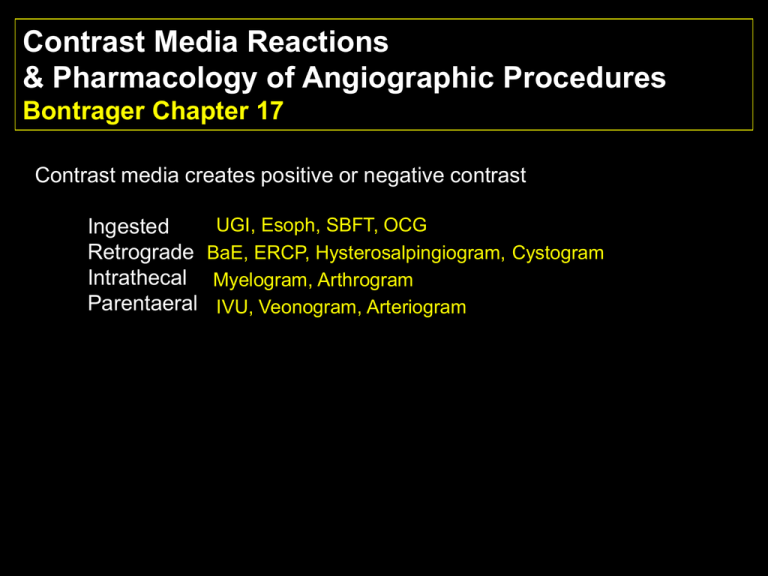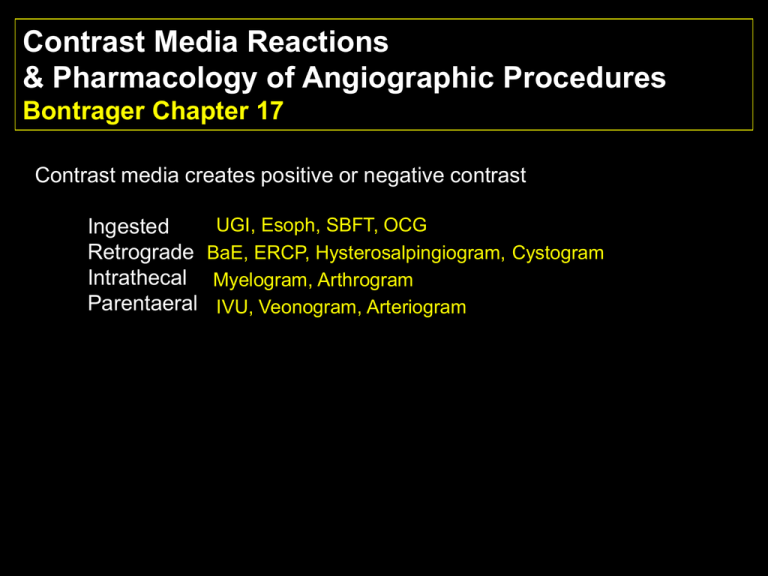
Contrast Media Reactions
& Pharmacology of Angiographic Procedures
Bontrager Chapter 17
Contrast media creates positive or negative contrast
Ingested
Retrograde
Intrathecal
Parentaeral
UGI, Esoph, SBFT, OCG
BaE, ERCP, Hysterosalpingiogram, Cystogram
Myelogram, Arthrogram
IVU, Veonogram, Arteriogram
127
Iodine 53
Iodine: atomic number 53.
Essential for nutrition, abundant in thyroid.
Principle ingredient in the surgical scrub, betadine
Non-metallic, commonly found in salt water swamps or brackish waters,
in grayish-black, lustrous plates or granules.
A halogen (group VII elements including fluorine, bromine, and chlorine),
iodine readily binds to salt.
Original “ionic” iodine contrasts were bound to sodium or meglumine
salt. When injected, the molecule begins to disassociate, releasing ionic
particles (+ cation and - anion) at a concentration 4 to 8 times higher
than the particle content of blood (Osmolality).
Characteristics of Ionic Contrast
Iodine concentration determines the radiopacity of the agent.
