Blood component preparation
advertisement

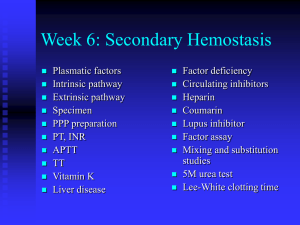
BLOOD AND ITS COMPONENTS BLOOD IS VITAL TO LIFE ,OR WE CAN SAY BLOOD IS LIFE. In INDIA blood transfusion was first started in School Of Tropical medicine. Calcutta,1939, with out any scope for group matching. As this procedure was unscientific a committee was formed for establishment of blood bank in Calcutta. Ultimately a small blood bank was started in the dept of Serology, School Of Tropical Medicine named as RED CROSS BLOOD BANK. Later it was shifted to Maniktala as Central Blood bank. Pundit Jawhar Lal Nehru donated blood in Calcutta in 1946. • In spite of dynamic progress in the field medical science, the life saving role of blood is yet with out parallel, even in the 21st century. • Blood is still the most essential factor in saving a life. • In INDIA total requirement of blood is approximately 80,00,000.units per year, where as its collection from voluntary donors does not exceed a total of 50,00,000units even after almost 60 years of independence. Contd. • In a statistical study it is seen that total no of blood donation in West Bengal- 713535 (Vol. 85.71%) Bihar – 47863 (Vol. 22.74%) Jharkhand --- 73238 (Vol. 33.13%) Uttar Pradesh- 394699 (Vol. 17.3%) Maharashtra- 377110 (Vol. 86.36%) Preservation and storage of Blood Since 1978 citrate-phosphate-dextrose with adenine (CPDA-1) is used as blood preservative for 35 days at 2-40C. Action of ingredients of anticoagulant solution. Citrate Sodium diphospate Prevents coagulation by chelating calcium Prevents fall in pH Glucose Supports ATP generation by glycolytic pathways Adenine Synthesizes ATP, increases level of ATP, extends the self life of RBC to 42 days. Action of ingredients of anticoagulant solution. - Blood pH on day of collection is 7.5 and on 35th day become 6.84. - A fall in pH in the stored blood results in a decrease in red cell 2, 3-DPG level, which results in increase in hemoglobin-oxygen affinity. CPDA-1 maintains adequate levels of 2,3-DPG for 10 -14 days. - During storage Na+ and K+ leak through the red cell membrane rapidly. K+ loss is greater than Na+ gain during storage. Biochemical changes in stored blood Characteristics Days of storage Whole blood RBC conc. 0 35 0 35 % viable cells (24 hrs after transfusion) 100 79 100 71 pH (Measured at 370C) 7.55 6.98 7.60 6.71 Biochemical changes in stored blood Characteristics Whole blood RBC 2, 3-DPG (% initial value) Plasma K (m.mol/l) 100 <10 100 <10 5.1 27.3 4.2 78.5 Plasma Na (m.mol/l) 169 155 Plasma Hb (mg/l) 78 461 111 82 658 Transfusion Reactions Reaction Acute (within 24 hours) ImmuneMediated Haemolytic Febrile non hemolytic Allergic anaphylactic TR-acute lung injury. Haemolytic Alloimmunization Post transfusion purpura Graft-Vs-host disease Non-Immune Mediated Bacterial contamination Circulatory overload hyperkalemia Hepatitis B & C HIV 1&2 Syphilis Malaria Iron over load Delayed (within days or month Inspection of blood Blood should be inspected before transfusion for possible bacterial contamination, haemolysis, visible clots, brown or red plasma. Plasma with a green hue should not to be rejected because this is caused by exposure of bilirubin pigment to the light. Yersinia enterocolitica can grow at 40C and the blood is haemolysed. Importance of component separation Separation of blood into component allows optimal survival of each constituents Component separation allows transfusion of only specific desired component to the patient Transfusion of only the specific constituent of the blood avoids the use of unnecessary component By using blood components several patient can be treated with the blood from one donor Blood Components (cellular & plasma) & Plasma Derivatives Cellular components • Red cell concentrate • Leucocytes-reduced red cells • Platelet concentrates • Leucocytes-reduced