Advance Care Planning" - Dr. Regina McQuillan, Consultant in
advertisement

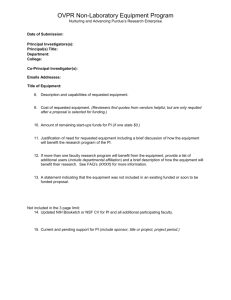
Advance Care Planning Regina Mc Quillan Advance care planning • • • • • What? Who? Why? When? Where? Medical Council Guidelines Paragraph 41.1 Sometimes patients might want to plan for their medical treatment in the event that they become incapacitated in the future. This might include an advance refusal of medical treatment and/or a request for a specific procedure. However, you are not obliged to provide treatment that is not clinically indicated for a particular patient Paragraph 41.2 An advance treatment plan has the same ethical status as a decision by a patient at the actual time of an illness and should be respected on condition that: The decision was an informed choice The decision covers the situation that has arisen The patient has not changed their mind Paragraph 41.3 If there is doubt about the existence of an advance care plan, the patient’s capacity at the time of making the treatment plan or whether it applies in the present circumstances, you should make the decision based on the patient’s best interests. In making such a decision, you should consult with any person with legal authority to make decisions on behalf of the patient and the patient’s family if possible. What? • Values and beliefs • Health care decision, including requests for treatment, refusal of treatment • Preferred place of care • ‘nominee’ for consultation Who? • Patient • Healthcare team-doctor, nurses, social workers • Family When? • Diagnosis of an illness in which there is likely to be loss of capacity • Diagnosis of an illness, when there are likely to be complications needing urgent treatment for example respiratory failure in MND, cardiopulmonary arrest • Disease progression indicators • Hospital admissions Where? Ideally in usual place of care, with usual supports Why? • • • • To respect patient’s wishes To improve end of life care To provide clarity for professionals and carers To reduce health care costs Why not? • • • • Consistency of wishes Undermine doctor-patient trust Institutional agenda-cost Coping mechanism of patients Consistency of wishes Patients were more likely to accept treatment resulting in certain diminished states of health, including pain, as time progressed and health deteriorated. (Fried et al. Prospective Study of Health Status Preferences and Changes in Preferences Over Time in Older Adults. ArchIntMed, 166, 890-5, 2006) Consistency of wishes Conflicting studies, but raise the question of when advance care plans be reviewed Undermine Staff-Patient Trust • Fear of over-aggressive treatment • Fear of medical paternalism • Duty of doctor to act in the patient’s best interests Institutional agenda Cost containmentfrequent emphasis on withholding and withdrawing treatment with the intention to reduce costs Patients’ coping mechanisms • Avoidance • Denial ( Advance planning considerations • • • • • Autonomy Functional capacity Informed decision Not obligatory Cannot oblige futile or unethical or illegal treatment Advance planning considerations • Rarely urgent-a process over a number of encounters • Fit for purpose-not so vague as to be useless • Documented in such a way as to be available when needed • Encourage engagement with family Statement of values and beliefs Specific statements about treatment refused • An advance decision to refuse treatment Specific statements about treatment requested • Can be requested, but not enforced Specific statements about treatment requested • Can be requested, but not enforced • Futile treatment Specific statements about treatment requested • Can be requested, but not enforced • Futile treatment • Respect for autonomy of others Specific statements about treatment requested • • • • Can be requested, but not enforced Futile treatment Respect for autonomy of others Fair use of resources Advance Care Planning • Part of current care planning • At patient’s request and pace • If patient does not have capacity, with those who understands patient’s wishes • In patient’s best interest • Document.