10.Mycology
advertisement

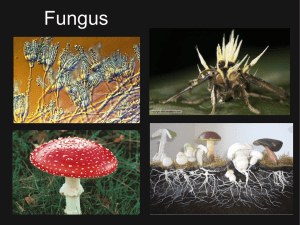
Mycology is the study of • • • • • • • • Beer Wine Bread Cheese Gourmet mushrooms Environmental toxins Biodegradation Diseases caused by fungi KINGDOM CHARACTERISTIC EXAMPLE Monera Prokaryocyte Bacteria Actinomyces Protista Eukaryocyte Protozoa Fungi Eukaryocyte * Fungi Plants Eukaryocyte Plants Moss Animals Eukaryocyte * Arthropods Mammals Man Fungi • Commonly present in nature as saprophytes, transiently colonising or etiological agenses. Frequently present in biological samples. They role in pathogenesis can be difficult to determine. Effect of fungi • Mycetismus – preformed toxins ergotamine alcaloids, psychotropic substances, • Mycotoxicoses – aflatoxines, chronical exposition • alergic reaction – air mycelium alergic pneumonia, rhinitis, bronchial asthma, aleveolitis, atopic reaction colonisation and disease – inborne immunity, diseases are short, self limiting • Infections Immunocompetent : superficial, skin, subcutaneous, systemic Immunocompromised and AIDS: fungi with low patogenicity – oportunictic mycoses Biology and classification • • • • • • • Eukaryoric cells Nucleus, nuclear membrane Multilayered rigid cell wall Cell wall with sterols, Without chlorophyll Not photosyntetic Heterotrophic metabolisme – saprophytic, comensals, parasits Biology and classification • Yeast - C. albicans One cell, asexual reproduction by budding (blastoconidia) or by division. They ca produce filamentous structueres resempling molds – pseudohyphae, elongated cells resembling sausages Biology and classification • Molds(hyphae) – elongation at both ends, can be multinucleated – coenocitic or septated The complex of hyphae is known as mycelium If implemented to the substrate – vegetative If on the surface - air – releasing specialised structures – conidia serving as propagation structures – asexual conidia, dissemination, identification Patogenic potential of fungi • Usually exogenous – exept. Candidosis • Longlasting exposition of man to fungi, • Pathogenesis depend on nonspecific immune mechanism – skin, mucous membrane, IDS • Presence of fatty acids, acidic pH, epitelium, physiological microbial agens, transferrin Tools of pathogenicity • Dermatophytes – co0lonisation of skin, hairs, nails – ensyme keratinase • Dimorfic fungi – as molds in the nature, as yeast in tissues Candida – yeast becomes filamentous during invasion of tissue • Capsule - Cryptococcus neoformans *Primary pathogens - Histoplazma capsulatum, Blastomyces dermatitis, Coccidioides immitis * Oportunistic pathogens - Aspergillus, Candida, Mucor MORE MYCOTIC INFECTION or REVIVED INTEREST IN MYCOLOGY 1. 2. 3. 4. 5. 6. 7. Increased frequency of mycotic diseases Increased awareness by physicians Better trained laboratory personnel More invasive procedures used on patients Increased use of immunosuppressive drugs Increase in immunosuppressive disease Better laboratory diagnostic tools Mycotic Diseases Are NOT Contagious with the exception of dermatofytes ESTABLISHMENT OF INFECTION WITH A MYCOTIC AGENT DEPENDS ON 1. Inoculum size 2. Resistance of the host Laboratory diagnosis • Primary pathogens – microscopy of tissue sample+cultivation • Oportunistic pathogens – often only contamination, ! Interpretation! Repeated isolation and presence of fungi in biological sample by microscopy * Methods of sampling - sterility, desinfection of the place of sampling (skin, nails, hairs) 70% etanol + dry, eschariation. * Procedure: material +10% KOH (destruction of tissue,, fungi pocess chitin that resist alkaline solution – mikrosscopy of hyphae – rice agar microscopy or staining sc. Gomori, Schiff - cultivation