Measured in %weight/volume. Ranges from 10 to 82, dependent on its
use. Many products include the concentration of iodine salts in the
brand name: Renografin-60, Hexabrix 76, Isovue-200 (20%). See
appendix L in Patient Care in Radiography.
Water soluable. Unlike barium in suspension, iodine preparations must mix
with blood.
Stable in solution. The iodine molecule must remain in solution. Products
that do not meet this requirement are packages as a solute, and solvent.
Low viscosity. The thickness of an agent significantly affects the ease in
which a bolus is injected, and the rate of drip infusion.
Low toxicity. Any preparation not natural to the body is toxic to some degree,
as are natural substances given in excess. The goal of contrast media is to
keep adverse reactions to a minimum.
Low osmolality. The number of particles in solution is the chief factor of
toxicity.
Chemical Composition
I
Chemical composition of ionic contrast media
I
Six sided Benzyl ring: Tri-iodinated Benzoic acid
I
Benzoic acid. White crystiline acid in benzoin (from the resin of
the kincense tree, also found in cranberries). Used as a preservative
and binding agent in food medicine, and perfume.
127
Iodine 53
Iodine: atomic number 53. 3 x denser than bone, 5 x denser than soft
tissue
Essential for nutrition, abundant in thyroid.
Principle ingredient in the surgical scrub, betadine
Non-metallic, commonly found in salt water swamps or brackish waters
in grayish-black, lustrous plates or granules.
A halogen (group VII elements including fluorine, bromine, and chlorine),
iodine readily binds to salt.
Six sided Benzyl ring of ionic contrast: Tri-iodinated Benzoic acid
“Ionic” iodine contrasts are bound to sodium, calcium, magnesium, or
meglumine salts.
The concentration of ionic contrast refers to the amount of salt in solution
When injected, the molecule begins to dissociate, releasing ionic particles
(+ cation and - anion) at a concentration 4 to 8 (3-10) times higher than the
particle content of blood
Terms: Osmolality, Isotonic, Hypertonic, Chemotoxicity, Osmotoxicity.
Normal capillary action
(Balance of blood and osmotic pressure)
= RBC
*
BP>OP
arteriole
*
*
= proteins
OP>BP
*
*
H 20
H 20
*
venule
The Osmotic Effect
1. As contrast
is injected
osmolality
increases
2. Blood entering the
capillary bed is
hypertonic to the
fluid in the surrounding
tissues.
6. Flexibility of vessels walls
allow vasodilation to accomodate
hypervolemia.
3. Extravascular fluid
crosses the semipermeable membrane of
the capillary to achieve
isotonicity, causing
hypervolemia
4. Fluid
drawn
from
RBCs
causes
sickling.
5. Epithelial cells lining the intimal
wall are similarly effected, and can
lead to inflammation and
thrombophlebitis
Ionic versus Nonionic Contrast
Ionics: Dissociate into + and – particles
High osmolality (2-8 x)
Disrupts electrolyte balance
Nonionic contrast substitutes noniodine parts of the benzoic ring with
a nonionizing side chain.
Nonionics: Do not dissociate
2 x blood plasma
Electrolyte balance maintained
Costs 10-20 times more
Higher viscosity
Osmolality of plasma = 300 millimoles/kg
“
“ nonionics = 750
“
“
“
ionics = 1000-2400
Nonionic, low-osmolality contrast agents (LOACs)
Quickly became popular in the late 1980s
Nonionics do not dissociate. Fewer particles means lower osmolality
than ionics. The cost is significantly greater, but comes with the
promise of fewer contrast reactions.
From Patient Care in Radiography,
5th edition. pg.269.
Contrast Reactions
Classified as Mild, Moderate, Severe and Fatal
4 Types of reactions
1. Vasomotor reactions: result from
the actions of nerves that innervate
vessel walls.
