Future - VCU School of Medicine
advertisement

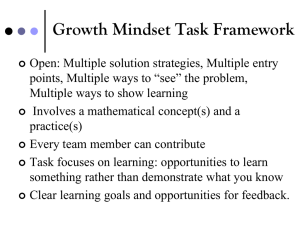
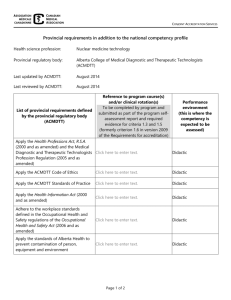
The “Future” of Didactics Kathryn Andolsek MD, MPH Duke University Hospital Graduate Medical Education Imagine the best didactic experience you ever had? Goal • Anticipate expectations for “didactics” • Develop creative, feasible, cost- effective options Didactics • Definition • Impact on Learning • What ACGME really requires • Possible “options” • New content • Competency Didactics– Defined: (ACGME 9/29/2010 glossary) • Didactic: A kind of systematic instruction by means of planned learning experiences such as conferences or grand rounds • GME: period of didactic and clinical education in a specialty…. Evidence Based Educational approach • Limited evidence of impact of Traditional lectures • On- line learning “as good” • Refocus from “strategy” to outcome Adult Learning Theory (with thanks to Malcolm Knowles) • Active Learning – Problem/case based – interaction associated = better achievement & retention of information – Best ways of learning = • Doing • Teaching others • “Just in time” learning – Virtual and or simulation environments • Capacity of learner to access and integrate multiple sources of information (this generation may be the best at multi-tasking) Bligh, 2000 Institutional Requirements CPR (new) • PD must…oversee and ensure the quality of didactic & clinical education in all sites II.A.4.a (IM) • … curriculum must contain the following educational components: regularly scheduled didactic sessions IV.A.3…….. • learning objectives …must: be accomplished through appropriate blend of supervised patient care responsibilities, clinical teaching and didactic educational events VI.A.4.a) IMDidactics • Regularly Scheduled Didactic sessions IV.A.3 • Must include a didactic program. based upon core knowledge content IV.A.3.a. – May include lectures, web-based content, pod casts IV.A.3.a.1 • Program must afford each resident an opportunity to review all of the core curriculum topics IV.A.3.a.1 • Residents must have opportunity to participate in – – – – – morning report, grand rounds, journal club, and M and M (or quality improvement) all of which must involve faculty IV.A.3.a.2 • Program must provide opportunities for residents to interact with other residents and faculty in educational session at a frequency sufficient for peerpeer and peer-faculty interaction VI.A.3.a.3 • Didactic and clinical education must have priority in the allotment of residents’ time and energy VI.A.3 Surgery didactic sessions: • The education of surgeons. encompasses both didactic instruction in the basic and clinical sciences + procedural skills and operative techniques Int.A. • Regularly Scheduled Didactic sessions IV.A.3 • Increases in resident complement: documentation of adequate clinical material and complex operative cases and quality didactic education III.B.2.b) • Regularly scheduled didactic sessions IV.A.3 • Didactic and clinical education must have priority in the allotment of residents’ time and energy VI.A.3 Didactics • opportunity to review • opportunity to participate in – – – – – morning report, grand rounds, journal club, and M and M (or quality improvement) all of which must involve faculty • opportunities for residents to interact with other residents and faculty • Core content of anything specified by RRC Generation Y (1982-1998) Capturing Lectures • • • • • Audacity Camtasia Lectopia Panopta And more…. Duke iTunesU www.itunes.duke.edu Duke itunesU Public Material Login for Classes • Net ID protected • Invitation only GME iTunesU Wiki • Website allowing numerous people access for edits • Restriction options for viewing, editing, etc. • Examples: – Meeting agenda and minutes – Program Information managed by residents (ex. Pathology) – Project Committee Organization – Group work – Lecture series (ex. Health Policy) Health Policy Lecture Series Example Links from Wiki • Roster • Lecture Schedule • Presenter Bio • Presenter Photo • Readings • iTunesU • Evaluation • Post-test New Content • • • • • • • Professionalism Personal Responsibility Patient Safety Transitions of Care Alertness Management/Fatigue Mitigation Supervision Teamwork Other On-line Resources • LIFE Curriculum – www.LIFEcurriculum.com – Trigger Scenarios • MedEdPortal – www.aamc.org/mededportal • AMA Electronic Ethics Journal (virtual mentor) – http://virtualmentor.ama-assn.org/ Didactics • Definition • Impact on Learning • What ACGME really requires • Possible “options” • New content • Competency FAQs, Possible pertinence to Didactics • • • • • • Duty hours are defined as all clinical and academic activities related to the program; i.e., patient care (both inpatient and outpatient), administrative duties relative to patient care, the provision for transfer