on selective media at 25 and 37.C Diagnosis 1. Wet Mount 2. Skin test 3. Serology 4. Fluorescent antibody 5. Biopsy and histopathology 6. Culture 7. DNA probes Cultivation media • Selective • Sabouraud agar - dextrose, pepton, less agar, pH 5,5 – acid environment and high concentration of glc • Saprophytic fungi can overgrow pathogenic – addition of chloramphenicol (against bacteria) and cyclohexamid (aganinst saprophytic fungi). • Recommendation of cultivation on media with and without ATB, always in 25 and 37*C ( some fungi do not grow at 37+ H. capsulatum) • Identification: all are G+, yeat are growing as bacterial colonies, fungi – longer – several days and even weeks, microscopy – rice agar block - morphology THERAPY Because they are eukaryotic, fungi are biochemically similar to the human host. Therefore it is difficult to develop chemotherapeutic agents that will destroy the invading fungus without harming the patient. Antimycotics • Polyensy - amfotericin B, nystatin Azoles – interference with ensymes depending on cytochromes and acting during demetylation of lanosterol to ergosterol - miconazol,ketoconazol, flukonazol, Nucleotides – inhibition of DNA a RNA synthesis - 5 fluorocytosin Grisanes – inhibition of the function of microtubules KJ – activation of lysosomal ensymes • Longlasting therapy, monitoring of the patient • Susceptibility testingovanie – not standardised IN FUNGAL THERAPY We attempt to induce cell injury by causing the cell membrane of the fungus to become permeable. PROBLEM Finding an agent that will selectively injure fungal cell walls without damaging the host cell. PRIMARY ANTI-FUNGAL AGENTS 1. Polyene derivatives – – Amphotericin B Nystatin 2. Azoles – – – – – Ketoconazole Fluconazole Itraconazole Voriconazole Posaconazole Mycoses • According to the tissue • Superficial – superficial layer of skin and hairs Skin – epidermis and adnexes Subsuperficial or subcutaneous - dermis, deeper tissues, muscles, fasciae - traumatic • Systemic – primary pathogenic fungi – endemic, dimorfic • Oportunistic – non pathogenic fungi, or fungi causing usually localised infection – spread and cause life threating infection Superficial • Cosmetic destruction of stratum corneum and cuticula of hair, without cell immunity reaction of the patients • Skin - Malassezia furfur (pityriasis versicolor) microscopically „spagetti look) - Exophiala wernecki ( tinea nigra) - microscopically, cutivation - dimorphismus – brown colonies and hyphae • Hairs - Piedraia hortoe (black piedra) – direct microscopy of hair - Trichosporon beigelii (white piedra) – direct microscopy of hair, dimorphismus • Th: keratolytical local substances (salicylates), miconazol – interfer synthesis of ergosterol, hygiene, relapsing Cutaneous - dermatophytes • Skin, hairs, nails – only on the areas of skin and adnexes containing keratin. Cell immunity reaction • Clinical manifestation – worm-like serpentin or ring-like • More than 100 species - dermatophytes. Trichophyton, Epidermophyton, Microsporum anthropofil (chronic anoying infections), zoophil and geophil dermatophytes (inflamatory reaction, selflimiting) – good prognosis Certain are endemic, age related • Therapy: skin – local - miconazol, clotrimazol, econazol hair - griseofulvin p.o., fungistatic • Laboratory diagnosis of dermatophytes Sampling and processing with KOH Microscopy - branching septated hyphae from skin and nails - spores in or surrounding hair - Trichophyton schoenleinii – vax-like substance of hyphae surrounding base of hair folicules – microscopy indentify just the mycotic ethiology. For species identification cultivation. Selektive medium with ATB and cyclohexamid