MMST_2-1
advertisement
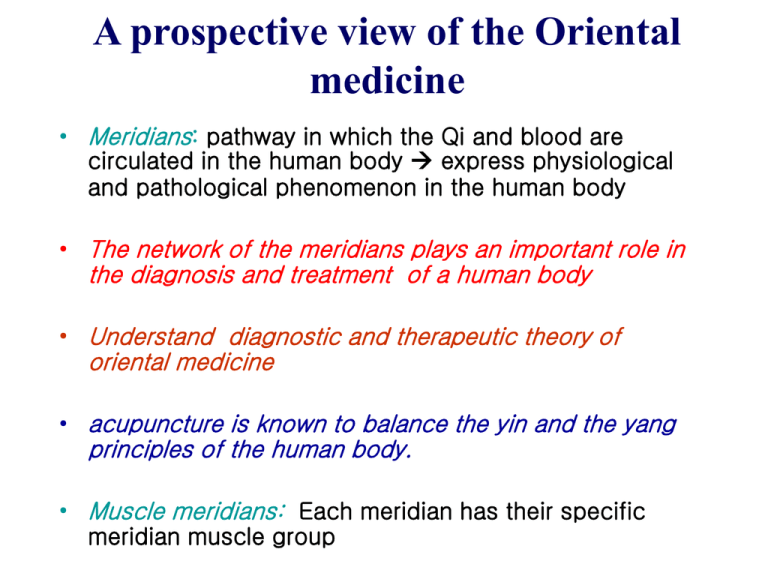
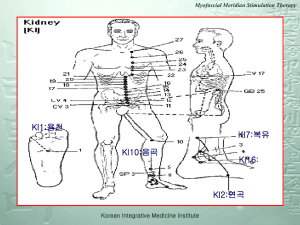
A prospective view of the Oriental medicine • Meridians: pathway in which the Qi and blood are circulated in the human body express physiological and pathological phenomenon in the human body • The network of the meridians plays an important role in the diagnosis and treatment of a human body • Understand diagnostic and therapeutic theory of oriental medicine • acupuncture is known to balance the yin and the yang principles of the human body. • Muscle meridians: Each meridian has their specific meridian muscle group Meridians • • • the meridians in the human body do not exist independently but they are linked with one another like a net in the whole body 14 basic meridians: simplified from a complicated Jing-Lo system having 12 regular meridians plus the CV and the GV Upper limb: 3 yin meridians (LU,PC,HT), 3 yang meridians (LI,TE,SI) Lower limb: 3 yin meridians (SP,LR,KI), 3 yang meridians (ST,GB,UB) • Linked with others like a net in the whole body • Circulation of the Qi and blood Diagnostic and Therapeutic theory of Oriental medicine • 변증시치(辯證施治) • 팔강변증(八綱辨證) • MMST(經筋動穴針法)에 있어서 팔강변증 (八綱辯證)의 해석 변증시치(辯證施治) • 이(理)라는 개념아래서 질병을 분석,종합하여 어떤 성질의 증후인가 를 인식하고 판단,진단하며 치료원칙을 수립하는 것을 ‘변증(辯證)’이 라 한다. • 법(法)이라는 개념 아래에서 치료원칙에 근거한 치료 지침을 결정하 는 것을 ‘시치(施治)’라 한다. • 이때의 ‘증(證)’이란 ‘증(症)’과는 다르다. ‘증(症)’은 질병의 주객관적 symptom을 말하며, ‘증(證)’은 질병의 원인, 부위, 성질과 환자의 신 체 여건 등이 상호 연계된 특징을 지니고 symptom이 종합 구성된 syndrome을 말한다. • Syndrome을 구별 또는 변별하여 치료를 알맞게 운용하는 것을 원칙 으로 한다. • 같은 병(病)이나 증(症)에 같은 치료가 있을 수 없고 같은 증(證)이라 해도 같은 치료를 운용할 수 없는 것이 동양의학적 치료의 특징이다. 팔강변증(八綱辨證) • 팔강(八綱)이란 음양(陰陽), 표리(表裏), 한열(寒熱), 허실(虛實)로 이루어졌다. • 팔강(八綱)은 pathology, symptom, treatment 등 여러 방면에 관련되어 있으 며 기혈(氣穴), 장부(腸腑), 병사(病邪), 육경(六經), 영위기혈(營衛氣血), 삼초 (三焦) 및 경락변증(經絡辨證) 등의 기초가 되므로 disease를 파악할 때 반드시 필요하다. • 음양(陰陽)은 disease의 유형을 구별하는 총강(總綱)으로 삼는다. • 표리(表裏)는 주요 병변이 존재하는 부위를 표시한다. • 한열(寒熱)은 disease의 symptom이 되는 현상을 말한다. • 허실(虛實)은 기(氣)가 쇠약하고 왕성한 것을 말한다. • 표(表), 열(熱), 실(實)은 양(陽)의 범주에 속하고 리(裏), 한(寒), 허(虛)는 음(陰) 의 범주에 속한다. MMST(經筋動穴針法)에 있어서 팔강변증(八綱辯證)의 해석 음양(陰陽) 표리(表裏) 한열(寒熱) 허실(虛實) 음(陰);ying 양(陽);yang Hypomobile Hypermobile 리(裏);inner 표(表);outer Visceral lesion Somatic lesion 한(寒);cold 열(熱);heat Neuropathy Inflammation 허(虛);weak 실(實);strong Chronic Acute Balance of the yin and the yang • acupuncture is known to balance the yin and the yang principles of the human body. • This is compatible with the idea of normalization of the sympathetic and parasympathetic dysfunctions of the human body. • For improvement of autonomic nervous dysfunction, we use sympathetic switch points and parasympathetic switch points introduced by Joseph Y. Wong’s neuro-anatomical approaches. • Sympathetic switches: LI4,LI11,LV3,ST36,UB23,GV3,GV14,GV26 etc. • Parasympathetic switches: CV24,PC6,HT7,SP6,SP9,UB31 to UB34 etc. Sympathetic switch point • Arteries are rich in sympathetic nerve fibers, particularly the smaller arteries. • In the extremities, when the arteries come down to the hands or feet, they form superficial and deep arterial arches. very reactive to sympathetic stimulation(radial artery and deep peroneal artery) • The most commonly used sympathetic switches are: 1) LI4,LI11 in the upper extremity 2) LV3,ST36 in the lower extremity LI4,LI11 in the upper extremity LI4 LI11 LI4 LI11 LV3 in the lower extremity LV3 LV3 ST36 in the lower extremity ST36 ST36 Para-Sympathetic switch point • The parasympathetic