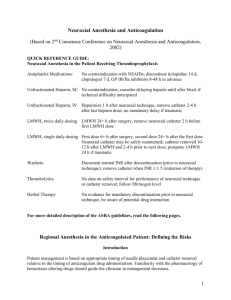
Maternal Fetal Medicine Talk 1
advertisement

What the obstetrician needs to know about anesthesia Tom Archer, MD, MBA Director, Obstetric Anesthesia UCSD July 13, 2011 The black box of anesthesia– Useful, but what is it really all about? ANESTHESIA What ARE those men and women doing BEHIND THE CURTAIN? “Pay no attention to the man behind the curtain” Anesthesia in one sentence: • You can put the nervous system to sleep with all kinds of drugs, and the patient will do fine, as long as she keeps breathing. Two more sentences: • Most “anesthesia” drugs can interfere with breathing. • Anesthesia drugs can cause loss of consciousness, intended or unintended, and this can allow stomach contents to get into the lungs (aspiration). Our drugs interfere with breathing: – Narcotics decrease respiratory rate (to zero!) – Propofol, midazolam cause “upper airway obstruction” (tongue falls back and obstructs). – Severe hypotension causes medullary ischemia and apnea (commonest cause of respiratory arrest after spinal). – High spinal or epidural can paralyze phrenic nerve (less common). – Seizures due to local anesthetic toxicity interfere with breathing. Our drugs allow aspiration: – Loss of consciousness (LOC) is associated with loss of gag, swallow and cough – Any LOC can allow aspiration of regurgitated gastric contents Now you understand what we do all day: • Mess up nervous system • Keep patient breathing • Worry about stomach contents getting into the lungs The rest is details. Two details: • Anesthesia can make the blood pressure go down a lot. That is bad. • Sticking needles into the backs of people whose blood can’t clot is not a good idea. Anesthetic agents and uterus • Inhaled sevoflurane and desflurane relax uterus. This effect goes away fast (don’t blame sevo for atony once patient is awake). N2O does not relax uterus. • IV and neuraxial anesthesia drugs (LA, narcotics, sedatives, hypnotics, propofol, etomidate, low-dose ketamine, etc.) have little to no direct effect on uterus. Epidural test dose • “Epidurals” can cause seizures if local anesthetic goes into a vein. • This is one reason for the “test dose”. • Other reason is to detect intrathecal catheter and prevent “high spinal”. Scenario #1– Elective Cesarean delivery— a uniquely social surgery Let’s teach our residents the proper approach to a unique operation in a unique setting. • We are “on stage” (what we say, do, body language, staff interactions are closely observed and judged). • You know this. Our residents may not. • As anesthesiologists we may not be accustomed to awake patients, presence of family, etc. Help us when we forget. Scenario #1: Elective C-section • Neuraxial anesthesia (NA, spinal or epidural) is good from multiple points of view: • Mother experiences birth, protects her own airway, baby gets minimal drug exposure. • NA allows morphine to be given for post-op pain control. Scenario #1: Elective C-section • NPO, famotidine (Pepcid), metoclopramide (Reglan), sodium citrate (Bicitra). • Despite attempts to empty stomach, we assume full stomach in pregnancy (decreased LES tone, delayed gastric emptying). Routine after spinal/epidural: • Left uterine displacement (how much is enough?). • Vasopressors to increase SVR and venous return (CO). • Decreased emphasis on IV fluid “preloading” than in the past. One equation: • (MAP - CVP) = CO x SVR. • Remember Ohm’s Law? V = IR. • Voltage = Current x Resistance • CVP is small, so MAP = CO x SVR, more or less. Neuraxial anesthesia tends to decrease the MAP, because it • Decreases tone of < 0.1 mm diameter resistance arterioles (SVR), and • Dilates lower body capacitance veins which decreases venous return, and • Venous return = Cardiac output. • And MAP = SVR x CO! Autonomic nervous system. T1 L2 Sympathetics go to internal organs and to veins and arterioles. Blocking sympathetics decreases venous tone (CO) and arteriolar tone (SVR). Blood pressure falls, vagal tone dominates and bradycardia may occur, making situation even worse. Spinal / epidural causes sympathectomy– dilation of resistance arterioles and capacitance veins. www.cvphysiology.com/Blood%20Pressure/BP019.htm 38 y.o. female, repeat c/s, 420 #, gestational hypertension, continuous spinal: fall in systemic vascular resistance (SVR), rise in cardiac output (CO) with onset of block. Increased