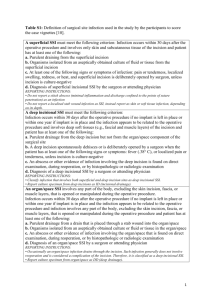
Surgical Site Infection Improvement Programme case studies (291
advertisement

Surgical Site Infection Improvement Programme Surveillance: Case studies Case 1 • A patient had bilateral knee prostheses (KPRO) implanted during a single trip to the OR – Left KPRO incision at 0823 and closed at 0950 – Right KPRO incision at 1003 and closed at 1133 Which statement is true A. One KPRO procedure should be reported with a combined duration of 2 hours 57 min B. Two separate KPRO procedures should be reported, each with a duration of 2 hours and 57 min C. Two separate KPRO procedures should be reported: – L KPRO with a duration of 1 hour 27 min – R KPRO with a duration of 1 hour 30 min Correct Answer C. Two separate KPRO procedures should be reported: —L KPRO with a duration of 1 hour 27 min —R KPRO with a duration of 1 hour 30 min Rationale • For operative procedures that can be performed bilaterally during same trip to operating room (e.g., KPRO), two separate Denominator for Procedure forms are completed • To document the duration of the procedures, indicate the incision time to closure time for each procedure separately • If separate times are not known, take the total time for both procedures and split it evenly between the two Case 2 • 18th July – 45 year old man had a Total Hip Replacement (HPRO) • 22nd July – Patients hip incision has purulent drainage from subcutaneous tissue and slight erythema; incision is intact. – Wound drainage specimen sent to lab for culture (24th July: grew S aureus) – Patient started on antibiotics What should be reported to NZ surveillance • Nothing – the surgeon did not open the wound, so the criteria are not met • Nothing, It is an HAI but not an SSI • Superficial SSI • Deep SSI Correct Answer • Superficial SSI Rationale • Infection occurs within 30 days after the operative procedure, and • Involves only skin and subcutaneous tissue of the incision, and • Patient has at least one of the following: a. b. c. purulent drainage from the superficial incision organisms isolated from an aseptically obtained culture of fluid or tissue from the superficial incision. superficial incision that is deliberately opened by surgeon and is culturepositive or not cultured, and d. patient has at least one of the following signs or symptoms: pain or tenderness, localised swelling, redness, or heat. A culture-negative finding does not meet this criterion. diagnosis of superficial incisional SSI by the surgeon or attending physician. Case 2 (ii) • 18th July – 45 year old man had a Total Hip Replacement (HPRO) • 22nd July – Patients hip incision has purulent drainage from subcutaneous tissue and slight erythema; incision is intact. – Wound drainage specimen sent to lab for culture (24th July: grew S aureus) – Patient started on antibiotics What is the date of infection? Answer • 22nd July (when criteria first met i.e. purulent drainage) Case 3 • Patient is admitted to the hospital on 4th July for elective surgery and active MRSA screening test is positive • On the same day patient undergoes Total knee replacement (KPRO) • Post operative course is unremarkable; patient discharge on the 8th July • On the 21st July patient is readmitted with complaints of acute incisional pain since the day before. Surgeon opened the wound to the fascial level and sent drainage specimen for culture and sensitivities • On 25th July, culture results are positive for MRSA What infection should be reported? • Superficial Incisional SSI • Deep Incisional SSI • Organ/space SSI Answer • Deep Incisional SSI – Criterion b Rationale Infection occurs within 30 or 90 days after the operative procedure and Involves deep soft tissues of the incision (e.g., fascial and muscle layers), and Patient has at least one of the following: a. purulent drainage from the deep incision b. a deep incision that spontaneously dehisces or is deliberately opened by a surgeon and is culture-positive or not cultured, and patient has at least one of the following signs or symptoms: fever (>38ºC), localised pain or tenderness. A culture-negative finding does not meet this criterion. c. an abscess or other evidence of infection involving the deep incision that is found on direct examination, during invasive procedure, or by histopathologic examination or imaging test. d.diagnosis of a deep incisional SSI by a surgeon or attending physician. Case 4 • Patient has a THR (HPRO) performed on the 17th March at Hospital A • Discharged from Hospital A on 19th March • Admitted to Hospital B on 25th March with purulent drainage from the superficial incision • Further investigation concludes this is a superficial