of patient care, time spent in-house during call activities, and scheduled activities, such as conferences. Duty hours do not include reading and preparation time spent away from the duty site. VI.G.1. Max Hours work per week Duty hours do not include reading, studying, and academic preparation time, such as time spent away from the patient care unit preparing for presentations or journal club . Any tasks related to performance of duties, even if performed at home, count toward the 80 hours. Residents who have satisfactorily completed the transition of care may, at their discretion, attend an educational conference that occurs during the four hours VI.G.4.b) Max Duty Period Length The goal of the added hours at the end of the on-call period is to promote didactic learning and continuity of care If attendance (at a conference) is “strongly encouraged,” the hours should be included because duty hours apply to all required hours in the program, and it is difficult to distinguish between “strongly encouraged” and required. Another way to look at it is that such a journal club, if held weekly, would add two hours to the residents’ weekly time. A program in which two added hours result in a problem with compliance with the duty hour standards likely has a duty hour problem Duty Hours limits and Research and Other Non-Patient Care Activities References • • • • • • • Andolsek KM, Murphy G, Pinheiro S, Petrusa E, Tuck T, Weinerth J. Efficacy and Efficiency of Webcast Orientations Versus Live Resident Orientations: Results of a 2Year Survey. Journal of Graduate Medical Education: March 2010; 2(1): 136-140. Casebeer L Andolsek K Abdolrasulnia M Green J Weissman N Pryor E Zheng S Terndrup T Evaluation of an online bioterroism continuing medical education course. J Contin Ed Health Profes 2006;26(2):137-44 Cook DA Garside S Levinson AJ Dupras DM Montori VM What do we mean by webbased learning? A systematic review of the variability of interventions. Med Educ 2010 Aug,44(8):765-75 Cook DA Levinson AJ Garside S Dupras DM Erwin PJ Montori VM Instructional design variations in internet-based learning for health professions education: a systematic review and meta-analysis Acad Med 2010 May,85(5):909-22 Cook DA Levinson AJ Garside S Time and learning efficiency in Internet-based learning: a systematic review and meta-analysis Adv Health Sci Educ Theor Pract 2010 Dec, 15(5):755-70 Epub 2010 May 13 Cook DA Levinson AJ Garside S Dupras DM Erwin PJ Montori VM Internet-based learning in the health professions: a meta-analysis JAMA 2008 Sept 10, 200(10:118196 Cook DA Gelula MH Dupras DM Schwartz A Instructional methods and cognitive and learning styles in web based learning: repot of two randomized trials Med Educ 2007 Sep 4(9):897-905 References • Cook DA Web-based learning: pros, cons and controversies. Clin Med 2007 Jan-Feb, 7(1):37-42 • Cook DA Where are we with Web-based learning in Medical education? Med Teach 2006; Nov, 28(7):594-8 • Cook DA Learning and Cognitive styles in web based learning: theory, evidence and application. Acad Med 2005 Mar 80(3):286-78 • Darling-Hammond L, Youngs P. Defining highly qualified teachers: What does scientifically-based research actually tell us? Educ Res 2002;31:13-25. • David TH Wagner GS Gleim G Andolsek KM Arheden H Austin R CourtneyEighmy Gradison M Leist JC Maynard C Noga EM Ostbye T Eisenstein EL Probloem based learning of research Skills J Electrocardiol 2006;Jan 39(1):120-8 • Griner PF, Danoff D. Sustaining change in medical education. JAMA, 2000;283(18)2429-2431 • Hatem CJ, Lown BA, Newman LR. The academic health center coming of age: Helping faculty become better teachers and agents of educational change. Acad Med. 2006;81:941-944. References • • • • • • • • • Nagler A Andolsek K Dossary K Schlueter J Schulman K Med Teach 2010;32(12)e559-65 McLean M. Rewarding teching excellence. Can we measure teaching excellence? Who should be the judge? Med Teac 2001;23:6-11. McKimm J Jollie C Cantillon P ABC of learning and teaching.: web based learning. BMJ 2003;326(7394):870-873 Morzinski JA, Fisher JC. A nationwide study of the influence of faculty development programme in teaching skills. Med Educ. 2007;41:592-600. Ruiz JG Mintzer MJ Leipzig RM The impact of e-learning in medical education. Acad Med 2006 81(3):207-212 Sandars J Morison C What is the Net Generation? The challenge for future medical Education. Med Teach 2007;29(2):85-88 Steinert Y, Mann K, Centeno a, et al. A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education. Med Teach 2006;28:497-526. Swanwick T. See one, do one, then what? Faculty development in postgraduate medical education. Postgrad Med J 2008;84:339-343. Young L, Orlandi A, Galichet B, Heussler H. Effective teaching and learning on the wards: easier said than done? Med Educ 2009;43(8):808-816.