chest tube
advertisement

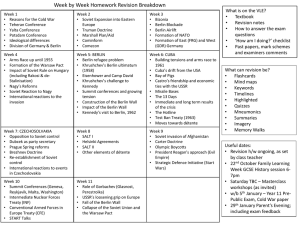
Pneu Concepts in Pneumothorax Tobias Lindner Emergency Dpt.- Trauma Wing UNIVERSITÄTSMEDIZIN BERLIN Diagnostics ….. WHAT DO WE HAVE ? clinicial examination chest film ultrasound CT UNIVERSITÄTSMEDIZIN BERLIN Diagnostics …..clinical examination auscultation alone is not reliable ! 118 patients, penetrating chest injury 71 (60%) with Ptx 30 of these (42%) not diagnosed by inhospital auscultation ! (control: chest radiograph !) Chen et al. : Hemopneumothorax missed by auscultation in penetrating chest injury. J Trauma. 1997 UNIVERSITÄTSMEDIZIN BERLIN Diagnostics ….. chest film…… ….. there is a problem: occult pneumothorax 109 patients after chest trauma only 13 of 25 PTXs detected by supine ap chest film (control: CT) sensitivity 52%, specifity 100 % Soldati et al. : Occult traumatic pneumothorax: diagnostic accuracy of lung ultrasonography in the emergency department. Chest. 2008 UNIVERSITÄTSMEDIZIN BERLIN Diagnostics ….. chest film…… blunt chest trauma, cyclist hit by car UNIVERSITÄTSMEDIZIN BERLIN Diagnostics ….. chest film…… blunt chest trauma, pedestrian hit by metal from lorry UNIVERSITÄTSMEDIZIN BERLIN Diagnostics ….. ultrasound……. M- mode, sliding lung sign B- mode seahore- sign comet- trail- artifacts stratosphere- sign reverberations Ouellet J-F et al., The sonographic diagnosis of pneumothorax. J Emerg Trauma Shock. 2011 Stone MB et al., The heart point sign: description of a new ultrasound finding suggesting pneumothorax. Acad Emerg Med. 2010 UNIVERSITÄTSMEDIZIN BERLIN Diagnostics ….. ultrasound……. M- and B- mode, 3 min. per side, convex probe operators at least 1 year experience (ER personnel) 23 of 25 PTXs detected by ultrasound (remember: only 13 by ap chest film !) 92 % sensitivity, 99.4 % specifity, NPV 98,9 Soldati et al. , Occult traumatic pneumothorax: diagnostic accuracy of lung ultrasonography in the emergency department. Chest. 2008 UNIVERSITÄTSMEDIZIN BERLIN 8 Diagnostics ….. ultrasound…… evidence based review (chest ap radiograph vs US) 4 prospective studies, gold standard: CT 606 patients, blunt trauma cases US: sensitivity 86- 98 %, specifity 97- 100 % chest ap supine: sensitivity 28-75 %, specifity 100 % RG Wilkerson et al., Sensitivity of Bedside Ultrasound and Supine Anteroposterior Chest Radiographs for the Identification of Pneumothorax After Blunt Trauma. Acad Emerg Med.. 2010 UNIVERSITÄTSMEDIZIN BERLIN Diagnostics ….. ultrasound…… Ding et al., CHEST. 2011 20 studies, US: pooled sensitivity/ specifity = 88/ 99 % (CR: pooled sensitivity/ specifity = 52/ 100 %) bedside US performed by clinicians had higher sensitivity and similar specificity compared to CR US depended on the skill of the operators US is reliable & advantage of portability, rapidity and non biological invasive UNIVERSITÄTSMEDIZIN BERLIN Diagnostics ….. however………. does not favor ultrasound in diagnosing spontaneous PTX – results too conflicting (for them !) UNIVERSITÄTSMEDIZIN BERLIN Diagnostics ….. ......instead: standard erect chest x- ray in inspiration (SP) lateral views might be helpful, but no routine expiratory films without additional benefit in doubt : CT UNIVERSITÄTSMEDIZIN BERLIN Therapy…..Guidelines ? Primary & Secondary Spontaneous Pneumothorax (PSP/SSP) UNIVERSITÄTSMEDIZIN BERLIN & UNIVERSITÄTSMEDIZIN BERLIN Therapy……PSP (small, stable) small* vs large small* vs large stable** vs unstable clinical compromise observation in ER for3-6 hrs. breathlessness ? ** check x- ray DISCHARGE (if unchanged) *apex/ cupula distance < 3cm on chest film *hilum to lateral chest wall < **resp. rate < 24/ min., hr > 2 cm on chest film 60/ min. and < 120 /min., bp **not definded normal, O2 sat. room air > 92 % UNIVERSITÄTSMEDIZIN BERLIN Therapy…..PSP (large, stable/unstable) stable & large: small- bore catheter (< 14 F) or chest tube (16-22F) discharge possible with Heimlich valve unstable & large: small- bore catheter or chest tube admit ! UNIVERSITÄTSMEDIZIN BERLIN >2cm &/or breathless: needle aspiration discharge after check x- ray Therapy…….SSP stable, small: observation or tube fatal cases during observation reported !!! (O´Rourke. Chest. 