Osteopathic Consideration for the Elderly Patient, Joy Palmer, D.O.
advertisement

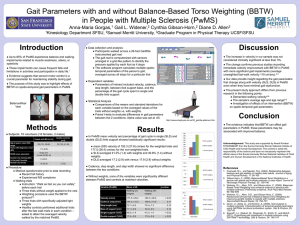
Joy Palmer, DO Edward Via College of Osteopathic Medicine VOMA Spring CME Conference May 2010 Objectives Understand the physiology of balance and gait Understand the influence of normal aging processes on balance and gait Understand the influence of common disease processes on balance and gait Review of literature Osteopathic considerations in keeping our patients up-right and moving; including review of physiologic models and treatment approaches Physiology of Balance Visual Eyes to visual Cortex Vestibular system Inner ear to Brainstem Somatic sensory (joints) Skin-muscles-joints to Spinal cord Physiology of gait Cerebrum frontal, occipital, parietal, thalamus, basal ganglia Cerebellum Coordination of vestibular and proprioceptive function Walking cycle Upper extremities, thorax, lumbars, innominate, sacrum, lower extremities Age-related changes to balance Visual Visual acuity, depth perception, contrast sensitivity, dark adaptation. Use of multi-focal lenses increases risk of falls Vestibular Labyrinthine hair cells diminish, loss of vestibular ganglion cells, loss of nerve fibers Somatosensory proprioceptive sensitivity decreases: decrease in mm mass, decreased ability to make modifications in joint play, decreased ability to send message about joint position Risk factors for falls Past history of a fall Psychotropic drug use Lower extremity Arthritis weakness Age Female gender Cognitive impairment Balance problems Hx of stroke Orthostatic hypotension Dizziness Anemia Age-related changes to gait IT IS NOT “NORMAL” AGING TO HAVE CHANGES IN GAIT Disease-related changes to gait Acute injury Fractures Spinal stenosis Chronic disease Arthritis Diabetes Obesity Postural hypotension Spinal stenosis Chronic pain Neurologic Movement disorders Stroke Visual changes White matter changes Gait Classifications Gait classification Hypokinetic-rigid gait disorder Antalgic gait Paretic / Hypotonic Sensory ataxic Cautious gait Careless gait Hypokinetic-rigid gait Main features of gait: Shuffling; slow, short stride reduced step height hesitation and freezing Specific gait or balance test: improves with external cues aggravated by secondary task Assoc sxs and signs: bradykinesia; resting tremor Antalgic gait Main features of gait: Limping Assoc sxs and signs : Pain Limited range of movements Paretic / hypotonic gait Main features of gait: High steppage Dropping foot Waddling Specific gait or balance test: Trendelenburg’s sign Assoc sxs and signs : Weakness Atrophy Low to absent DTRs Sensory ataxic gait Main features of gait: Staggering Wide-based Specific gait or balance test: Aggravated by eye closure Assoc sxs and signs : Disturbed proprioception Cautious Gait Main features of gait: Slow, wide base, short steps Marked improvement with external support Assoc sxs and signs : Mild to moderate postural instability Excessive fear of falling Careless Gait Main features of gait: Speed is inappropriately fast Motor “recklessness” Commonly seen in: Huntington’s Alzheimer’s Confusion / delirium Review of Literature Review of literature Manchester D et al. Visual, Vestibular and Somatosensory Contributions to Balance Control in the Older Adult. J of Gerontology, 1989; 44(4). Baezner H. et al. Association of gait and balance disorders with age-related white matter changes – The LADIS Study. Neurology, 2008; 70. Patel M, et al. Change of Body Movement Coordination during Cervical Proprioceptive Disturbances with Increased Age. Gerontology, 2009. Review of literature Katsura Y, et al. Effects of aquatic exercise training using water-resistance equipment in elderly. Eur J Appl Physio, 2010; 108. Gill T et al. A Program to prevent Functional Decline in Physically Frail, Elderly Persons Who Live at Home. NEJM, 2002; 347. Madureira M et al. Balance training program is highly effective in improving functional status and reducing the risk of falls in elderly women with osteoporosis: a randomized controlled trial. Osetoporosis International, 2007; 18. Beling J, Roller M. Multifactorial Intervention with Balance Training as a Core Component Among Fall- Prone Older Adults. J of Ger Physical Therapy, 2009; 32. Osteopathic Considerations Osteopathic considerations Whole patient : mind, body, spirit Exercise, physical therapy Osteopathic manipulation Medicinal Treatment models Circulatory-Respiratory Biomechanical/Postural/Tensegrity Viscero-somatic/Somato-viscero Neuro-Endocrine-Immune Bio-energetic Psychosomatic Circulatory-Respiratory Getting nutrients to, removing waste products from Respiratory mechanics Junctional areas are key sites to evaluate and address Osteopathic research and the Respiratory/Circulatory model O-Yurvati et al. Hemodynamic effects of OMT immediately after CABG. JAOA. 2005; 105(10): 475-80. N=29 (10 tx group) Findings: reduced central blood volume, mixed venous oxygen saturation increased, improved cardiac index No particular tx protocol Various modalities utilized Biomechanical Posture and balance Motion Functional anatomy Tensegrity Osteopathic research and the Biomechanical model Ingber D, et al. Journal of Cell Science. 