nerve fibers are located within the venous and lymphatic system. mainly distributed in the medial aspect of the upper and lower extremities • The three yin meridians run along the medial aspect of the extremities and the acupuncture points in these meridians appear to be able to normalize parasympathetic dysfunction • The most commonly used parasympathetic switch points: 1)HT7, PC6 in the upper extremity 2)SP6, SP9 in the lower extremity SP6 in the lower extremity SP6 SP6 SP9 in the lower extremity SP9 SP9 HT7, PC6 in the upper extremity HT7 PC6 HT7 PC6 Relation of the meridians and the meridian muscles We also use the concept of meridian muscle to explain the methods of assessment about limitation of movment Pectoralis minor LU2 Biceps brachii Brachioradialis LU5 Thenar muscles LU10 LU LU meridian muscle Myofascial Meridian Test(MMT) • If symptoms of musculoskeletal pain and dysesthesia are examined from the above concept ie the expression of tissue strain or failure by limitation of movement on some part of body, this limitation on movement can be examined in association with the myofascial tension line and the meridian line. • Objective diagnosis by selecting a specific myofascial tension line related to limitation on certain movement • Treatment point selection by applying similarity between the myofascial tension line and the meridian muscle line • Myofascial connections과 연관된 postural alignment The analogy between the myofascial line and the meridian muscle The meridians, more specifically the meridian muscle group, is also a network system in the human body which controls physiological function similar to myofascial tension lines Deep front arm line travels very similar to Lu meridian muscle. Deep front arm line LU meridian muscle Limitation of passive movement • focused on the limitation or pain on passive movement for the evaluation of the MMT • LPM(limitation of passive movement)의 stiffness는 근육 이 수축할 때의 관절가동범위 마지막에서의 긴장이 아니라 근육이나 연부 조직을 elongation시키는 과정동안에 나타 나는 저항을 의미한다. The MMT Evaluation I focused on the limitation or pain on passive movement for the evaluation of the MMT Extremities Axis • Cervical : • 1.superficial back line:( + / - ) -neck flexion: UB, SI , GV 2.superficial front line:( +/ - ) -neck extension: LI, ST, CV 3.lateral line: Rt( + / - ), Lt( + / - ) -neck side-bending: GB, TE • Thoracolumbar : 1.superficial back line:( + / - ) -trunk flexion: UB, GV 2.superficial front line:( +/ - ) -trunk extension: CV 3.lateral line: Rt( + / - ), Lt( + / - ) -trunk side-bending: GB 4.spiral line:Rt( + / - ), Lt( + / - ) -trunk rotation: both • Upper extremity 1.deep front arm line: Rt( + / - ), Lt( + / - ) -shoulder extension: LI, LU 2.superficial front arm line: Rt( + / ), Lt( + / - ) -wrist extension: PC 3.deep back arm line: Rt( + / - ), Lt( + / - ) -shoulder elevation: HT, SI 4.superficial back arm line: Rt( + / ), Lt( + / - ) -wrist flexion: TE Lower extremity 1.superficial back line: Rt( + / - ), Lt( + / - ) -leg elevation: UB 2.superficial front line: Rt( + / - ), Lt( + / - ) -leg extension: ST 3.lateral line: Rt( + / - ), Lt( + / - ) -fabere test: GB, LR ,KI, SP Approach of postural alignment • Head and Neck: forward head/chin up neck rotation • Shoulder girdle: humerus head anterior gliding scapular abduction/upward rotation scapular adduction/downward rotation scapular elevation scapular depression • Elbow 1st phalange flexion/ 5th phalange extension Approach of postural alignment • Lumbo-pelvic-hip