emorragia; eventuale valutazione laboratoristica della attività anticogulante del NAO - Misure locali - Antifibrinolitici - Rimandare, ridurre oppure temporaneamente sospendere la dose successiva del NAO,evitando peraltro prolungate riduzioni o sospensioni della stessa - Identificare e se possibile trattare la causa della emorragia