SVR with phenylephrine. Neuraxial anesthesia is dangerous in OB because: • Inferior vena cava compression by gravid uterus exacerbates decrease in venous return due to sympathectomy. • Hence, supine OB patient and fetus can “crash” after NA. Hence, routine LUD and pressor agents. “High or total spinal” • Respiratory AND circulatory disaster. • Assist ventilation AND support CV system with vasopressors. • Getting baby out promptly will HELP with both breathing and venous return / cardiac output. Colman-Brochu S 2004 When IVC is not compressed, venous return is easy. Cardiac output stays high. http://www.manbit.com/OA/f28-1.htm Manbit images When IVC is compressed, venous return occurs by vertebral plexus and azygos system. CO falls and uterine veins are engorged. http://www.manbit.com/OA/f28-1.htm Chestnut chap. 2 How much LUD is enough? Now we judge by maternal BP and FHR. Is there a better way? Cardiac output (venous return) depends on maternal position late in gestation. 34 y.o. pregnant patient at 26 weeks 3 days estimated gestational age. Hospitalized for preterm labor. No contractions or medications at time of measurement. 120 HR 80 80 SI 30 8 CI 3 Position Minutes S 0 R90 L90 R90 L90 S 33 Archer, Suresh and Ballas 2011 After epidural, BP and CO fall and don’t respond to phenylephrine or ephedrine. BP and CO increase when patient is placed left side down. Archer, Shapiro, Suresh 2011 Autotransfusion observed: once patient is left side down, blood squeezed out of contracting uterus easily gets back to the heart, causing increased CO, as seen here. Archer, Shapiro, Suresh 2011 Basic CS monitoring • • • • • • • Talk with the patient! Does her face display anxiety? “Take a deep breath!” Have her squeeze your fingers What is her hand temperature? Are the hand veins dilated? “Do your hands feel normal or do they feel a little numb?” CS red flags • “I don’t feel so good…I think I’m going to throw up…” (Hypotension until proven otherwise). • “Doc, I feel like I’m not getting enough to breathe…” • The “floppy arm sign.” • The “shaking head sign.” • High spinal will need ventilatory help. One more “equation”: • Neuraxial anesthesia + • Aortocaval compression + • Unreplaced blood loss = • Disaster Intrathecal and epidural medications: • Neuraxial local anesthetics cause sympathectomy and hypotension. Can cause motor block. • Fentanyl (rarely sufentanil): improves quality of block during CS, esp. visceral pain. No sympathectomy, no hypotension, no motor block. Can cause itching. • Morphine for post-CS pain relief. Itching? Block level for CS • Need T4 (nipples) to block visceral pain (traction on peritoneum, exteriorize uterus). Numbness in hands is OK (C5-8). • Lower block will allow skin incision and you can probably “get away with it” but expect visceral discomfort. Leave uterus in for repair to decrease peritoneal traction? • Supplement with fentanyl, ketamine prn. Neuraxial (NA) morphine • Delayed respiratory depression (up to 24 hrs later). With 0.1 mg, very rare (1 per several 1000s). Rx with naloxone (Narcan). • ASA guidelines for post NA morphine monitoring: RR q 1 hr x 12h then q 2h x 12h. • We do a “post CS pain management visit”. Neuraxial morphine • Can cause: itching, nausea, ileus, urinary retention. Itching Rx’d with nalbuphine (nubain) or diphenhydramine (Benadryl). • We do pain orders 1st 24 hours. Caution with IV + NA narcotics. • “Multimodal analgesia”: NA morphine, NSAID, oral acetaminophen plus narcotic (Percocet), cautious IV opioid. NSAIDs for post CS pain • Ketorolac commonly used around the country: 30 mg IV q 6h x 4 doses. Maximum of 5 days. • NSAID contraindications: renal problems (includes pre-eclampsia), GI ulcers, bleeding problems. • American Academy of Pediatrics says: Ketorolac OK for breast feeding. Our NICU says yes. Package insert says no! Spinal Anatomy Vertebral Body Nerves from spinal cord Spinal sack Or Dura Nerve to body Bump on the back Slide courtesy of Alex Pue, MD 40 Spinal Anesthetic is deposited inside the spinal sack and quickly acts on the nerves spinal needle Slide courtesy of Alex Pue, MD 41 Epidural Spinal sack Epidural needle & catheter are outside the spinal sack (dura) Epidural catheter Slide courtesy of Alex Pue, MD 42 Anesthetic initially deposited inside the spinal sack and acts directly on the nerves Combined spinalepidural spinal needle epidural