at 25* - as long as 4 weeks. • mycelia are not diagnostic - microscopy and identification acc.to conidia Subcutaneous Mycoses • Confined to subcutaneous tissue and rarely spread systemically. The causative agents are soil organisms introduced into the extremities by trauma Subsuperficial, subcutaneous • Wide spectrum of infections usually after traumatic innoculation (thorn, tick, wood, nail – deeper layers, chronical process, spread under epidermis. • Localised usually on extremities • Dif. dg. actinomycoses, mycetoma, atypical mycobacteriosis. • Therapy can be frustrating, radical, surgery, amputation. • exotické • Sporothrix schencki – lymphocutanneous or disseminated • Mycetom • Other subcutaneous mycoses - zygomycosis, Mycetom - clinical unit - caused by bacteria (Actinomyces izraelí, Nocardia asteroides, Streptomyces, Actinomadura) or fungi (Madurella grisea, ) Dg: pus from liquid from sinuses - macroscopic granules, - microscopic Th: important to identify the ethiology bacterial or mycotic, total surgical excision, amputation Systemic Mycoses • Involve skin and deep viscera • May become widely disseminated • Predilection for specific organs Dimorphic Fungi • Yeast Form • Parasitic form • Tissue form • Cultured at 37 C • Mycelial Form • Saprophytic form • Cultured at 25 C Sytemic mycoses • Primary pathogenic: (dimorfic - Histoplasma capsulatum, Blastomyces detmatitidis, paracoccidioides brasiliensis, Coccidioides immitis Crytococcus neoformans • C. neoformans – is the only monomorfic - at 25 and 37* yeast, mucopolysacharide capsule • Primary place of infectione - lung – usually asymptomatic infection. If sec. spread - dissemination • Usually endemic • Cryptococcosis – torulosis, european blastomycoses. Not dimorphismus: 4 serotypes A,D and C,B Virulence - capsule - asymptomatic lung disease – solitary lung nodul – imitation of Ca, symptomatic pneumonia – difuse infiltration - hematogenous dissemination - meningitis (headache, longlasting fever, - skin lesions, lysis of bones. Dg detection of antigen – polysacharide capsule - latex agglutination Burri method. Cultivation Discrimination of pathogenic and not pathogenic – growth at 41*C – patogenic do not grow Th amfotericin B, 5 fluorocytosin CNS - 10 weeks, • Blastomycosiss - lung disease, often innaparent, later ulceros lesion on skin and bones. Dg. – serology immunodiffusion, skin test, cultivation of the tissue and microscopy – budding yeast cells. Identification by dimorfismus. Th - amphotericin B, in non complicated lung ketokonazol • Coccidioidomykóza - inhalation, asymptomatic or life threating, meningitis. Dimorphismus – filamentous in the nature (cylindric conidia). In the tissue multinuclear structures changing to endospores with one nucleus growing and developing to new spherules Endemic. Dg. Serology imunodifusion, precipitation (early stages) or CF(later stages), skin test Th. Amfotericin B (poorly enter to CSM). Ketokonazol – intrruption of the infection - relapses after interruption of the therapypo prerušení liečby. • Paracoccidioidomycosis – lung disease after inhalation – asymptomatic, or ulcerouse forme in mouth or nos or progresive lung or systemic infection. • Clinically usually in men • Dimorfic – mold in nature, yeast in tissue diagnostic Dg. Serology immunodiffusion, histology, cultivation 14 days at 25*C - mycelium – transport to 37*C – change of the phase – to yeast • microscopy („ captain wheele“ – central cell with • Histoplasmosis - asymptomatic or influenza-like, big exposition – pneumonia with rare complications – pericarditis, fibrosis of mediastinum.Diseminated in immunocompromised. • Dg.