Urticaria or hives result from
bug bites (single), from allergic
reactions they range from
scattered to giant.
increase in impulses = constriction
decrease in impulses = dilation
1. Vasomotor (mild or “normal”)
* feeling warm, flushed
* pallor
* nausea
* mild urticaria
* anxiety
* syncope (preceded by dizziness, lightheadedness)
Contrast Reactions
Classified as Mild, Moderate, Severe and Fatal
4 Types of reactions
2. Anaphylactic reactions:
2. Anaphylactic (true allergic reaction)
Sudden release of immunilogic
* can resemble vasomotor
mediators (antibodies from
* can escalate
previous exposures) starts a
* Edema (larynx) laryngospasm
cascade effect, Not dose related
* Asthma like signs
* Moderate to severe urticaria
* vasodilation
(giant hives)
* permeability of capillaries
* Angioedema
* Smooth muscle spasm
* Hypotension
* urticaria
* Tachycardia
Contrast Reactions
4 Types of reactions
Vagus, 10th
cranial. Known
as the “wandering
nerve.”
3. Vasovagal reactions (severe)
* Interference with cardiac conduction
* Dysrhythmia
* Hypotension
* Absent pulse
* Convulsions
Contrast Reactions
Classified as Mild, Moderate, Severe and Fatal
4 Types of reactions
4. Acute renal failure
* Anuria
* Torpor
* Disorientation
Apathy, inactivity
sluggishness
Contrast Reaction Treatments
1. Vasomotor (“normal”)
* feeling warm, flushed
* nausea
* mild urticaria
Treatment: Reassurance, monitoring,
Diphenhydramine (Benadryl) for hives.
Benadryl is an antihistimine used for
anaphylactic reactions.
Patients with a known sensitivity may
be administered Benadryl before the
procedure
Contrast Reaction Treatments
2. Anaphylactic (true allergic reaction)
* can resemble vasomotor
* can escalate
* Edema (larynx)
* Asthma like signs
* Giant Hives
* Hypotension, tachycardia
Treatment: Epinephrine (IV best)
beta z agonist when epi fails
Benadryl
Tagamet/Zantac
IV fluid (rapid)
O2
Corticosteroids
Epinephrine for bronchospasm.
Vasodilator for hypotension
Agonists = drugs that mimic
the bodies regulatory functions.
Beta agonists treat COPD,
asthma. Beta z stimulate
bronchodilation
Steroids = sex hormones
Cortico = from cortex of
adrenal gland (or synthetic)
Treats inflammation, asthma
dermatitis.
Contrast Reaction Treatments
3. Vagal reactions
* Interference with cardiac conduction
* Dysrhythmia
* Bradycardia
* Hypotension
* Absent pulse
* Convulsions
Treatment: Epinephrine IV
Atropine IV
Lidocaine IV
O2
Sodium Bicarbonate
Diazepam (Valium) IV
Atropine for bradycardia
Sodium Bicarb for
metabolic acidosis
Valium for spasm, convulsions,
anxiexty
Contrast Reaction Treatments
4. Acute renal failure
* Anuria
* Torpor
* Disorientation
Conservative to aggressive treatment
What two labs tests measure renal function?
Creatinine .6-1.5 mg/ml serum
BUN 8-20 mg/ml serum
Preparing to inject
* Stock should be rotated, lots not mixed
* Inspect vial before drawing up. Assure correct media,
check color, expiration date, flaws in glass.
* Do not swab rubber stoppers of unopened vials.
* Patient history and allergies
* Previous injection of contrast without problem does not
preclude a reaction
* Previous reactions do not guarantee subsequent
reactions, but are deemed high risk
* Do not discard vials until after the case
Contraindications:
Glucophage – med for diabetes mellitus. When combined with
contrast increases the risk of renal failure. Recommended to
be withheld 48 hrs prior to and following contrast administration
Multiple myeloma - Malignancy of bone that leads to renal failure, and
increases the risk of contrast reactions.
Azotemia (uremia)- High levels of nitrogen waste in blood. Laboratory
tests BUN (blood urea nitrogen) should be 8 – 25 mg/100 ml. Another
test for nitrogen waste, Creatinine levels, should be .6 to 1.5 mg/dl.
Contraindications continued:
Hypersensitivity to iodine
Anuria – no excretion of urine
Severe renal disease or failure
Congestive heart disease (CHF)
Sickle cell anemia
Pheochromocytoma – tumor of the kidney
In certain cases, an IVU may be performed despite contraindications.
Patients should be well hydrated to lessen the risks.