1989) only in < 1 cm without compr.: consider observation or NA all others: chest tube 2cm at level of hilum &/or breathless: small bore catheter admit all ! admit all ! UNIVERSITÄTSMEDIZIN BERLIN size 1-2 cm/ not breathless: needle aspiration Bringing it together…… (needle aspiration) small- bore catheter (< 14F) chest tube (16- 28F) needle aspiration 1st choice, unless: bilateral PTX SSP and > 2cm at level of hilum on CR small bore chest drains (8-14F) (generally, no need for larger bore catheters in all spontaneous PTX) UNIVERSITÄTSMEDIZIN BERLIN NA vs Chest tube in PSP 1 included study, total of 60 patients 27 underwent simple aspiration 33 underwent intercostal tube drainage no significant difference with regard to: immediate, one week or one year success rate simple aspiration is associated with a reduction in hospitalization rate (53 vs 100 %) Wakai et al., Simple aspiration versus intercostal tube drainage for primary spontaneous pneumothorax in adults. Cochrane review. 2007. Based on: Noppen 2002 UNIVERSITÄTSMEDIZIN BERLIN NA vs Chest tube in PSP review NA as safe and successful as tube thoracostomy fewer hospital admissions after NA shorter hospital stays (if admitted) Zehtabchi et al., Management of Emergency Medicine Department Patients With Primary Spontaneous Pneumothorax : Needle Apsiration or Tube Thoracostomy ? Ann of Emerg. Med.. 2008. review NA might fail in larger PTX also SSP studies included ! Chan et al. , The Role of Simple Aspiration in the Management of Primary Spontaneous Pneumothorax, J of Emerg. Med., 2008. UNIVERSITÄTSMEDIZIN BERLIN general remarks: supplementary O2 therapy (at least 24 h) - increases resolution rate by reduction of nitrogen partial pressure no flights until then plus 1 week, but: generally, recurrence risk drops sign. only after 1 year ! no diving unless bilateral pleurodesis ! UNIVERSITÄTSMEDIZIN BERLIN chest drain removal: clamping is generally unnecessary period without suction before removal 41 % of panel members do clamp all check CR before removal 63 % after 13-23hrs after last evidence of air leak UNIVERSITÄTSMEDIZIN BERLIN Traumatic PTX general remarks: 2nd rank of injury after chest trauma (after rib fx) relevant prehospital Dx ! UNIVERSITÄTSMEDIZIN BERLIN Diagnostics …..clinical examination might be (more) reliable in trauma than in spontaneous Ptx ! UNIVERSITÄTSMEDIZIN BERLIN Traumatic PTX- Diagnostics synopsis of auscultation, respiratory rate /shortness of breath. diagnostic accuracy can be improved by combining these three signs…… (and putting hands on ! ) Waydhas et al.,Prehospital pleural decompression and chest tube placement after blunt trauma: A systematic review. Resuscitation. 2007. ……..but still: clinical examination is very variable….. ……. need of: safe, objective method independent from setting German Guideline on Polytraumamanagement- Prehospital Section, 2010 UNIVERSITÄTSMEDIZIN BERLIN Diagnostics ….. ultrasound…… prehospital: possible as on scene method but still skill dependend ! Kirkpatrick et al. , Hand- Held Thoracic Sonography for Detecting Post- Traumatic Pneumothoraces: The Extended Focused Assessment With Sonography for Trauma. J of Trauma. 2004 Walcher et al., Optimierung desTraumamanagements durch präklinische Sonographie. Unfallchirurg. 2002 UNIVERSITÄTSMEDIZIN BERLIN Diagnostics …..what else is on the horizon ? micropower impulsed radar/ultrashort radar pulse spatial accuracy of approx. 5mm UNIVERSITÄTSMEDIZIN BERLIN Diagnostics …..what else is on the horizon ? portable/ point of care non- invasive easy 1-2 min. scan time skin contact unnecessary penetrate through clothing ? specific location and volume ? UNIVERSITÄTSMEDIZIN BERLIN Diagnostics …..what else is on the horizon ? promising ! easy, quick, repeatable, not this operator depended, objective ! INDEPENDENT from preclinical setting ! UNIVERSITÄTSMEDIZIN BERLIN Therapy –Traumatic PTX should all be treated with chest drains ! air & blood ! 28- 36 F ! UNIVERSITÄTSMEDIZIN BERLIN Pneu Concepts in Pneumothorax US is accepted (in experienced operators hands) for diagnosing PTX needle aspiration is the evolving method of choice for active intervention in MOST spontaneous PTx !? there is an urgent need for a easy & objective tool for PTX diagnostics in the prehospital setting ! UNIVERSITÄTSMEDIZIN BERLIN UNIVERSITÄTSMEDIZIN BERLIN Danke ! UNIVERSITÄTSMEDIZIN BERLIN