complex: low back hypertrophy low back flat low back arch iliac crest height in faber test, femur head anterior gliding in SLR, femur head posterior gliding in prone position, knee flex and lateral rotation Approach of postural alignment • Knee: bowleg knock-knee • Foot and Ankle: pronation(eversion) supination(inversion) T.P(Trigger Point or Treatment Point) through MMT • 어떤 움직임의 제한에 관련되는 특정 근막선(myofascial line)을 이용하여 객관적 진단 에 응용할 수 있고, 근막선(myofascial line)과 경락선(meridian line)의 상호 연관성을 이용하여 치료에 응용할 수 있다. • Postural alignment의 변화는 움직임이 제한된 부위를 보상하기 위한 동작이라 이해할 수 있다. 그리고 자세를 관찰하고 움직임을 진단하는 등의 physical examination를 통해 어느 근막선의 움직임이 제한되고 있을까를 판단하는 정보를 얻을 수 있다. • 또한 치료에 접근 시, 수많은 경락 중에서 어느 경락을 선택해야 할 것 인가라고 하는 판 단의 기준이 필요하다. 이러한 이유에 의해서, 어느 근막선의 움직임에 제한이 있는지를 간단하고 쉽게 판단할 수 있는 방법론이 필요하게 되었고 근막선과 경락선과의 상호 연 관성을 이용한 Myofascial Meridian Test를 고안하게 되었다. • MMST(筋經動穴針法)에서는 T.P.는 움직임으로부터 myofascial connection과 meridian pathway의 유사성을 이용한 MMT로 검사하여 선택된 meridian point를 이용 하여 치료를 하는 것이다. Deep front arm line LU meridian muscle LI11 MMT result: Deep front arm line: Rt( + ) -shoulder extension: LI,LU As limitation on passive shoulder extension, We can explain deep front arm line related to LU and LI through analogy between functional anatomy of myofascial line and pathway of meridian muscle. As a result, Trreatment points are LI4,LI11 and LU10 For maintenance of myofascial meridian balance, we have used meridian points selected by the Myofascial Meridian Test (MMT) applying similarity between myofascial lines and meridian muscle lines LU1 0 LI4 Common Patterns of the MMT from clinical observation • Above 80% of all patients; limitation or pain right shoulder passive extension (+), left trunk passive rotation (+), right trunk passive bending (+), trunk passive flexion or extension (+), right fabere test (+), right > left SLR test (+), left > right knee passive flexion (+) Low back approach • Lumbo-pelvic-hip complex • Lumbo-pelvic-hip stabilization • Core stabilization • Lumbar stabilization • Pelvic stabilization • Postural rotation Lumbo-Pelvic-Hip complex • Stabilization system(core system) if not functioning optimally will end neuromuscular substituting to utilize the strength power and neuromuscular control in the rest of the body. • Neuromuscular inhibition -> CNS will shut down prime movers of LPH complex not stabilized -> minimizing the kinetic chain. Functional anatomy of LPH complex • The LPH complex musculature produces force, reduce force, and stabilizes the kinetic chain during functional movements. • The core functions primarily to maintain dynamic postural control by keeping the center of gravity over our base of support during dynamic movements. Lumbo-pelvic-hip stabilization • Two important group: inner unit and outer unit • Inner unit: pelvic floor, transversus abdominis, multifidus, diaphragm • Outer unit: posterior oblique system, deep longitudinal system, anterior oblique system, lateral system • Weakness, or insufficient recruitment and/or timing, of the muscles of the inner and/or outer unit reduces the force closure mechanism through the sacroiliac joint. Lumbo-pelvic-hip stabilization: Inner unit • The levator ani and multifidus act as a force couple to control the position of the sacrum. -> the base of the spine is more stable. • Contraction of transversus abdominis increases the tension laterally in the thoracodosal fascia and helps to increase the intraabdominal pressure. -> role in stabilization of the