platelet concentrates • Platelet Apheresis • Granulocytes, Apheresis Contd. Plasma Components • • • • Fresh frozen plasma Single donor plasma Cryoprecipitate Cryo-poor plasma Plasma derivatives • • • • • • Albumin 5% & 25% Plasma protein fractions Factor viii concentrate Immunoglobulin Fibrinogen Other coagulation factors Preparation of blood component is possible due to Multiple Poly Vinyl Chloride (PVC) pack system Refrigerated centrifuge Different specific gravity of cellular components ◦ Red cells spg. 1.08-1.09 ◦ Platelet spg. 1.03-1.04 ◦ Plasma spg. 1.02-1.03 Due to different specific gravity of cellular components, they can be separated by centrifuging at diff g for diff time. Centrifugation for blood component preparation The components are prepared by centrifuging at diff relative centrifugal force at diff time. Relative Centrifugal Force in g =118 x10-7 x r x N2 Precautions to be observed in preparing components In collection of blood • proper selection of donor • Clean & aseptic venepuncture site to minimize bacterial contamination • Clean venepuncture with minimum tissue trauma and free flow of blood • The flow of blood should be uninterrupted and continuous. If any unit takes more than 8 minutes to draw, it is not suitable for preparation of blood components. • A correct amount of blood proportionate to anti coagulant should be collected in primary bag that has satellite bags attached with integral tubing. Contd. • Monitor the collection of blood with automatic mixer which is used for collecting the desired amount of blood and mixing the blood with anticoagulant • If platelets are to be harvested the blood bag should be kept at room temperature 20-240C until platelets are separated. Platelets should be separated within 6 hours from the time of collection of blood. • Triple packs system with two attached bags makes it possible to make red cells, platelet concentrate and fresh frozen plasma. While quad packs system with three attached bags are used for preparing red cells, platelets concentrate , cryoprecipitate (factor viii) and cryo-poor plasma. Double bags are used making red cells and Platelet rich plasma only. Blood Component Separation centrifuge blood pl.rich plasma PRBC centrifuge at 20o freeze -700c pl.poor plasma platelet frozen RBC leuco poorRBC FFP cryo poor plasma cryoprecipitate Whole Whole Blood Whole blood contains 450+63 ml or 350+49 ml of blood plus anticoagulant solution. The anticoagulant used is CPDA-1. Whole blood has a hematocrit of 30-40 percent. Minimum 70% of transfused red cells should survive in the recipient’s circulation 24 hrs after transfusion. Stored blood has no functional platelets and no labile coagulation factors V and VIII. Preparation of Red Blood Cell Concentrates Red blood cells are prepared by removing most of the plasma from a unit of fresh blood. Red blood cells preparations are: ◦ Sedimented red cells: They have a PCV of 60-70%, 30 % of plasma & all original leucocytes and platelets. Kept at 2-60C. ◦ Centrifuged red cells: They have a PCV of 70-80 percent, 15 % of plasma and all original leucocytes and platelets. Kept at 2-60C. ◦ Red cells with additive (Adsol or SAG-M): They have PCV of 50-60 Percent, minimum plasma and all leucocytes and platelets. Usually kept at 2-40C. Leukocytes-Reduced Blood Components Leukocytes in blood components can cause: – – – – – – Non hemolytic febrile transfusion reactions (NHFTR) Human leukocyte antigen (HLA) alloimmunisation. Transfusion of Leukotropic viruses eg. CMV, EBV, HTLV1. Transfusion related GVHD Transfusion related acute lung injury (TRALI) Transfusion related immunosuppression. Contd. Cytokines are generated by leukocytes, even at 260C but to a much greater extent at 20-240C. Cytokine level rise in direct proportion to the number of leukocyte. Hence leuko-reduction before storage in blood bank is much better than post storage bed side leuko-reduction . Reducing the leukocyte content <5x106 in one unit of RBCs prevents non hemolytic febrile transfusion reactions (NHFTR) and HLA alloimmunisation or transmission of CMV. Methods of Preparation of LeukocytesReduced Red Cells Centrifugation and removing of Buffy coat Filtration Washing of red cells with saline Freezing and thawing of red cells leuko-reduction can be done at three diff points 1. 