Slideshow - Great Basin Academy Dental Study Club
advertisement

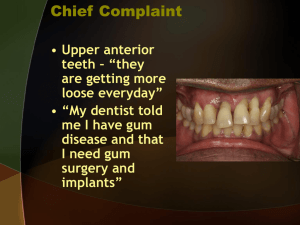
Great Basin Academy Study Club March 2013 Roseman University of Health Sciences Preparation of the Periodontium Iatrogenic Causes and Restorative Considerations Supportive Periodontal Treatment (Maintenance) Results of Periodontal Treatment Presented by Craig M. Ririe, DDS, MS Restorative Dentistry Periodontium free of inflammation Periodontium free of pockets Periodontium free of Mucogingival involvement 3 Implant Dentistry Needs site development Needs bone augmentation Needs gingival augmentation 4 Periodontal Disease must be eliminated prior to Restorative dentistry. To determine gingival margins of restorations properly Inflammation weakens abutment teeth stability Teeth shift in presence of disease 5 Elimination of Periodontal Disease Resolution of inflammation in P.D.L. Regeneration of P.D.L. fibers, APICAL to level of attachment loss Can cause teeth to shift again 6 Fixed bridge work designed for teeth BEFORE the periodontium is treated may produce INJURIOUIS tensions and pressures on the treated periodontium. 7 Abutment teeth must have NO periodontal involvement – Before and after restoration is complete. 8 Removable Partial Dentures Frame work should not be constructed until periodontal treatment is complete and healing is complete. 9 A TRUE ADAGE GARBAGE IN GARBAGE OUT 10 Tooth Mobility 11 SUMMARY The goal of periodontal therapy should be to create the gingival mucosal environment and osseous topography necessary for the proper function of single tooth restorations and fixed and removable partial prosthesis. 12 TREATMENT TO MAKE THIS HAPPEN Treatment Sequence: 1. 2. 3. 4. Hopeless teeth are extracted Construct TEMPORARY partial denture Construct TEMPORARY crowns with PROVISIONAL margins PERIODONTAL THERAPY is performed. 2 months after completion of periodontal therapy Gingival health restored Gingival sulcus mature Periodontal membrane restored to health & function Mobility decreased 13 Treatment Sequence Continued Preparations modified to relocate margins in proper relationship to the healthy gingival sulcus 6. Final restorations (fixed, removable, implants) are constructed 5. 14 Esthetic Needs Clinical crown of tooth must be adequate for retention of artificial crown. 15 To get enough retention you may be tempted to place the margin into the junctional epithelium and connective tissue attachment. 16 Result: Gingival inflammation Sometimes bone loss 17 Biologic Width Violations Ramification of Biologic Width Violation margin placed within the zone of attachment 18 Biologic Width 19 Clinician has 3 options for crown margin placement: Supragingival Equigingival Subgingival 20 Biologic Width Concerns Equigingival margins 21 Biologic Width Average Biologic Width Vacek, et. al.: can be up to 4.3 mm 22 Evaluation of biologic width Radiographs Symptomatic “Sounding” 23 Probe to bone level and subtract sulcus depth (must be done on teeth with healthy gingival tissues) 24 Treatment of Biologic Width Violation Orthodontics Surgery 25 Biologic Width Violation Left central fractured and restored 12 months ago 26 Biologic Width Violation Removal of bone would be unaesthetic 27 Biologic Width Treatment Orthodontic solution erupted 3mm then surgery 28 Biologic Width Violation Orthodontic/Surgical Before 1 year recall 29 Surgical Crown Lengthening Before treatment 30 “Golden Proportion” 31 Surgical Crown Lengthening Ideal gingival symmetry 32 Surgical Crown Lengthening Measurement taken for crown lengthening 33 Surgical Crown Lengthening Incision following Ideal Symmetry 34 Surgical Crown Lengthening Final Restoration • Note the ideal symmetry 35 Biologic Width Average Biologic Width Vacek, et. al.: can be up to 4.3 mm 36 Margin Placement to Avoid Biologic Width Violation HISTOLOGIC SULCUS DEPTH ≠PROBING DEPTH 37 Biologic Width Average Biologic Width Vacek, et. al.: can be up to 4.3 mm 38 Iatrogenic Problems Poor margin placement Margins were covered when restored on Periodontally diseased tissue 39 Electro Surgery Tissue retraction for impression taking 40 Temporary Crowns Critical Areas Marginal Fit Contour Surface Finish 