Skin & Wound Care Considerations in Special
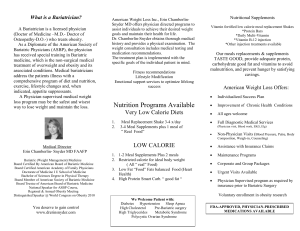
advertisement

Skin & Wound Care Considerations in Special Populations: Bariatric Tucson Affiliate of the WOCN Society Conference March 8, 2014 Karen Lou Kennedy-Evens RN, FNP, APRN-BC Learning Objectives • Describe the top three most common skin challenges in the bariatric population. • Discuss the pathogenic factors contributing to these common alterations in skin integrity. • Review the skin and wound care considerations of the most commonly seen skin challenges in the obese population. Incidence of Obesity • 35% of the world’s adults over 20 are overweight • World wide obesity has doubled since 1980 Future Generation Obesity increases risk of: • • • • • • Hypertension Type 2 diabetes Coronary heart disease Abnormal lipid concentrations Delayed wound healing Admissions to acute care, home care and out patient clinics • Prolonged acute care to prevent complications One-third of critical care patients are obese or morbidly obese. Comorbities Associated with Obesity • • • • • • • • • • • Hypertension Ischemic heart disease Type 2 diabetes Stroke Osteoarthritis Chronic renal failure Obstructive sleep apnea Restrictive lung disease Immobility Depression Metabolic syndrome • • • • • • • • Ovarian cancer Breast cancer Irritable bowel syndrome Nonalcoholic fatty liver disease GERD Colon cancer Disorders of the gall bladder esophageal cancer Surgical/Post-op Complications • • • • Risks of sepsis • Systemic inflammatory response syndrome (SIRS) Wound infections • Multi-organ dysfunction Dehiscence syndrome (MODS) Venous thromboembolic • Increase risk for skin disorders breakdown and wound deterioration. Loss is Skin Integrity due to: • Adipose has less blood supply inadequate oxygenation • Excessive sweating increases skin moisture and risk of bacterial/fungal invasion especially in deep folds • Immobility friction and shear due to weight stress • Malnutrition • Iatrogenic injury due to tubes, catheters and other interventions Skin Changes with Obesity • • • • Stretch marks (striae) Hirsutism in women Aerochordons (skin tags) Acanthosis nigricans Specific Skin/Wound Issues • • • • • • • • • • • • Atypical pressure ulcers Perigenital irritant dermatitis Intertrigo Fungal infections Cellulitis Fournier’s gangrene Erythrasma Diabetic foot ulcers Venous insufficiency with possible ulceration Lymphedema Abdominal elephantiasis Surgical site infections – increased chance of dehiscence and evisceration. Atypical Pressure Ulcers • Skin folds that create pressure on each other – – – – – – Neck Upper back Upper medial thigh Flanks Posterior legs Pannus • No risk assessment scales validated for the obese Interventions • • • • • • Relief of pressure Skin fold management Moisture management Appropriate sized beds for repositioning Adequate staff for repositioning Fabrics Perigenital Irritant Dermatitis • Due to urinary and/or fecal incontinence • Inability for self-care after toileting • Environment not set up for bariatric clientele resulting in unable to cleanse and dry the urethral and rectal orifices/without the danger of falling Intervention • Easy cleaning with appropriate equipment & supplies – – – – – – – – Toilet risers Extra wide toilet seats Bariatric commodes Hand rails for support Prepackaged cleansing & protection Perineal care with each incident Appropriate sized briefs and/or pads Drying fabrics Intertrigo • Maceration due to excess moisture • Infectious or noninfectious • Friction from two opposed skin surfaces • painful and/or pruritic • Presents as: – Erythematous, macerated plaques – Erosions with possible scaling – Candida intertrigo: satellite papulopustules – Found in perineal area, deep skin folds Interventions • • • • Topical or oral antifungal Drying agents Fans or cool hair dryer Special textiles with drying and antimicrobial properties Barriers to Skin Care • Body habitus • Lack of bariatric equipment • Inappropriate environmental design • Caregivers fatigue Bariatric Equipment Staff/Patient/Family Education • • • • • • Bathing & hygiene Skin fold management Perigental care Toileting Odor management Caregiver injury prevention Educational Props Other issues • Psychosocial issues • Bariatric-specific surgery References • • • • • • Beitz, J., Providing quality skin and wound care for the bariatric patient: An overview of clinical challenges . Ostomy Wound Management. Jan 2014 Blackett A., Gallagher S., Dugan S., Gates J., Henn T., Kennedy-Evens K., Lutz J., Caring for persons with bariatric health care issues. Journal Wound Ostomy Continence Nursing. 2011 Gallagher, S., The intersection of ostomy and wound management, obesity and associated science. Ostomy Wound Management Jan 2014 Rush A, Muir M. Maintaining skin integrity in bariatric patients. Journal of Community Nursing. 2012 World Health Organization. Obesity and Overweight. 2013. www.who.int/mediacentre/factssheet/ Wound Ostomy Continence Nurses Society. Safety and Comfort issues for Nursing Care of the Obese Patient. Mt. Laurel, NJ. WOCN 2013