DISORDERS OF GAIT
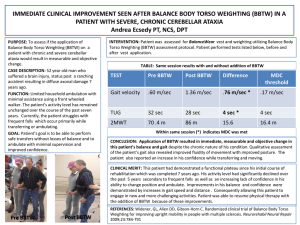
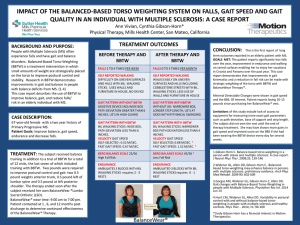
advertisement

Practical approach to the assessment of gait: watch the patient walk along a stretch of corridor and observe the characteristics of the gait.Note the following: -Whether the patient walks unaided:if not,does the patient walk with a stick or crutches?. -Whether the patient walks in a straight line:patients who are ataxic are unsteady and may be unable to tandem walk i.e.heel-to-toe walking. -Normal arm swing: arm swing may be reduced in patients who have an extra-pyramidal syndrome.This may be more marked on one side than the other,especially in idiopathic Parkinson’s disease. -Turning around:patients who have an extrapyramidal syndrome or ataxia perform this with difficulty. -Standing and walking on the toes(S1)and then heels(L5):patients with a common peroneal nerve palsy and L5 or S1 radiculopathy will find this difficult,as will patients with a hemiparesis. -Perform Romberg’s test:ask the patient to stand with feet together and eyes closed.The test is positive if the patient is more unsteady with eyes closed than with eyes open.This occurs in patients with a sensory ataxia who have impaired proprioception.It cannot be tested reliably in patients with a cerebellar disorder or moderate to severe weakness from any cause as the patient will be unsteady irrespective of whether there is sensory ataxia. Differential diagnosis of disorders of gait Gait of cerebellar ataxia: Patients with cerebellar ataxia stand and walk unsteadily,as if drunk.They soon begin to compensate for this by adopting a broad base with feet further apart(fig).The gait is unsteady ,with irregularity of stride. The trunk sways and the patient may veer towards one side.In mild cases,the only manifestation of gait disturbance may be difficulty walking heel-to-toe in a straight line(i.e. tandem walking). On neurological exam there may also be nystagmus,dysarthria and cerebellar signs in the limbs.Ataxia may be confined to the gait when the cerebellar lesion is in the midline. Cerebellar ataxia(cont’d) Causes include: -Multiple sclerosis -Vascular disease (ischemic,hemorrhagic, AVMs) -Alcoholic cerebellar degeneration -Anticonvulsant therapy : carbamazepine, phenytoin -Posterior fossa tumours -Cerebellar paraneoplastic syndrome -The hereditary cerebellar ataxias. Hemiparetic gait Patients with a hemiparetic gait have a characteristic posture on one side,of flexion and internal rotation of the upper limb and extension of the lower limb(fig).The leg moves stiffly and is swung around in a semicircle to avoid scraping the foot across the floor.However such scraping does occur to some extent and the toe and outer sole of the shoe become worn. Causes include:cortical or internal capsule strokes,cerebral hemispheric tumour and traumatic lesions. Spastic gait A spastic gait is seen in patients who have a spastic paraparesis or bilateral hemiparesis.The legs move slowly and stiffly and the thighs are strongly adducted such that the legs may cross as the patient walks or “scissor gait”. Causes of spastic gait: -Spinal cord compression. -Trauma/spinal surgery. -Birth injuries or congenital deformities: cerebral palsy,spina bifida. -Multiple sclerosis. -Motor neuron disease. -Parasagittal meningioma. -Subacute combined degeneration of the cord. Parkinsonian gait The patient often has a stooped and flexed posture with loss of arm swing,which is almost always more marked on one side in idiopathic Parkinson’s disease(figs).The steps are short and the patient shuffles. There may be difficulty starting and stopping.Turning may occur “en bloc”(i.e. not smoothly but in stiff stuttering movements).Having started to walk,the patient leans forward and the pace quickens,as though the patient is attempting to catch up on himself or herself(festinant gait). Gait of sensory ataxia Sensory ataxia arises from impaired proprioception caused by a lesion of the peripheral nerves,posterior roots,dorsal columns in the spinal cord or rarely the