2003. (article in 2 parts) Ingber D, et al. Ann. Rev. of Phys. 1997. Wang, et al. PNAS. 2001. Osteopathic research and the Biomechanical model Cislo S, Ramirez M, Schwartz H. Low back pain: Treatment of forward and backward sacral torsions using counterstrain technique. JAOA. 1991;91(3): 25559. Wynn M, Burns J, Eland D, Conatser R, Howell J. Effect of Counterstrain on Stretch Reflexes, Hoffmann Reflexes, and Clinical Outcomes in Subjects With Plantar Fasciitis. JAOA. 2006;106(9): 547-556. Viscero-somatic / Somato-viscero Facilitated segment VISCEROSOMATIC REFLEXES Reflex loop, bi- directional Wide dynamic range cells Chapman’s reflex Figure 1 Diagram of viscerosomatic reflexes taken from: content.answers.com/.../9/9d/360px- Gray839.png Blue indicates PARASYMPATHETIC INNERVATION Red indicates SYMPATHETIC INNERVATION Research supporting S-V reflex Miranda A, et al. Altered visceral sensation in response to somatic pain in the rat. Gastroenterology. 2004 Apr;126(4):1082-9. Sato Y, et al. Reactions of cardiac postganglionic sympathetic neurons to movements of normal and inflamed knee joints. J Auton Nerv Syst. 1985 Jan;12(1):1-13. Research supporting V-S reflex Stawowy M, et al. Somatosensory changes in the referred pain area in patients with cholecystolithiasis. Eur J Gastroenterol. 2005 Aug;17(8)865-70. Nicholas AS, et al. A somatic component to myocardial infarction. Br Med J (Clin Res Ed). 1985 July 6;291(6487):13-17. Osteopathic Research and the Viscerosomatic/Somatovisceral Beal MC. JAOA. 1983; 82(11): 822-31 & 1985; 85(5): 302-07. Cox J. JAOA. 1983; 82(11): 832-6. N: 97 Results: greatest change in rom at T4, of these participants, 75% had angiogram evidence of CAD Basbaum, Levine. Can J Phsyiol Pharmacol. 1991; 69: 647-651. Foreman, Blair, Ammons. Prog Brain Res. 1986; 67: 39-48. Neuro-Endocrine-Immune Homeostasis vs allostasis Stressful stimuli may be psychological or physiological Hypothalamic-thyroidadrenal-gonadal axis Osteopathic Research and the Neuro-Endocrine-Immune model Celander E. Effect of OMT on Autonomic Tone as Evidenced by Blood Pressure Changes and Activity of the Fibrinolytic System. JAOA. 1968; 67: 1037-38. Basbaum, Levine. Can J Phsyiol Pharmacol. 1991; 69: 647-651. Foreman, Blair, Ammons. Prog Brain Res. 1986; 67: 39-48. Rivers WE, Treffer KD, et al. Short-Tem Hematologic and Hemodynamic Effects of Osteopathic Lymphatic Techniques: A Pilot Crossover Trial. JAOA. 2008; 108(11): 646-651. Bioenergetic Energy expenditure Energy conservation Changes in musculoskeletal system can effect body’s energy requirements. Psycho-somatic Role of limbic system in perception of pain Depression and musculoskeletal pain Treatment Approaches Approaches Direct Indirect Soft tissue Strain-CounterStrain Muscle energy Facilitated Positional Release HVLA Balanced ligamentous Articulatory / Still’s tension / ligamentous articular strain Osteopathy in the Cranial Field Osteopathy in the Biodynamic Field Osteopathy in the Cranial Field Structure of Fascia Structure: Loose areolar vs. dense “irregular” Cellular components Fibroblasts Mast cells Histiocytes etc. (adaptability) Subcellular components Collagen (reticular fibers) Elastic fibers GAG etc. (adaptability) General Properties of Fascia Viscosity Rate of deformation under a load Capability to yield under continual stress Elasticity Ability to recover its shape after deformation Plasticity The ability to retain a shape attained by deformation General Functions of Fascia Mechanical support (vascular & structural) compartmentalization conduit Metabolic Diffusion: gel energy storage: elastic potential energy Immunologic line of defense: lymphoid tissue Barrier: compartments Mechanisms of Soft Tissue Properties of fascia contribute to effects of soft tissue approach Mechanical Circulatory Neurologic Analgesic Jones’ Strain-Counterstrain Jones’ tender point Small, hypersensitive points in the myofascial tissues of the body used as diagnostic criteria