needle Slide courtesy of Alex Pue, MD spinal needle 43 Ultrasound for spinal block placement: first, midline is marked (“shadow” of spinous processes in middle of probe). http://www.usra.ca/sb_neuraxial Then vertical level is marked between spinous processes, where we can see reflection from vertebral body. http://www.usra.ca/sb_neuraxial Ultrasound (US) can be useful in obese patients or patients with scoliosis or other spine pathology. We use the standard OB curved US probe. Needle insertion point is intersection of midline (y-axis) and proper horizontal level (x-axis). http://www.usra.ca/sb_neuraxial Combined Spinal-Epidural spinal needle epidural needle Spinal fluid coming from spinal needle Slide courtesy of Alex Pue, MD 49 Anesthesia for CS— Complications • • • • • • • • • Sympathectomy / hypotension Nausea Bradycardia High spinal / respiratory paralysis Aspiration Difficult intubation Local anesthetic toxicity (IV “epidural”) Failed regional anesthesia GA Persistent neurological deficit “Uterine hypertonic syndrome” • Rapid pain relief with CSE or epidural can cause “fetal distress” due to uterine hypertonus. • We must be aware to avoid unnecessary CS. • Dx is palpate uterus. • Rx is SC terbutaline or SL NTG. • Mechanism: loss of epinephrine beta agonism? Scenario #2: Examination for postpartum hemorrhage (PPH) • Woman postpartum with hemorrhage. • You need to explore birth canal and repair laceration or remove retained placenta. • Epidural catheter in place. • How do we proceed? Scenario #2: In PPH, we are worried about: • • • • • Airway (GA is always Plan B) Adequate IV access Volume status (in shock RRHRBP). Blood availability Keep patient warm and warm all fluids (especially blood) – prevent “fatal triad” of hypothermia, acidosis and coagulopathy. Scenario #2: Examination for postpartum hemorrhage • Anesthesiologist should be reluctant to use epidural catheter in presence of uncorrected hypovolemia. • Even riskier with de novo spinal (faster onset). • Go to OR for exam / repair. Correct volume status and use neuraxial or GA. Scenario #3: STAT CS for “fetal distress” • We are thinking: Airway, airway, airway. • STAT CS is one reason we need advance knowledge of difficult airways. You tell us, or better, we take a peak at everybody. • Minimal History: allergies, meds, heart and lung disease, other major med problems. Scenario #3: STAT CS for “fetal distress” • If airway is sketchy and no neuraxial available, we all have a big problem. Nervous anesthesiologist • If you want to make an anesthesiologist uptight and ornery, ask her to use her wonderful and dangerous drugs when the airway cannot be secured. • Don’t put someone to sleep unless you are sure you can breathe for them. • For us, this is absolutely fundamental. “STAT CS” • • • • • • Often “a flail”. “We’ve got to go. NOW!” Egos and emotions run high. Does the patient know what is happening? Talk to patient. Informed consent. Don’t endanger the mother to “save” the baby. • Anesthesia needs to know when and how to say “no” to the OB. • Stay calm. • Cover the basics (H&P, IV access, airway, informed consent, patient asleep before How do we kill patients in OB anesthesia? • Rush to the OR, pressure to “put the patient down” to save the baby. • IV induction, paralysis. • Panic, confusion, inexperience, bad luck • “Can’t intubate, can’t ventilate” death or brain damage. “The AIRWAY— Anesthesia’s #1 concept” • Just exactly what does it mean? • An anatomical and functional concept which means “We can ensure that the patient will breathe on her own or we can breathe for her.” • “Protected airway” means that stomach contents can’t get into the lungs. Intubating a dolphin would be very easy. They have a “blowhole”. We would be out of a job. Unlike dolphins, humans have a breathing orifice that is hard to get to. Cuffed endotracheal tube (ETT)– gold standard of airway maintenance and protection. http://www.healthsystem.virginia.edu/Internet/AnesthesiologyElective/images/anesth0018.jpg Laryngeal mask airway (“LMA”)– gold standard of airway rescue / maintenance device when ETT not possible. LMA sits behind larynx and epiglottis. Provides limited airway protection. Can be a life-saving device. www.anecare.com/.../QED-spontaneous-brief.html Oral airway plus lift mandible and tongue (“jaw thrust”)– basic airway maintenance maneuver. Provides no airway