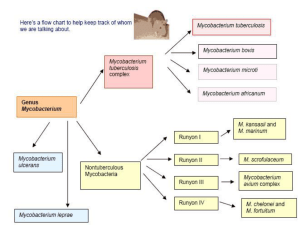
CLASSIFICATION - thegreentraveler.net

Module 1:
LEPROSY: The Disease
WHAT IS LEPROSY?
Leprosy is a chronic infectious disease caused by Mycobacterium leprae, an acid-fast, rod-shaped bacillus that mainly affects the skin , peripheral nerves , mucosa of the upper respiratory tract and eyes .
It has a very long incubation period or latency which ranges from 3 to 15 years.
• Leprosy is an infectious disease directly transmitted from man to man.
• It is acquired through prolonged repeated exposure & chromo 6
• It is transmitted from one untreated person to another via the respiratory tract .
• Only a small proportion of the population is affected (5%);(95%) develop immunity.
DIAGNOSIS OF LEPROSY:
Diagnosis of leprosy is mainly based on clinical signs and symptoms.
Only in rare instances is there a need to use laboratory and other investigations to confirm a diagnosis of leprosy.
An individual should be regarded as having leprosy if he exhibits the following cardinal signs:
Hypo-pigmented or reddish skin lesion(s) with definite sensory loss;
Peripheral nerve damage, as demonstrated by loss of sensation and muscle weakness in the hands, feet and/ or face;
Positive skin smear.
Other signs of leprosy are:
Skin lesion(s) with a decrease or loss of sweating and/or hair growth;
Other signs of leprosy are:
Skin lesion(s) with a decrease or loss of sweating and/or hair growth;
Constant redness in the eyes from irritation and dryness;
Other signs of leprosy are:
Skin lesion(s) with a decrease or loss of sweating and/or hair growth;
Constant redness in the eyes from irritation and dryness;
Loss of eyebrows and eyelashes (madarosis);
Other signs of leprosy are:
Skin lesion(s) with a decrease or loss of sweating and/or hair growth;
Constant redness in the eyes from irritation and dryness;
Loss of eyebrows and eyelashes (madarosis);
Other signs of leprosy are:
Nasal congestion / obstruction and frequent nosebleed
Collapse of nose bridge;
Other signs of leprosy are:
Enlargement of the breast in males
(gynecomastia);
Other signs of leprosy are:
Mobile or stiff clawing of fingers and toes
Other signs of leprosy are:
Chronic ulcers, usually in the sole of the foot, palm of the hands and fingers.
Diagnosis of leprosy is mainly based on clinical signs and symptoms . i
The development of complications can be effectively prevented through early detection , correct i diagnosis and effective treatment .
PATIENT’S HISTORY
:
The leprosy case history should have the following information:
1.
The nature of the first lesion or symptom and its progress.
This is because the skin lesion usually develops slowly over several months and is not troublesome.
Ask:
• When did the patient
?
first notice the lesion?
• What was its appearance?
• How did it feel? Was it painful?
Itchy?
PATIENT’S HISTORY
:
2.
Past Treatment.
Ask:
• What did the patient do when he first noticed the lesion?
• Did he apply any drug(s)?
• What was the effect of this/these
?
drug(s)?
PATIENT’S HISTORY
:
3.
Other Illnesses.
Pay attention to contra-indications to
MDT drugs; or any other illness requiring special attention and/or referral.
Ask:
• Does the patient have a history of liver disease?
• Allergy to drugs?
• If yes, what drugs?
?
PATIENT’S HISTORY
:
4.
Contact with Persons With Leprosy
(PWLs)
This information will help determine the patient’s susceptibility to the disease.
Ask: family have leprosy?
• Does he have a friend or acquaintance who has/had leprosy?
CLASSIFICATION :
Leprosy can be classified on the basis of clinical manifestations and skin smear results.
The Ridley-Jopling classification has seven (7) types of leprosy:
CLASSIFICATION : (Ridley-Jopling)
1. Indeterminate (I).
Solitary, ill-defined, faintly hypopigmented macule, with partial loss of sensation.