2. 3. Prestorage leuko-reduction Post storage leuko-reduction Bedside filtration Impact of pre-storage leuko-reduction Results from pre-storage leuko-reduction ◦ Cytokine production is reduced or eliminated ◦ White cells are removed before fragmentation transmission ◦ Tumor metastasis are immunomodulation reduced . Potential patient benefit Decrease in NHFTRs Decrease alloimmunization Decrease virus Prevent Preparation of Platelet Rich Plasma & Platelet Rich Concentrate Are prepared from • 450 ml of fresh blood by centrifugation or Aphaeresis. • A unit of platelet concentrate prepared from 450 ml of fresh blood contains: – Plasma vol. – Platelet yield – WBC – RBC – pH 40-70ml. 5.5x1010 ≥108 traces to 0.5ml. 6.0 or more Calculation of Platelet Yield – Number of platelet in blood= platelet per mm3 x1000 x vol. of blood (ml) – Number of platelet in PRP = platelet per mm3 x 1000 x vol. of PRP (ml.) – Number of platelet in P.C. = platelet per mm3 x 1000 x vol. of P.C. (ml.) Calculation: – % of platelet yield in PRP= Number of platelet in PRP x100/ Number of platelet in blood – % of platelet yield in P.C.= PRP Number of platelet in P.C. x100/ Number of platelet in Precaution and storage pH should never fall below 6. A decline in pH causes ◦ Changes in shape of platelets from disc to sphere ◦ Pseudopod formation ◦ Release of platelets granules The above changes are responsible for low recovery and poor survival of platelets in vivo. Agitation during storage helps the exchange of gases, maintenances of pH, & reduce formation of platelet aggregates. Granulocyte Concentrates Granulocyte concentrates prepared by Single donor unit Leukapheresis by blood cell separators As the specific gravity of red cells and granulocytes is very similar, the separation of granulocytes by centrifugation is not satisfactory. Leukapheresis is a better method. Granulocytes can be stored at 20-240C but they should be used within 8 hrs. & not later than 24 hrs from blood collection. Fresh Frozen Plasma (FFP) It contains all coagulation factors & great care must be taken during collection of blood , freezing and thawing to preserve their activity. Collection of blood : 1. Blood should be collected le by a clean, single venepuncture. 2. Flow of blood should be rapid and constant. 3. Total time taken to collect 450 ml of blood should not be more than 8 minutes. The most labile coagulation factors are preserved for one yr. if FFP is kept at -300C or below. If FFP is not used within one yr. it is redesignated as Single Donor Plasma which can be kept further for 4 yrs at -300C or below. The FFP should be administered as soon as possible after thawing, and in any event within 12 hrs. if kept at 2-60C. Cryoprecipitate Cryoprecipitate are precipitated proteins of plasma rich in Factor VIII and fibrinogen, obtained from a single unit of fresh plasma ( approximately 200 ml.) by rapid freezing within 6 hrs of collection. Factors improve the yield of Factor VIII in Cryoprecipitate 1. Clean single venepuncture at first attempt 2. Rapid flow of blood, donation of blood (450ml) obtained in less than 8-10 mins should be used 3. Adequate mixing of blood and anticoagulant 4. Rapid freezing of plasma as soon as possible after collection in any case within 6-8 hrs after collection as done for preparing FFP. 5. Rapid thaw at 40C in circulating water bath. Storage and shelf life of Cryoprecipitate: