Nail Disorders
advertisement

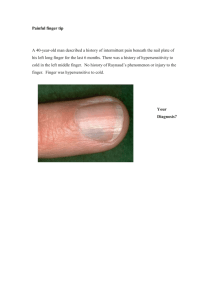
CASE CONFERENCE: Nail Disorders KAREN ESTRELLA 05/12/2010 Do you check the nails of your patients? History 3y/o M seen at SBC for 1st WCC -no acute concerns except for: changes in nail bed of left 2nd nail for 1 year Normal nail • EMBRIOLOGY: – starts to develop at 10-11 wks – keratinizes from 15 wk – fully formed by birth Normal nail • ANATOMY: Consult DERMATOLOGY: • Dark linear, uniform, well demarcated linear ban along the nail bed, involving proximal nail fold Melanonichia striata What is melanonychia? • Tan, brown or black pigmentation from the proximal nail fold and cuticle to the free distal end of the nail plate – Usually affects 1 or 2 digits • Due to: melanocyte activation (physiologic), benign melanocyte hyperplasia (nevi), or melanoma. • Most common in african-american or hispanics Melanonychia etiology: benign • LOCAL – – – – – Trauma Radiation Nail bitting Foreign body Infection Single bands • SYSTEMIC – Addison, Cushing, Hyperthyroidism, – Hemosiderosis – Alcaptonuria – Psoriasis – LES, scleroderma – Malnutrition Multiple bands Melanonychia etiology: iatrogenic • CHEMOTHERAPY – – – – – Metotrexatem Bleomycin Doxorubicin Ciclophosphamide 5-fluoruracil • OTHERS – – – – – Steroids, Ibuprofen Phenytoin Zidovudine, lamivudine Ketokonazole, fluconazole Melanonychia etiology: malignancy • • • • Age: adults Brown-black band greater than 3 mm Change in nail band morphology despite treatment Digit involved: The thumb is more likely to be affected by subungual melanoma than the great toe; the great toe is more likely than the index finger to be affected by subungual melanoma. • Extension onto the adjacent cuticle and proximal and/or lateral nail folds (Hutchinson sign) • Family or personal history of dysplastic nevus or melanoma Melanonychia work-up • Dermatoscopic evaluation: – Of the free edge of nail bed Melanonychia: Dermatoscopic evaluation continued Melanonychia: work-up continued • Nail bed Sampling: – Punch bx: 3mm, from proximal matrix • Risk of permanent nail dystrophy – Nail-shave bx : 4-6mm, central portion of nail bed – lateral-longitudinal – If suspicion for subungueal melanoma: full thickness Melanonychia Treatment • Tx of underlying condition • Removal of agent • If melanoma: complete removal of hyperpigmented section OTHER NAIL DISORDERS Congenital disorders: (Ectodermal defects) • ANONYCHIA – Associated with nail-patella sd., deafness • PACHONYCHIA – Associated with: hyperhidrosis, leukokeratosis: TM, cornea, mucosas Congenital disorders continued • HYPOPLASTIC – Phenytoin – Warfarin – Fetal alcohol syndrome Associated with systemic disorders • CLUBBING – hypoxic stages • KOILONYCHIA (spoon nails) – Iron deficiency Associated with systemic disorders • SPLINTER HEMORRHAGES • HALF & HALF NAILS – endocarditis • RIDGING-TRANSVERSE LINES - malnourishment – liver, kidney failure Acquired nail disorders: infection • PARONYCHIA – Red, tender, swelling of prox or lateral fold • Acute: S. aureus • Chronic: Candida albincans • ONYCHOMYCOSIS - yellowish, brittle - Unusual before puberty - Systemic antifungal tx Acquired nail disorders: dystrophy (distortion, discoloration) • TRAUMA – Subungual hematoma • PSORIASIS Acquired nail disorders: dystrophy continued • TRACHYONYCHIA (Twenty nail dystrophy) – School children – Yellow or gray color nails, (+) pitting, friable – Progresses in 6-18 months, self-limited – Some cases associated with alopecia areata, atopic dermatitis Thank you : ) References • • • • Cohen, B. pediatric Dermatology. Mosby LTD, Spain: 1999. pg 201-208 www.dermaimaging.com/?cat=39 http://www.ncbi.nlm.nih.gov/pubmed/10411404 http://www.scielo.br/scielo.php?script=sci_arttext&pid=S036505962009000200013&lng=en&nrm=iso>. ISSN 0365-0596. doi: 10.1590/S0365-05962009000200013. • http://emedicine.medscape.com/article/1375850-overview • http://www.medscape.com/viewarticle/718695_7