CLASSIFICATION : (Ridley-Jopling)
1. Indeterminate (I)
Solitary, ill-defined hypopigmented macule on left cheek; only partially anesthetic.
CLASSIFICATION : (Ridley-Jopling)
1. Indeterminate (I)
Solitary, ill-defined, faintly hypopigmented macule on the dorsum of the wrist; minimal surface changes; partially insensitive.
CLASSIFICATION : (Ridley-Jopling)
1. Indeterminate (I)
Single, slightly hypochromic macule with ill-define borders on the dorsum of the lower right forearm; minimal surface changes; partially anesthetic.
CLASSIFICATION : (Ridley-Jopling)
2. Tuberculoid (TT)
Small, solitary marginally hypopigmented oval lesion, with papulated well-defined margins with flat, slightly atrophic central area insensitive to pain.
CLASSIFICATION : (Ridley-Jopling)
2. Tuberculoid (TT)
Faintly hypochromic, rounded macule with discontinuously papulate borders, fairly defined, anesthetic, above smallpox vaccination scar on the left arm.
CLASSIFICATION : (Ridley-Jopling)
2. Tuberculoid (TT)
Solitary, well-defined early tuberculoid lesion with slightly papulate borders; completely anesthetic.
CLASSIFICATION : (Ridley-Jopling)
2. Tuberculoid (TT)
Sharp-edged, hypopigmented, ringworm-like lesion with finely papulate borders; anesthetic.
CLASSIFICATION : (Ridley-Jopling)
2. Tuberculoid (TT)
Superficial, circinate lesion with pinkish, elevated, finely granular margins; center is insensitive to touch and pain.
CLASSIFICATION : (Ridley-Jopling)
2. Tuberculoid (TT)
Well-defined, hypopigmented lesion with dry surface and moderately raised granular margins; completely anesthetic.
CLASSIFICATION : (Ridley-Jopling)
3. Borderline
Tuberculoid (BT)
Rounded lesion with wide, slightly brownish and scaly elevated margins fairly welldefined, center flat, with noticeable hair loss; at posterior aspect of the leg; anesthetic.
CLASSIFICATION : (Ridley-Jopling)
3. Borderline
Tuberculoid (BT)
One of several sharpedged, erythematous patches on the patient, with fairly thick granular margins and small satellite lesions; anesthetic.
CLASSIFICATION : (Ridley-Jopling)
3. Borderline
Tuberculoid (BT)
Well-defined, dry and rough surfaced plaque on cheek, insensitive to touch and pain; note papulo-nodular lesions near eye and upper lip
CLASSIFICATION : (Ridley-Jopling)
3. Borderline
Tuberculoid (BT)
Distinct, erythematohypochromic patch with a dry surface and raised, well defined margins showing satellite lesions; anesthetic.
CLASSIFICATION : (Ridley-Jopling)
3. Borderline
Tuberculoid
(BT)
Large patch with wide, raised erythematous well-defined margins sloping toward center of lesion; central portion is anesthetic.
CLASSIFICATION : (Ridley-Jopling)
3. Borderline
Tuberculoid (BT)
Multiple, sharplydemarcated, scaly reddish-brown plaques; these subsiding lesions are only partially anesthetic.
CLASSIFICATION : (Ridley-Jopling)
3. Borderline
Tuberculoid (BT)
Large, thickly infiltrated, sharp-edged plaque with slightly scaling surface; anesthetic.
CLASSIFICATION : (Ridley-Jopling)
3. Borderline
Tuberculoid (BT)
Extensive, subsiding lesions showing large, clear center areas surrounded by welldefined, slightly raised, inner and outer margins; centers are anesthetic.
CLASSIFICATION : (Ridley-Jopling)
4. Borderline (BB)
Fairly extensive succulent plaque with sharply demarcated clear central area; peripheral edges sloping into surrounding normal skin; central uninvolved area anesthetic.
CLASSIFICATION : (Ridley-Jopling)
4. Borderline (BB)
Several “punched-out” lesions very characteristic of borderline leprosy; central areas are anesthetic.
CLASSIFICATION : (Ridley-Jopling)
4. Borderline (BB)
Irregular, erythematous, infiltrated bands around a large, anesthetic central “immune” area; inner margins of lesion tend to be better defined than the outer margins.