lumbar spine • transversus abdominis with outer unit -> increase the tension in the posterior SI ligaments through thoracodorsal fascia ->force closure mechanism Lumbo-pelvic-hip stabilization: Outer unit • posterior oblique system: contralateral latissimus dorsi, gluteus maximus, intervening thoracodorsal fascia ->SI joint compression: contralateral latissimus dorsi, gluteus maximus contract • deep longitudinal system: erector spinae, deep lamina of the thoracodorsal fascia, sacrotuberous ligament, biceps femoris ->increase tension in the thoracodorsal fascia and facilitate compression through the SI joint • anterior oblique system:oblique abdominals, contralateral adductor, intervening anterior abdominal fascia • lateral system:gluteus medius and minimus, adductor, contra-lateral quadratus lumborum Lumbo-pelvic-hip stabilizing model:force closure mechanism Lumbo-pelvic-hip stabilizing model: form closure mechanism B.W. Trabecular system of the pelvis follows Weight Bearing Lines Definition of Core • lumbo-pelvic-hip complex with 29 attached muscles • where body’s center of gravity is located and where all movement begin in the kinetic chain • maintains postural alignment and dynamic postural equilibrium during functional activities • provide optimum neuromuscular efficiency by improving dynamic postural control Composition of Core • Inner unit transverse abdominis multifidus pelvic and respiratory diaphragm Role of Core stabilization • Improve dynamic postural control • Ensure appropriate muscular balance and joint arthrokinematics • Allow functional strength • Provide intrinsic stability to the lumbo-pelvic-hip complex, which allows for optimum neuromuscular efficiency of the rest of the kinetic chain Lumbar stabilization Compression force Iliopsoas pull Posterior shearing force DES pull Anterior shearing force Compression force Pelvic stabilization: locking mechanism Iliolumbar ligament Many low back injuries occur in this position *Long dorsal sacroiliac ligament tightens *SI joint is less compressed and more motor control is required for load transference. Nutation * More stable than counte-rnutation *Sacratuberous ligament and interosseous ligament tighten *Increasement of ligamentous tension: force closure and compression Efficient load transfer: through pelvic girdle to lower extremity Counter-nutation Sacrotuberous ligament Pelvic tilting mechanism Lumbo-pelvic-hip muscle imbalance Exaggerated anterior pelvic tilt with lumbar extension during active knee flexion • Compensatory reaction -> lumbar extension • Posterior pelvic tilt due to contraction of hamstring -> contraction of hip flexor and paraspinal muscle • 운동을 막기위한 것보다는 요추의 과도한 flexibility때문에 stabilizing muscle에서 수축이 유발된다 Left postural rotation 1.limitation of right rotation -> left side bending에 제한 (coupling movement) TL junction의 stress 증가 >segmental hyperactivity 2.Left DES의 hypertrophy -> abnormal posterior shearing force & compression 3.Left side bending의 limitation >Quadratus lumbarum elongation External & contrallateral Internal oblique m이 작용 ->rotation Right rotation의 제한될 때 DES elongation이 restrict Spinal stenosis • Spinal canal or intervetebral foramen: narrowing -> symptom • Complex dysfunction: degenerative disc, arthritis, subluxation -> lamina of vertebral arch와 척추 후면의 비대 -> facet joint 비대로 nerve root의 침식 • Lumbar extension -> symptoms occur LR8:곡천 LR3:태충 LR7:슬관 GB14:양백 GB26:대맥 GB28:유도 GB30:환도 GB29:거료 GB31:풍시 GB20:풍지 GB34:양릉천 GB43:협계 GB21:견정