Technical Considerations of Perfusion CT
advertisement

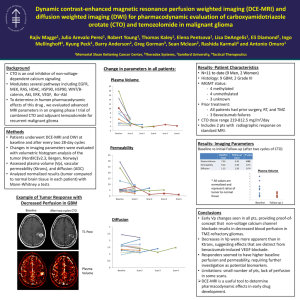
ACRIN Gynecologic Committee Fall Meeting 2010 ACRIN Abdominal Committee ACRIN Gynecologic Committee CT Perfusion Study of Ovarian Cancer ACRIN 6695 Project Team ACRIN Abdominal Committee ACRIN Gynecologic Committee Study Schedule Regimen I: Cycle 2 Cycle 3 Cycle 4 Cycle 5 Cycle 6 Cycle 1 (All cycles 3 weeks in length) Ovarian cancer: suboptimally debulked (e.g. > 1 cm tumor left behind Surgically) R A N D O M I Z E Carboplatin AUC 6 IV day 1 every cycle x 6 cycles Paclitaxel 175 mg/m2 IV Day 1 every cycle x 6 cycles Bevacizumab 15 mg/kg IV day 1 every cycle starting cycle 2 and continuing beyond cycle 6 until progression or adverse effects preclude further treatment Regimen II: Cycle 1 (All cycles 3 weeks in length) Cycle 2 Cycle 3 Cycle 4 Cycle 5 Cycle 6 Carboplatin AUC 6 IV day 1 every cycle x 6 cycles Paclitaxel 80 mg/m2 IV days 1, 8 and 15 every cycle x 6 cycles Bevacizumab 15 mg/kg IV day 1 every cycle starting cycle 2 and continuing beyond cycle 6 until progression or adverse effects preclude further treatment Perfusion CT intermediate (T1) Baseline RECIST CT scan & Perfusion CT Baseline (T0) at end of 1st cycle between 18-21 days At least 3 weeks post surgery and within 4 weeks prior to initiating protocol chemotherapy Perfusion CT (T2) Reproducibility Perfusion CT After one week into cycle 2 A subgroup of patients will be studied ACRIN Gynecologic Committee Follow-up RECIST CT scans after cycle 3,6,14,22 After completion of all protocol therapy, every 3 months for 2 years, then every 6 months for 3 years, then annually CT Perfusion Study Protocol Scout to define limits of localization scan Localization scan Use site abdominal scan protocol Define limits of tumor, either 4 or 8 cm slab If follow-up study, try locate the same tumor slices as the initial baseline study CT Perfusion scan as per protocol GE Healthcare scanner - non axial shuttle mode GE Healthcare scanner – axial shuttle mode Toshiba Aquilion One scanner No breath-hold, patient is instructed to breath normally during scan Contrast dose 0.7 ml per kg body weight up to a max of 65 ml Injection rate 3-4 ml per second Radiation dose 4 cm coverage : 9.5 mSv 8 cm coverage : 16.8 mSV ACRIN Gynecologic Committee CT Perfusion Scan Protocol 64-slice CT scanner with 40 mm wide detector array without toggling table mode 40 axial scans @ 2.8 - 3 s intervals: 120 kVp; 100 mA; 8 x 5 mm slices; 0.4 s rotation period 0s 3 6 9 12 1 2 3 4 Inject 300 – 370 mgI/ml contrast 0.8 ml/kg @ 3 – 4 ml/s ACRIN Gynecologic Committee 114 117 120s 38 39 40 Effective Dose = 7.2 mSv Skin dose = 150 mGy CT Perfusion Scan Protocol 64-slice CT scanner with 40 mm wide detector array with toggling table mode 40 passes @ 2.8 - 3 s intervals: 120 kVp; 100 mA; 16 x 5 mm slices; 0.4 s rotation period 0s 3 6 9 12 1 2 3 4 Inject 300 – 370 mgI/ml contrast 0.8 ml/kg @ 3 – 4 ml/s ACRIN Gynecologic Committee 114 117 120s 38 39 40 Effective Dose = 14.3 mSv Skin dose = 150 mGy CT Perfusion Scan Protocol 128-slice CT scanner with 80 mm wide detector array 40 axial scans @ 2.8 - 3 s intervals: 120 kVp; 100 mA; 16 x 5 mm slices; 0.4 s rotation period 0s 3 6 9 12 1 2 3 4 Inject 300 – 370 mgI/ml contrast 0.8 ml/kg @ 3 – 4 ml/s ACRIN Gynecologic Committee 114 117 120s 38 39 40 Effective Dose = 14.3 mSv Skin dose = 150 mGy CT Perfusion Scan Protocol 256-slice CT scanner with 120 mm wide