CLASSIFICATION : (Ridley-Jopling)
4. Borderline (BB)
Classical “punched-out” lesions of borderline leprosy; central
“immune” areas are anesthetic.
CLASSIFICATION : (Ridley-Jopling)
5. Borderline
Lepromatous (BL)
Numerous and widespread borderlinetype plaques, annular lesions, papules and macules; center of large lesions show some loss of sensation.
CLASSIFICATION : (Ridley-Jopling)
5. Borderline
Lepromatous (BL)
Thick, erythematous plaques on face and ears. Lesions are not sharply defined and show no sensory impairment.
CLASSIFICATION : (Ridley-Jopling)
5. Borderline
Lepromatous
(BL)
Bilaterally distributed, irregularly shaped, erythematous, infiltrated patches; these are not anesthetic.
CLASSIFICATION : (Ridley-Jopling)
5. Borderline
Lepromatous
(BL)
Fairly uniform symmetrically distributed, infiltrated, maculo-papular lesions, none of which show sensory impairment.
CLASSIFICATION : (Ridley-Jopling)
6. Sub-polar
Lepromatous (LLs)
Symmetrically distributed infiltration with prominent macular lesions. Note borderline-type, punched-out patches on the wrist.
CLASSIFICATION : (Ridley-Jopling)
6. Sub-polar
Lepromatous (LLs)
Symmetrical infiltration and erythematous macules, with an unusual borderline-type plaque on the left buttock.
CLASSIFICATION : (Ridley-Jopling)
6. Sub-polar
Lepromatous
(LLs)
Extensive, symmetrically distributed infiltration with almost coalescent macules and plaques. These lesions are not anesthetic. Note small rounded borderline-type plaque on the left lumbar area.
CLASSIFICATION : (Ridley-Jopling)
7. Polar Lepromatous
(LLp)
Early lepromatous leprosy with recognizable diffuse infiltration all over face and ears.
CLASSIFICATION : (Ridley-Jopling)
7. Polar Lepromatous
(LLp)
Fairly advanced lepromatous leprosy, with symmetrically distributed diffuse infiltration, nodules on face and ears, and madarosis.
CLASSIFICATION : (Ridley-Jopling)
7. Polar Lepromatous
(LLp)
Advanced lepromatous leprosy, with marked diffuse infiltration, madarosis and loss of eyelashes.
CLASSIFICATION : (Ridley-Jopling)
7. Polar Lepromatous
(LLp)
Advanced lepromatous leprosy with diffuse infiltration coupled with nodules over eyebrows, cheeks, ala nasae and chin, as well as earlobes.
CLASSIFICATION : (Ridley-Jopling)
7. Polar Lepromatous
(LLp)
Advanced lepromatous leprosy with diffuse infiltration and nodular lesions.
The World Health Organization (WHO) classifies leprosy into only three (3) types:
• Single Lesion Paucibacillary (SLPB)
• Paucibacillary (PB)
• Multibacillary (MB)
CLASSIFICATION :
Characteristic
Lesions:
• Type
SLPB
Macule
PB
Infiltrated patches
MB
Macules, plaques, papules & infiltration
CLASSIFICATION :
Characteristic
Lesions:
• Number
SLPB
One (1)
PB
Two (2) to five (5)
MB
More than five (>5)
CLASSIFICATION :
Characteristic
Lesions:
• Surface
SLPB PB
Normal, dry or scaly
Normal, dry or scaly, absence of hair growth
MB
Smooth & shiny, some lesions may be dry
CLASSIFICATION :
Characteristic
Lesions:
• Border
SLPB PB MB ill-defined to well-defined
Well-defined, clear-cut margins
Vague, sloping outwards, merges imperceptibly with surrounding skin
CLASSIFICATION :
Characteristic
Nerve
Involvement:
SLPB
None
PB
Zero (0) to one (1)
MB
More than one (1)
CLASSIFICATION :
Characteristic
Slit Skin
Smear:
SLPB
Negative
PB
Negative
MB
Positive
NOTE: Positive skin smear = Multibacillary (MB) regimen .