protection but can be lifesaving. Do this in seizing patient, plus turn her onto her side. What are the threats to the airway? • You and I are the primary threats! • We want to help! • We want to “save the baby”! • Will we choose to induce anesthesia without ensuring the airway? General anesthesia for CS • Recent anesthesia grads will have limited experience with GA for CS because of our success with neuraxial. • And we all get “flustered”. • A good topic for drills, practice. Protocol for general anesthesia for CS Abdomen is prepped, draped, OBs have knife in hand, ready to cut, prior to induction. • Clear, calm, specific communication. • “Patient is awake”, “Patient is asleep”, “You can cut now”. Protocol for general anesthesia for CS Two to three minutes of “preoxygenation” (patient breathes 100% O2 to fill lungs). Pre-oxygenation provides a reserve of O2 for period of apnea after induction and paralysis and before ventilation. Functional residual capacity (FRC) is our “air tank” for apnea. www.picture-newsletter.com/scuba-diving/scuba... from Google images Pregnant Mom has a smaller “air tank”. Non-pregnant woman www.pyramydair.com /blog/images/scubaweb.jpg This is why we “pre-oxygenate” the patient. Wikipedia It gives us more time to get the tube in before she gets low on oxygen. “Ramping up” the obese patient to facilitate intubation. Cephalad retraction of pannus can interfere with breathing. Obese patient: disaster waiting to happen. www.airpal.com/ramp.htm Awake fiberoptic intubation can be lifesaving, but it takes time and skill. We need to know about “difficult airways” in advance, so we evaluate patient and make plans. Weight and Wellness Program (Dr. Lacoursiere) • Integrated approach to obese parturient: • OB, Anesthesia, Nursing, equipment, training, patient buy-in, etc. • Protocols, bundles, etc. • In development… Scenario #4: Severe pre-eclampsia • • • • • Anesthesia worries: Platelets (also PT, PTT, fibrinogen?) Airway swelling / pulmonary edema Stroke / MI / CHF due to hypertension Magnesium effects (uterine atony, potentiates neuromuscular blocking agents, patient on ventilator postop?). Scenario #4: Severe pre-eclampsia • Our approach: neuraxial unless platelets are low (50-100K is the number). Look at venipuncture sites for oozing, under BP cuff for bruising. • Neuraxial will “help” lower BP– but don’t let us overdo it! • Early epidural? Scenario #4: Severe pre-eclampsia • Get epidural in before the platelets go down in HELLP? • Maybe, but then removal of catheter becomes a problem (same requirement for 50-100K). Scenario #4: Severe pre-eclampsia • How recent does platelet count have to be in pre-eclampsia? Communicate with your anesthesiologist. • 2-6 hours in truly severe pre-eclampsia and florid HELLP? I have no firm answer. • 27 gauge spinal? Scenario #4: Severe pre-eclampsia • We should NOT be more worried than usual about catastrophic hypotension with neuraxial anesthesia in pre-eclampsia. • This used to be taught but is less common in pre-eclampsia than in normal patients. Scenario #4: Severe pre-eclampsia • If GA required (low platelets, abruption, severe “fetal distress”, DIC): • Prevent extreme hypertension with laryngoscopy by using IV fentanyl and / or labetalol before induction of GA. • Magnesium will potentiate nondepolarizing NMB agents (curare-like, vecuronium, rocuronium). Scenario #4: Severe pre-eclampsia • Arterial line VERY useful in severe preeclampsia for: • BP, but also mag levels, other blood draws, ABGs in case of pulmonary edema or ventilator care. • A little extra work (and nurses may be unfamiliar) but very helpful. Summary • Neuraxial and general anesthesia are both threats to breathing. • “Airway” is the fundamental concept of anesthesia and our greatest obsession. • Prevention of aspiration of gastric contents is another of our obsessions. Summary • Neuraxial anesthesia is best in OB, but GA is always the backup. • Neuraxial anesthesia + blood loss + IVC compression = disaster. • In OB, we need to get the uterus off the IVC, but knowing how much LUD is enough may be difficult. EC may help with this. Summary • OB anesthesiologist needs to communicate well with rest of OB team. • Obesity requires communication and planning (“systems approach”). • Spinal or epidural best in pre-eclampsia, but check platelets. GA in pre-E requires special care. The End