detector array 40 axial scans @ 2.8 - 3 s intervals: 120 kVp; 100 mA; 20 x 5 mm slices; 0.4 s rotation period 0s 3 6 9 12 1 2 3 4 Inject 300 – 370 mgI/ml contrast 0.8 ml/kg @ 3 – 4 ml/s ACRIN Gynecologic Committee 114 117 120s 38 39 40 Effective Dose = 17.8 mSv Skin dose = 150 mGy CT Perfusion Scan Protocol 320-slice CT scanner with 160 mm wide detector array 40 axial scans @ 2.8 - 3 s intervals: 120 kVp; 100 mA; 24 x 5 mm slices; 0.4 s rotation period 0s 3 6 9 12 1 2 3 4 Inject 300 – 370 mgI/ml contrast 0.8 ml/kg @ 3 – 4 ml/s ACRIN Gynecologic Committee 114 117 120s 38 39 40 Effective Dose = 21.4 mSv Skin dose = 150 mGy Example CT Perfusion Scan of Prostate Average Effective dose 21 mSv Enhancement (HU) 200 150 Artery 100 50 0 0 20 40 60 80 100 120 140 Time (s) Scan Protocol Each scan: 16 x 5 mm slices @ 80 kVp and 50 mAs 1 scan every 2.8 s 42 scans 40 35 30 Enhancement (HU) Intravenous Injection of Contrast Agent 60-70 ml @ 3-4 ml/s 25 20 15 10 5 0 0 ACRIN Gynecologic Committee 20 40 60 80 -5 Time (s) 100 120 140 Deconvolution with physiol model 250 AVG Blood Flow BF Blood Volume BV PS PS Primary Objective To determine whether larger changes in the tumor perfusion parameters (BF, BV, MTT, PS) from baseline T0 to T2 are predictive of higher progression-free survival (PFS) rate at 6 months in patients treated with weekly paclitaxel regimen or every-3-week paclitaxel regimen, who are receiving carboplatin with or without bevacizumab ACRIN Gynecologic Committee Secondary Objectives To determine whether larger changes in tumor perfusion parameters from baseline T0 to T1 are predictive of higher progression-free survival (PFS) rate at 6 months in patients treated with weekly paclitaxel regimen or every3-week paclitaxel regimen, who are receiving carboplatin with or without bevacizumab To determine whether larger changes in tumor perfusion parameters values from T0 to T1, T0 to T2 and T1 to T2 are predictive of better overall survival in all treatment arms. To assess the association between changes in tumor perfusion parameters before and after chemotherapy and subsequent best tumor response according to standard anatomic response evaluation criteria (RECIST). To assess the association between tumor perfusion parameters before chemotherapy and subsequent best tumor response according to standard anatomic response evaluation criteria (RECIST), progression free survival at 6 months and overall survival. To test the assumption that tumor perfusion parameters are reliable, userindependent and reproducible parameters of tumor microvascular characteristics. A subgroup of 15 patients will have repeat CT Perfusion studies at T1 to achieve this objective ACRIN Gynecologic Committee Radiation Risk Radiation Dose Effective dose • • Research plus normal care – 87.2 mSv Annual background – 3.0 mSv Cancer induction and fatality risk BEIR VII report • Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation, National Research Council Excess cases of cancer (all solid cancers and leukemia including non-fatal cases) from ONE DCE-CT study per 100,000 exposed 1,195 Number of cancer cases per 100,000 in the general population not exposed to radiation 37,490 Excess cases of cancer death from ONE CT Perfusion study per 100,000 exposed 576 Number of cancer deaths per 100,000 in the general population not exposed to radiation 18,030 ACRIN Gynecologic Committee Questions ? ACRIN Abdominal Committee ACRIN Gynecologic Committee