41 Gingival Embrasure Loss of Papilla between #8, 9 42 Gingival Embrasure Method for altering tooth form to fill embrasure 43 Gingival Embrasure One year after restoring #8, 9 mesial 44 Pontic Design Sanitary Pontic Ridge Lap Pontic Modified Ridge Lap Pontic Ovate Pontic 45 Ovate Pontic Design Must be shallow 46 Ovate Pontic in less esthetic area 47 Ridge Consideration Ridge augmentation 48 Iatrogenic Problems Maxillary Partial Denture 49 Iatrogenic Problems Partial Denture Removed • Not removed and cleaned often enough • Not monitored by Dental Office often enough to check for plaque/allergic reaction 50 Iatrogenic Problems Plaque retention on poor restoration margin/gingival interface 51 Iatrogenic Problems Overhanging margin • Bone loss 52 Iatrogenic Problems Inadequate office maintenance during orthodontic care 53 Iatrogenic Problems Maxillary Left bridge #8-11 Periodontally involved 54 Iatrogenic Problems Periodontal Surgery Completed 55 Iatrogenic Problems Calculus 56 Iatrogenic Problems Large Cemented Post • Root Fracture 57 Iatrogenic Problems Retentive Screw Post • Perforated Distal • Bone Loss Repaired 58 Iatrogenic Problems “Idiopathic” bone loss 59 Iatrogenic Problems “Exploratory” Surgery found orthodontic elastic 60 Iatrogenic Problems Removal of orthodontic elastic 61 Iatrogenic Problems Orthodontic elastic 62 Iatrogenic Problems Extracted maxillary molar open margins on crown 63 Iatrogenic Problems Extracted mandibular molar Margin not adapted into furcation 64 Iatrogenic Problems Perforated post into furcation 65 After cementation of crown: cement prevented complete seating of crown. 66 Usually the dentist will not even be aware of this problem. 67 Therefore: Where possible – place margins supra or equigingival. 68 It is best to assume that all of your subgingival margins look like this and then maintain your patients accordingly. 69 Supportive Periodontal Therapy “SPT” Two phases of Treatment: 1. 2. Elimination of Periodontal Disease PRESERVATION of Periodontal health BOTH ARE EQUALLY IMPORTANT 71 The patient must understand the purpose of the maintenance program. The dentist MUST emphasize: preservation of the teeth is dependent on it. 72 FACT!! The more often a patient presents for the recommended SUPPORTIVE PERIODONTAL THERAPY (SPT) the less likely they are to lose teeth. 73 Tooth loss is 3 times as common in treated patients who do not return for regular recall visits as in those who do. Lietha Elmer, 1977 74 Patients with inadequate SPT after successful therapy have a 50 fold increase in probing attachment loss as compared with those with regular SPT appointments. -Cortellini 1994 75 The maintenance phase (SPT) starts immediately after the completion of the Reevaluation appointment. While the patient is in the maintenance phase (SPT) the necessary surgical and restorative procedures are performed. 76 This ensures that all areas of the mouth retain a degree of health attained after phase one therapy (non-surgical therapy) 77 Zone of Influence SUBGINGIVAL PLAQUE Zone of Influence Clinically, we readily see evidence of the inflammation caused by Supragingival plaque. Therefore, we react with plaque control, etc. to resolve what is OBVIOUSLY EVIDENT. But what about the subgingival plaque? The deeper the inflammation – NOT CLINICALLY EVIDENT. 78 But much more damaging – bone loss – attachment loss Subgingival scaling alters the microflora of periodontal pockets. 79 One study shows that after scaling the subgingival flora had not returned to pretreatment proportions after 3 months. But this varies greatly among patients. Slots, J 1979 80 Episodic Nature of Periodontitis Tortuous Topography of a pocket Tortuous Topography of a pocket 82 Importance of fixed, stable, predictable recall system in your office: Patients tend to reduce their oral hygiene efforts between appointments (Out of sight, out of mind) 83 Interval between SPT visits initially set it at 3 months then vary it according to the patients needs 84 SPT Appointment Study page 96 in the Department of Periodontics Clinic Handbook 2010-2011 85 Referral of Patients to the Periodontist Study the Triage September 2005 article by Cobb and Callan 86