Orthopedic Injuries
advertisement
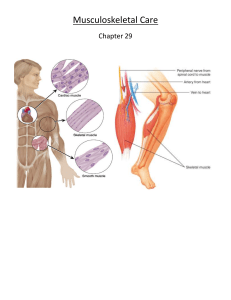
Orthopedic Trauma Andrea L. Williams, PhD, RN Emergency Education & Trauma Program Specialist Associate Clinical Professor UWHC & UW-SON Name that Injury! Name that Injury! Name that Injury! Name that Injury! Name that Injury! Name that Injury! Name that Injury! Name that Injury! Name that Injury! Name that Injury! Name that Injury! Name that Injury! Associated Conditions • Hemorrhage – Shock (~2L pelvis, 1L thigh & 500 ml tibia) • Instability • Loss of tissue • Laceration with contamination • Interrupted blood supply – Ischemia • Nerve damage • Long-term Disability Sprains • Partial tear of a ligament by twisting & stretching of a joint beyond normal ROM – 1st Degree Sprain – No instability, few fibers torn. Minimal hemorrhage & swelling – 2nd Degree Sprain – No instability, ligaments partally torn, swelling and hemorrhage – 3rd Degree Sprain – Unstable, ligaments completely, with significant swelling & hemorrhage. Sprained Knee Strains & Ruptures • Strain - Injury to a muscle or tendon from overexertion (back, arms, calf) • Severe strains can cause bone avulsion Joint Dislocations • Dislocation – Articulating surfaces of 2 bones are displaced – – – – Luxation – Complete dislocation Subluxation – Incomplete dislocation Rotator Cuff injuries – Usually deltoid Common sites • Shoulders, elbows, fingers, knees, & ankles – Complications • Posterior popliteal injury Principles of Splinting (p. 1238) • Splint joints and fractures above & below injuries • Cover open fractures • Document pulses, sensation, motor function before & after splinting • Stabilize the limb with gentle in-line traction to a position of normal alignment • Immobilize dislocations in a position of comfort with • Ice, cold compresses • Elevation – to or just below level of heart Shoulder Injuries • Dislocations • Subluxations • Rotator cuff tendon injuries • Sternoclavicular strain • Treatment – Neurovascular status – Splint in position found or – Sling & secure to body – Ice or cold compresses Elbow Injuries • Falling on an outstretched arm or flexed elbow • Pulled elbow – Nursemaids elbow from a sudden lateral force • Athletic injury • Complications – Volkmann’s contracture – Claw-like contraction of hand & arm deformity from ischemia – Laceration of brachial artery – Ulnar nerve damage • Treatment – Check neurovascular status – Splint in position found – Ice or cold compresses Radial, Ulnar, Wrist Injuries • Check neurovascular status • Splint in position found (rigid or formable • Ice & elevation Hand Injury • Boxer’s fracture 5th metatarsal bone • Treatment – Check neurovascular status – Splint (rigid or semiformable) in position of function – Ice & elevation Finger Injuries • Assess neurovascular status • Splint in foam filled aluminum splint, with tongue blades, or tape to adjacent finger • Ice & elevation Pelvic Injuries • • • • Signs & Symptoms Pain Hypovolemic shock Shortening or abnormal rotation of affected extremity Associated with injuries to the bladder, urethra, reproductive organs & sacral nerves Pelvic Injuries Treatment of Pelvic Fractures/Ring Injuries • Open book – Vacuum mattress, Pelvic Binder, or sheet • Control hemorrhage – Direct pressure or close pelvic ring • Fluid volume replacement – Normal Saline (ED - PRBC, FFP, Platelets., Factor VII A &/or embolization) External fixation/ORIF Classification of Long Bone Injuries • Fractures – – – – – – – – – Complete or incomplete Open or closed Epiphyseal – Cause bending or deformity Comminuted – Several breaks in the bone Greenstick - Break in periosteum w/i bowing or buckling Spiral – Twisted or circular break. ↑ child abuse Oblique – Diagonal, slanting break Transverse – Right angle fracture Pathological Long Bone Fractures • • • • Pathophysiology Femur fractures result from major force Long bone fractures from falls, MVC, MCC Femur neck fractures common in elderly Blood loss into a femur – 1,000-1,500 ml Long Bone Fractures • • • • • • Signs & Symptoms Pain Ecchymosis & edema of the site Deformity at the site Shortening of affected extremity Internal or external rotation Hypovolemia or hypovolemic shock Long Bone Fractures Assessment • Circulation – Hemorrhage or ischemia – Neurovascular status – Pulses • Deformity – Edema, hematoma, wounds • Compartment Syndrome – 6 P’s – Pain, Pallor, Parasthesia, Pulses, Paralysis, Pressure Long Bone Fractures Treatment • • • • • Immobilize Splint Control pain Realign – In ED Skeletal traction – (In ED) Usually temporary. Weights must hang free, meticulous skin care • External fixators • ORIF Splinting • Types of splints – Rigid splint – body part fit to splint design – Soft or formable splint – molded to shape or configuration of the body part – Traction splint – (Femur fractures) – traction to stabilize and align Open Fractures • • • • • Signs & Symptoms Evidence of skin disruption over a fracture Protrusion of bone through an open wound Pain Neurovascular compromise Bleeding Open Fractures • • • • • • • • Treatment Cover the wound Splint ED or OR Wound cleansing & debridement Realignment Splint/Cast External fixation ORIF Complications osteomyelitis, cellulitis Techniques for Realignment • • • • • Finger realignment Shouldar realignment Hip realignment Knee realignment Ankle realignment Jumper Syndrome • Vertical deceleration • Forces transmitted upwards from lower extremities, pelvis, spine, chest • Lower extremity fractures & spinal cord injuries • Retroperitoneal hemorrhage is the most common cause of shock Amputations • • • • Classification Partial Complete Usually involves digits, foot, lower leg, hand or forearm Life over limb considerations Amputations Classification • Partial • Complete • Usually involves digits, foot, lower leg, hand or forearm • Life over limb considerations • Re-implantation (Favorable in Peds & with guillotine-type amputations) Amputations • • • • Signs & Symptoms Obvious tissue loss Pain Bleeding Hypovolemic shock Amputations • • • • • Treatment Reattachment Amputation Rehabilitation Prosthesis Clinic Assessment & Care Keep body part bagged not directly on ice Compartment Syndrome • • • • • • Signs & Symptoms Pain disproportionate to injury Sensory deficit Progressive muscle weakness Tense swollen area Elevated compartment pressures Loss of pulses Compartment Syndrome Treatment • Elevation of limb not above heart level • Placement of an intracompartmental monitor – <20 = normal – >20 = ischemia – > 30 = necrosis • Fasciotomies to release the pressure