One yr at -300C or below. After reconstitution Cryoprecipitate should be kept at 2-60C and administered within 4 hrs. Single Donor Plasma Single donor plasma can be prepared by separating it from red cells any time up to 5 days after the expiration of the whole blood unit. When stored at -200C or lower, single donor plasma may be kept up to 5 yrs. A prolonged pre separation storage period increases its contents of potassium & ammonia. It has no labile coagulation activity. Cryoprecipitate Poor Plasma • It is a by-product of cryoprecipitate preparation. • It lacks labile clotting factors V and VIII and fibrinogen. • It contains adequate levels of stable clotting factors II, VII, IX & X. • It is frozen and stored at -200C or lower temperature for 5 yrs. Indications, Contraindications & Complications of Diff Blood Components BLOOD TYPES Fresh Blood Whole blood or RBC concentrates less than 12-24 hours old form the time of collection are considered as Fresh Blood • Whole Blood • Blood after 24 hours of collection to 35 days are considered as Whole Blood (without platelet and labile clotting factor) Fresh blood In new born exchange transfusion open heart surgery Hyperkalemia Renal failure One unit increases 0.8 gm% hemoglobin in adult Disadvantages of Fresh blood transfusion 1. Chance of transfusion of cytomegalovirus virus, Human T- Cell Lymphotropic virus type I & II, E.B Virus, Treponema pallidum 2. Non –hemolytic febrile transfusion reaction 3. Transfusion Related Acute Lung Injury (TRALI) results pulmonary oedema Cytomegalovirus (CMV) CMV is a common human pathogen and present in sub clinical stage in 90 % adults. - It is the common cause of congenital defects eg. Microcephaly, Intra cerebral calcification, mental retardation, unilateral or bilateral hearing loss. Viruses are shed in most of the body fluids. It infect the mononuclear leucocytes. Whole blood Blood after 24 hours of collection to 35 days are considered as Whole Blood (without platelet and labile clotting factor) Indication 1. Symptomatic decrease in oxygen – carrying capacity combined with hypovolemia. 2. More than 30% blood loss in acute haemorrhage. 3. Anticipated surgical blood loss more than 1 litre . 4. Source of protein with oncotic property. 5. Source of Non-labile coagulation factors. 6. Inoperative blood loss more than 15%. Whole blood Disadvantages 1. Less oxygen carrying capacity and more potassium accumulation. 2. Low level of 2, 3 –di- phosphoglycerate which is important in premature neonates, patient with impaired cardiac function, haemorrhagic shock, respiratory distress syndrome. 3. Develop C.C.F in severe anemic patient. 4. Contraindicated in multiple transfusion Whole blood Complication 1.Dilutional thrombocytopenia 2. C.C.F Red blood cell concentrate (packed Red Cell) are prepared by removing most of the plasma from a unit of whole blood. Indication: 1. 2. 3. 4. 5. 6. Urgent operation with haemoglobin less than 10 gm% Anaemia associated with cardiac failure. Haemoglobin less than 6 gm% Approaching delivery and haemoglobin less than 7 gm% Liberal guideline in thalassaemia major Anticipated surgical blood loss more than one litre RBC concentrate contra-indication 1. Chronic renal failure 2. Pre-operative transfusion to raise hemoglobin above 10gm% 3. Nutritional Anaemia 4. To enhance general well being, promote healing, prevent infection Platelet Concentrate (Production of platelets are approx. 40000/microlitre/day) 1 unit platelet increases 7000/microlitre platelet count in adult, 80000/microlitre in infants, 20000 /microlitre in Child of 18 kg body wt. Platelet Concentrate (Production of platelets are approx. 