Fournier’s gangrene
Dr. Vinod Jain
26.08.2014
Fournier’s gangrene
•
•
•
•
•
•
•
•
Definition
Etiology & risk factors
Pathogenesis & pathology
Incidence
Clinical features
Differential diagnosis
Investigations
Treatment –
- Medical
- Surgical
• Complications
Definition
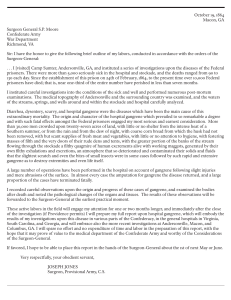
Named after French venereologist
Jean Alfred Fournier (1883).
Fournier gangrene is defined as a
polymicrobial necrotizing fasciitis
of the perineal, perianal, or genital
areas.
Etiology & risk factors
• Initially described as idiopathic
• Now in more than 75% cases
inciting cause in known
• Necrotizing process commonly
originates from infection in
anorectum, urogenital tract or skin
of genitalia
Etiology
1. Ano-rectal causes –
– infection in the perineal glands
– Manifestation of colorectal injury,
malignancy or diverticulitis
2. Uro-genital causes –
– infection in the bulbourethral glands
– urethral injury
– Iatrogenic injury
– Lower urinary tract infections
Etiology (contd.)
3. Dermatologic causes –
–
–
–
Hidradenitis suppurativa
Ulceration from scrotal pressure
Trauma to scrotum or perineum
4. Other less common causes –
–
–
–
Consequence of bone marrow
malignancy
Systemic lupus erythematosus
Crohn’s diseases
Risk factors
•
•
•
•
•
•
•
•
Diabetes mellitus
Alcoholism
Malignancies
Cirrhosis Liver
Chronic steroid use
HIV infection
Malnutrition
Morbid Obesity
Causative Bacteria
•
•
•
•
•
Polymicrobial infection
Minimum of four isolates per case
Most common aerobe – E. coli
Most common anaerobes – Bacteroids
Others – Streptococcus, Staphylococcus,
MRSA – Methicillin Resistant
Staphylococcus aureus, Klebsiella
Pseudomonas, Proteus & Clostridium.
Pathogenesis
• Bacteria act synergistically causing
obliterative endarteritis & production of
various enzymes causing destruction
• There is imbalance between host
immunity & virulence of organism
Mechanism of spread
Entry of bacteria (act through synergism)
Fibrinoid coagulation of nutrient vessels
Decreased locally blood supply to skin
Decreased tissue oxygen tension
Growth of anaerobes & microaerophilic
organisms
Production of enzyme (Collagenase,
Lecithinase, Hyaluronidase )
Digestion of fascial barrier
Rapid spread of infection
Pathology
•
•
•
•
•
Pathognomonic findings on pathological
evaluation of tissue are :Necrosis of superficial & deep fascial planes
Fibrinoid coagulation of the nutrient
arterioles
Polymorphonuclear cell infiltration
Presence of micro organisms with in the
involved tissues
Air in the perineal tissue
Incidence
• Age
• Sex
– 30 – 60 years
– 10 times more common in
males
• Social habits – More common in male
homosexuals (more prone
for Rectal injury)
Clinical features
•
•
•
•
•
•
•
Begins with insidious onset of pruritus and
discomfort of external genitalia
Prodromal symptoms of fever and lethargy, which
may be present for 2-7 days before gangrene
The hallmark of Fournier gangrene is out of
proportion pain and tenderness in the genitalia.
Increasing genital pain and tenderness with
progressive erythema of the overlying skin
Dusky appearance of the overlying skin;
subcutaneous crepitation; feculent odor
Obvious gangrene of a portion of the genitalia;
purulent discharge from wounds
As gangrene develops, pain subsides (Nerve necrosis)
Differential diagnosis
•
•
•
•
•
•
•
•
•
Balanitis
Cellulitis
Epididymitis
Gas gangrene
Compicated hernias
Complicated hydrocele
Necrotizing fasciitis
Orchitis
Testicular torsion
Other Problems to be Considered
•
•
•
•
•
•
•
•
Testicular fracture
Testicular hematoma
Testicular abscess
Scrotal abscess
Vasculitis
Warfarin gangrenosum
Polyarteritis nodosum
Wegener’s granulomatosis
Investigations
(CBC) Complete blood count
Electrolytes
BUN / Serum creatinine
Blood Sugar
ABG
Blood and urine culture with sensitivity
Coagulation profile for DIC
Investigations (contd.)
Imaging
Conventional radiography
Ultrasonography
C.T. Scanning
MRI
Conventional radiography
• Consider where clinical findings
are inconclusive
• Presence of gas in soft tissue
Ultrasonography
• Can be used to detect fluid or
gas in soft tissue
• “Sonographic hallmark” –
Presence of gas in scrotal
tissue
• Excludes other conditions
• Testicular blood flow - N
• Limitations – Direct pressure on
involved tissue causes
inconvenience
C.T. Scanning
• Can detect smaller amount of
soft tissue gas
• Defines extent more specifically
• Identifies underlying causes eg.
Small perineal abscess
MRI
• Yields greater soft tissue details
• Create logistic challenges,
especially in critically ill
patients
Treatment
• Medical
• Surgical
Medical Treatment
1.
2.
3.
Restoration of normal organ perfusion
Reduction of systemic toxicity
Broad spectrum antibiotics to cover anaerobes as well
(cipro+clinda+metro)
4. Vancomycin for MRSA
5. Tetanus prophylaxis
6. Irrigation with super oxidised water
7. Hyperbaric oxygen therapy
8. IV immunoglobulins to neutralize super antigen as
streptotoxin A & B (as adjuvant)
9. Antifungal – if required
10. Non – conventional
- Unprocessed honey – enzyme action
- dressing with gauge soaked with zinc per oxide
Surgical treatment
• Repeated aggressive debridement
• Preservation of testes (subcutaneous
pocket from desiccation)
• Reconstruction after infection is over
• Fecal diversion
• Urinary diversion
• Vacuum assisted closure (VAC)
Complications
•
•
•
•
•
•
ARF
ARDS
Septicemia and gram negative shock
MSOF
Tetanus
Death
Questions ?
Let us revise
•
•
•
•
•
•
•
•
Definition
Etiology & risk factors
Pathogenesis & pathology
Incidence
Clinical features
Differential diagnosis
Investigations
Treatment –
- Medical
- Surgical
• Complications