ascending fibres to the parietal lobes.The gait is unsteady and wide-based and often stamping (fig).Romberg’s test is positive and there is impaired perception of joint position on examination of the lower limbs. Causes of sensory ataxia: *Posterior spinal cord lesions: -Multiple sclerosis - Cervical spondylosis - Tumours - Vitamin B12 deficiency - Tabes dorsalis *Sensory peripheral neuropathies include: -hereditary:Charcot-Marie-Tooth disease -metabolic:diabetes -inflammatory:Guillain-Barre syndrome -malignancy:myeloma,paraneoplastic syndrome -toxic:alcohol,drugs(e,g. isoniazide) Steppage gait Steppage gait arises from weakness of the pretibial and peroneal muscles of lower motor neuron type.The patient has footdrop and is unable to dorsiflex and evert the foot(fig).The leg is lifted high on walking so that the toes clear the ground.On striking the floor again,there is a slapping noise.Shoe soles are worn on the anterior and lateral aspects. Causes of steppage gait: -Charcot-Marie-Tooth disease(bilateral footdrop) - -Common peroneal nerve palsy e.g.from a fibular fracture(unilateral footdrop) - Anterior horn cell disease e.g. polio,motor neuron disease (often asymmetrical footdrop) Myopathic gait Myopathic gait ic the so-called waddling gait caused by weakness of the proximal muscles of the lower limb girdle.The weight is alternately placed on each leg,with the opposite hip and side of the trunk tilting up towards the weight-bearing hip,which sways outward,with the opposite pelvis dropping as does the trunk on that side. Causes of waddling gait: Muscular dystrophies:Duchenne’s,Becker’s, limb-girdle,facio-scapulo-humeral. - -Metabolic myopathies:periodic paralysis,hypo- and hyperkalemia. - -Endocrine myopathies:Cushing’s disease Addison’s disease,hypo- and hyperthyroidism. -Inflammatory myopathies:polymyositis and dermatomyositis. Apraxic gait Diseases of the frontal lobes gives rise to an apraxic gait.The patient walks with feet placed apart and with small hesitant steps,which may be described as ‘walking on ice’ or ‘marche a petit pas’.There is difficulty with initiation of walking and,in advanced cases,it may seem as though the patient’s feet are stuck to the floor . There are no abnormalities of power,sensation or coordination.There may be other signs of frontal cortical dysfunction(e.g. grasp or rooting reflex);the tendon reflexes may be brisk and the plantar responses extensor. Causes of apraxic gait include: - Bilateral subcortical cerebrovascular disease - Normal-pressure hydrocephalus - Frontal lobe tumours e.g. meningioma -Frontal subdural hematomas(rare; bilateral usually) -Advanced Alzheimer’s disease. Antalgic gait Antalgic gait arises from pain(e.g.a painful hip or knee due to arthritis).The patient tends to bear weight mainly on the unaffected side,only briefly putting weight onto the affected side. Functional gait A functional ,hysterical or non-organic gait arises from psychological or behavioural disturbance.It does not conform to any descriptions given above.It can take a number of forms and is variable in character.There are no objective abnormal neurological signs on formal examination. Functional gait(cont’d) There are often other positive features of an underlying psychiatric disturbance. However,the only manifestation of a midline cerebellar lesion may be severe ataxia of gait and stance,with normal limb signs on formal examination and this can sometimes be mistaken for a non-organic illness. The character of a patient’s gait will provide clues to the clinical signs that might be expected on further neurological exam. The abnormal types of gait are: *Ataxic:broad-based and unsteady. *Hemiplegic:unilateral flexed posture of the upper limb and extended posture of the lower limb. *Spastic:’scissoring’ posture of the legs. *Parkinsonian:stooped posture,shuffling small stepped gait with loss of arm swing. *Sensory ataxia:high stepped ‘stamping’ gait. *Steppage:footdrop. *Myopathic:’waddling’gait. *Apraxic:hesitant ‘walking on ice’ gait. *Non-organic:bizarre and variable.