40000/microlitre/day). Indication: 1. Count less than 5000/microlitre regardless clinical condition 2. Count is around 20000/microlitre with thrombocytopenic bleeding or increase risk of bleeding in acute leukaemia or chemotherapy 3. Count is around 60000/microlitre with DIC or before major surgery. Administration of ABO incompatible platelet is an acceptable transfusion practice, but not Rh incompatible platelet. Platelet Concentrate Complication 1.Chill, Fever, Allergic reaction 2.Infusion of Bacteria 3.Alloimmunisation 4.Platelet refractory state 5.Graft vs. host disease Platelet concentrate contra-indication 1. ITP 2. TTP 3. Heparin induced thrombocytopenia 4. No role in routine open heart surgery 5. Invasive procedure where count is more than 50000/microlitre 6. Bleeding unrelated to decrease platelet number and function. Fresh frozen plasma Indication 1. Actively bleeding and multiple coagulation factor deficiency 2. Liver Diseases 3. DIC 4. Coagulopathy in massive transfusion 5. TTP 6. Von Willebrand disease Fresh frozen plasma contra-indication 1. Should not be used as blood volume expander 2. Hypoproteinaemia 3. When prothrombine time is less than 18 second 4. Source of immunoglobin Limitations 1.Components must be prepared within 6 hours from collection time 2.Needs costly instruments and infrastructures and specially trained personnel Plasma Derivatives & Plasma Substitutes Plasma protein solutions Plasma protein solutions are prepared from pooled plasma after removal of factor viii conc., fibrinogen & immunoglobulin – Albumin preparation • • • Albumin 5% soln. Albumin 25% soln. contain 96% alb & 4% globulin Plasma protein fraction (PPF) 5% soln. Contain 83% alb. & 17% globulin Characteristics of Albumin Preparation The 5% soln. are osmotically and oncotically equivalent to plasma, 25 % soln. is five times that of plasma Products are heated and chemically treated to reduce the risk of viral disease transmission mainly the viruses that have lipid envelope eg.HIV1 & 2, Hepatitis B&C, HTLV1&2 Shelf life depends on the storage temperature— ◦ room temp----3yrs Indications 5% albumin & PPF ◦ Blood volume expansion & colloid replacement ◦ Hypoproteinemia following burn & extensive surgery ◦ The replacement fluid in therapeutic plasma exchange ◦ Hemorrhagic hypovolemic shock ◦ Retroperitoneal surgery in which large vol. of protein rich fluid may pool in bowel ◦ 25% albumin Severe Hypoproteinemia in acute nephrotic syndrome & acute liver disease Hyperbillirubinemia in the new born Toxemia in pregnancy Adverse Effect & Contraindication • Adverse effects – Urticaria and anaphylactoid reactions – Circulatory overload – Febrile reactions – Hypotension due to vasoactive substances in plasma – Contraindications • Hypoproteinemia in malnutrition • Chronic Nephrotic syndrome • Cirrhosis of liver Factor VIII Concentrate Preparations available ◦ ◦ ◦ Factor viii prepared from large pools of plasma is sterile , lyophilized Commercially prepared by recombinant DNA technology Storage Freeze dried products are stored at 2-60C Indications ◦ ◦ ◦ Hemophilia A Hemophilia A with low levels of inhibitors of factor viii Von-Willibrand disease Immunoglobulin preparation • Immunoglobulin for IM use: A concentrated solution of the IgG component of plasma prepared from large pools plasma of donors containing antibodies against infectious agents • Indication – Congenital Hypogammaglobinemia – Persons exposed to diseases like Hepatitis A or Measles • Immunoglobulin for IV use: – Indications • Idiopathic autoimmune thrombocytopenic purpura • Treatment of immune deficiency states • Hypogammaglobinemia • Myasthenia gravis • HIV related disease Contd. • Hyper immune Globulin Used for prevention of diseases like Hepatitis B, Varicella Zoster, Rabies, mumps & others • Anti-Rh (D) Immunoglobulin (anti-D RHIG) prepared from plasma containing high level of AntiRh D antibody from previously immunized persons. Indication: To prevent Rh (D) negative mother from Rh immunization who is pregnant with Rh. (D) positive infant.