incisional SSI •What should hospital B do? •What should hospital A do? •What if the infection became apparent 35 days after the procedure? Answers • What should hospital B do? – Notify Hospital A about the SSI • What should hospital A do? – Report the SSI to NZ surveillance • What if the infection became apparent 35 days after the procedure? – Not an SSI; not reported Rationale •SSIs are always associated with a particular operative procedure and with the facility in which the operation was performed; in this case, this was Hospital A •Superficial SSI are followed for only 30 days Case 5 • Patient admitted on the 9th October and underwent a R THR; wound class – clean • 13th Oct the patient has a temp 38.7oC and hip pain. Ultrasonography shows abscess in the hip joint • 14th Oct the joint abscess is aspirated and the specimen is sent for culture. Antibiotics started. • 18th Oct patient is discharged from hospital on oral antibiotics. Abscess is culture positive for Staph aureus What type of infection does this patient have? A. B. C. D. Superficial Incisional SSI Deep Incisional SSI Organ/space SSI Does not meet criteria for any SSI Answer Organ/space SSI – joint Organ/ Space SSI Infection occurs within 30 or 90 days after the VICNISS operative procedure and Infection involves any part of the body, excluding the skin incision, fascia, or muscle layers, that is opened or manipulated during the operative procedure, and Patient has at least one of the following: a. purulent drainage from a drain that is placed into the organ/space. b. organisms isolated from an aseptically obtained culture of fluid or tissue in the organ/space. c. an abscess or other evidence of infection involving the organ/space that is found on direct examination, during invasive procedure, or by histopathologic examination or imaging test. d. diagnosis of an organ/space SSI by a surgeon or attending physician. and Meets at least one criterion for a specific organ/space infection site Case 6 Day 1 HPRO performed. Patient screened for MRSA upon admission as per local protocol Day 2 Patient is very confused. Temperature normal. Wound condition good Day 3 Results of the admission screening cultures of the nose and groin are positive for MRSA. The following entry is found in the chart: “patient removed dressing several times. Recurrent confused condition. Wound edges very red and taut” Case cont… Day 5 Entry in the chart: “wound abscess lanced by the attending surgeon”. A wound specimen sent to lab for culture. Antibiotics begun. Day 7 Wound culture: MRSA Day 9 Improvement in wound condition. Discharged to rehab centre Does this patient have an SSI? If Yes, what type? Answers • Does this patient have an SSI? – Yes • If Yes, what type? – Superficial incisional SSI Rationale • Post-op patient has an intact incision or status of incision is unknown (e.g., dressing never changed so no one has seen the incision), or it is noted that patient showered/bathed “too early” post-op, or it is noted that the patient was incontinent and incision was or may have been contaminated, or patient got intact incision dirty, then subsequent incisional infection is considered an SSI. Case 7 • A patient underwent a KPRO in April 2011 • In October 2012 the prosthesis was removed due to an unresolved infection in the joint space with MRSA. A spacer was placed and a replacement procedure was scheduled for the following Feb 2013. • The replacement KPRO was completed in Feb 2013 and, within 3 weeks after discharge, he developed osteomyelitis with MRSA near the attachment site How should this osteomyelitis be reported? A. SSI linked to the April 2012 operative procedure B. SSI linked to the October 2012 operative procedure C. SSI linked to the Feb 2013 operative procedure D. Does not meet criteria for SSI Answer C. SSI linked to the Feb 2013 operative procedure Rationale • If a patient has several NZ SSI operative procedures performed on different dates prior to an infection, attribute the infection to the operation that was performed most closely in time prior to the infection date, unless there is evidence that the infection was associated with a different operation. Case 8 • A female patient underwent a KPRO operation on December 22nd 2012. She returned to her surgeon on January 31st 2013 with purulent drainage from the superficial incision, which had started 2 days prior. • How should this infection be reported? A. B. C. D. SSI – superficial SSI – Deep SSI – Organ/Space Not reported Answer & Rationale • Not reported – does not met criteria for SSI • Infection occurred > 30 days post-op therefore cannot be called SSI-superficial • Not readmitted to hospital