-serologically CFR, imunodifusion (antigen histoplasmin – • - histological, - cultivation (sputum, microscopy - long. - skin test with histoplasmin (questionable). - Ag detection in blood and urine. • Th: amfotericin B Oportunistic mycoses • Usually well tolerated without sequelae with the exception of alergic hypersensitivity. • High degree of inborne resistance against colonisation with fungi, low degree of virulence of fungi • If immunodeficiency – life threating diseases (AIDS, drugs, irradiation, cytotoxic therapy) • Most common - Candida albigans, Aspergillus fumigatus, Rhizopus - • • • • • • Candidosis Candida sp. – part of normal physiological microbial flora (mucous membrane of mouth, vagina, rectum), colonisation without symptomes. Seldom on skin. Hemataogenous dissemination from oropharynx or GIT if injury of m.m., chemtherapy, contaminated catheters (usually endogenous infection Lung, spleen, kidneys, liver, heart, brain, eye, skin lesion during dissemination. Hemocultivation is usually negative. Localised infection of skin and nails (dif.dg.from dermatophytosis) Infection of m.m. of mouth, vagina, aesophagus, brochi Chronic mucocutaneous candidosis Disseminated candidosis Imunity – mostly cellular Th: local for skin and mucocutaneous inf. Systemic and nail -amfotericín B a 5 fluorocytozín, ketokonazol Dg of candidosis • Usually blastospores, pseudohyphae and septated hyphae. • C.glabrata –only yeast • Colonies - big, cream like • Rapid test of - C. albicans - germ tubes test – hyphae propagules when cultivated in human serum Aspergilosis • Aspergilosis - exogenous infection • . A. flavus, A. fumigatus. • Cause only opportunistic infections. Alergic aspergilosis, secundary colonisation, systemic aspergilosis • Lab.dg.: regularly septated hyphae, oriented in one direction in the sample • Cultivation usually negative • Invasive disease – repeated isolation from the same place zygomycosis • Zygomycosis (mucormycosisa, phycomycosis) - usually in the environment • Similar to asperfilosis • Coenocitic hyphae • Infection from paranasal sinuses, spreading to orbita and brain • Terminal stage of patients in acidosis in metabolic disorders (DM) • Invasive after colonisation of burned places • When disseminating – predilection to big vessels, embolisation, ischemia, necrosis • .Dg.: filamentose, coenocytic Opportunistic Mycoses Infections due to fungi of low virulence in patients who are immunologically compromised PATHOGENIC FUNGI • NORMAL HOST • • • • Systemic pathogens - 25 species Cutaneous pathogens - 33 species Subcutaneous pathogens - 10 species IMMUNOCOMPROMISED HOST Opportunistic fungi - 300 species HOST-PATHOGEN EQUILIBRIUM NUMBER OF ORGANISMS X VIRULENCE HOST RESISTANCE = DISEASE Opportunistic Fungi 1. Saprophytic - from the environment 2. Endogenous – a commensal organism MOST SERIOUS OPPORTUNISTIC INFECTIONS • CANDIDA SPECIES • ASPERGILLUS SPECIES • MUCOR SPECIES (ZYGOMYCES) CLINICAL PRESENTATION 1. 2. 3. 4. 5. Atypical Signs and Symptoms Unusual Organ Affinity Outside Endemic Area Unusual histopathology Unusual Pathogens CLINICAL PRESENTATION 1. 2. 3. 4. 5. Atypical Signs and Symptoms Unusual Organ Affinity Outside Endemic Area Unusual histopathology Unusual Pathogens CLINICAL PRESENTATION 1. 2. 3. 4. 5. Atypical Signs and Symptoms Unusual Organ Affinity Outside Endemic Area Unusual histopathology Unusual Pathogens CLINICAL PRESENTATION 1. 2. 3. 4. 5. Atypical Signs and Symptoms Unusual Organ Affinity Outside Endemic Area Unusual Histopathology Unusual Pathogens CLINICAL PRESENTATION 1. 2. 3. 4. 5. Atypical Signs and Symptoms Unusual Organ Affinity Outside Endemic Area Unusual histopathology Unusual Pathogens MYCOLGISTS have more FUNGI