and treatment monitors Strain-counterstrain Indirect treatment utilizing a myofascial tenderpoint reflective of musculoskeletal dysfunction elsewhere in the body. Tenderpoint and associated somatic dysfunction is relieved by placing the patient into a position of ease. Mechanism of Strain-Counterstrain Tenderpoint arises when abnormal mm tone is maintained through an inappropriate strain reflex Spindle apparatus and “Relief Reflex”. Passively placing the patient into a position of ease (POE), allows for resetting of the neural components involved in the “strain reflex” “Inherent corrective forces of the body – if the patient is properly positioned, his own natural forces may restore normal motion to an area.” – Rumney, KCOM, 1963 Normal resting tone is achieved, resulting in balance in the muscular system, skeletal system, neural and vascular systems. Golgi tendon apparatus Work of Korr, “Proprioceptors and Somatic Dysfunction,” JAOA 1975 Limitation and resistance to motion of a joint do not ordinarily arise w/in the joint…, but are imposed by one or more of the muscles that traverse and move the joint. The secondary ending reports length at any moment, but the primary ending reports velocity of stretch (hence joint motion) and length (hence joint position). Produces marked inhibitory effect on fibers when the amplitude of the stretch becomes too severe. (Jones) Contracted position becomes “normal resting tone”; limiting range of motion and according to Rennie, maintained through self-propelled metabolic changes. Metabolic – Paul E. Rennie, DO tender point is associated with neural tissue locations – neuromuscular junction or piercing of nerves through the muscle. “metabolic recovery after muscle effort” Vascular and neural components Results in somatic manifestations: Procedure Structural exam Find tenderpoint Establish the pain scale for the patient Passively position the patient into a position of ease, where the relative tenderness elicited by palpation of the same point decreases by 70% Hold the patient in this position for 90 seconds while continuously monitoring the point. Slowly, passively, return the patient to the original starting position. Retest the point. Mechanisms of Facilitated Positional Release Similar to Strain-Counterstrain Stretch reflex Nociceptive model Procedure Diagnose the segment/joint/region Place area to be treated in “postural neutral” Add slight compression then move tissues into their position of ease OR • Place tissues into position of ease and then add slight compression • Hold for 3-5 seconds • Recheck Osteopathic manipulation for the Elderly population Start low, go slow Strain-Counterstrain approach Facilitated Positional Release Myofascial release Soft tissue Structural evaluation - junctions Pelvis and lumbar spine Innominates Sacrum Lumbars Thoracic cage Thorax Ribs Cervical spine and cranium Extremities Heel of hands on anterior aspect of ASIS. Compress down towards the table and a bit lateral to assess motion at the SI joint. Palpate down towards the table, then if tissues allow, out laterally. Place hands at posterior pelvis so that middle fingers are at the level of the PSIS. Lift up on either side to engage rotation. Hand on femur, moving into int and ext rotation. One hand on l-spine assessing motion in response to femur int/ext prom . Hands at T-L junction. Lifting up on each side to assess rotation. Thumbs contacting transverse processes of T1 in back; hands resting over top of cervicothoracic junction, with finger pads assessing rib one. C-spine assessment. OA/AA assessment. SCM-belly trigger point assessment. SCM-clavicular trigger point assessment. Grasp at distal radius/ulna. Pull up out laterally and up into flexion to assess “shoulder” prom . References Literature as listed in presentation Bosco G, Poppele RE. Proprioception From a Spinocerebellar Perspective. Physiologic Reviews. 2001; 81(2):539-68. Hurmuzlu Y, Basdogan C, Stoianovici D. Kinematics and dynamic stability of the locomotion of post-polio patients. J Biomech Eng. 1996 Aug;118(3):405-11. Kiel DP. Falls in older persons: Risk factors and patient evaluation. UpToDate: www.uptodate.com February 3, 2010. Peterka RJ, Black FO. Age-related changes in human posture control: sensory organization tests. J Vestib Res. 19901991;1(1):73-85. Snijders A, van de Warrenburg B, Giladi N, Bloem B. Neurological gait disorders in elderly people: clinical approach and classification. www.neurology.thelancet.com vol 6, January 2007. Ward R, et al. Foundations for Osteopathic Medicine. Williams and Wilkins. 1997. p 608.