Chapter 40 Nursing Care of Clients with Eye and Ear Disorders Fall
advertisement

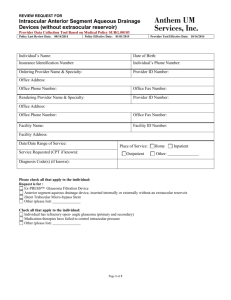
Nursing Care of Clients with Eye and Ear Disorders Chapter 40 Physical Assessment of Eye and Vision Snellen chart or E chart for testing visional acuity Cardinal fields 20 feet test for extraocular eye movements Cover-uncover test test for stabisms Physical Assessment of Ear and Hearing Hearing Weber test Rinne test Whisper test Eye Disorders Age Related Vision Changes flatting of the cornea pupillary constriction decrease in lens elasticity loss of sensory cells Physical changes inversion, eversion of lid, decreased tear secretion, “hollowed-eyed” Conjunctivitis-red, pain, itchy, sticky drainage Eye Disorders Inflammatory Disorders conjunctivitis inflammation of the conjunctiva bacterial or viral Treatment topical anti-infectives anti-inflammatories Eye Disorders Corneal Infections/Inflammations corneal scarring and ulcerations are a major cause of world-wide blindness Treatment Corneal Transplant The Client with Eye Trauma Corneal Abrasion Burns Penetrating Trauma Blunt Trauma Treatment topical anesthesia facial X-rays or C-T Scans The Client with Eye Trauma Foreign body removal Eye irrigation sterile saline irrigation chemical burn Surgery penetrating wound The Client with Cataracts Cataract a clouding of the lens of the eye interferes with light transmission and the ability to perceive images clearly Significant cause of visional problems in the elderly (50-70%) Senile Cataracts normal aging process The Client with Cataracts Treatment Surgical removal of cataract and lens Implantation of intraocular lens Post-operative Nursing Care assessment eye patch semi-folwer’s Post-operative Nursing Care Avoid coughing, sneezing straining these increase intraocular pressure Assess for post-op pain Assess for surgical complications Approach from unaffected side Teach Home Care meds., symptoms to report, photophobia Glaucoma Characterized by increased intraocular pressure and gradual loss of vision “Silent” thief of vision Narrowing of visual fields 2 Types Open Angle and Closed Angle Glaucoma - inner eye pressure Glaucoma Open Angle common (90%) >35yrs, genetic link, African-American Pathophysiology impaired aqueous outflow increased intraocular pressure usually bilateral Glaucoma Clinical Manifestations none frequent lens changes in glasses impaired night vision halos reduction of vision field, become narrow increased intraocular pressure (tonometry) Glaucoma Treatment miotics - pilocarpine Laser Surgery (trabeculoplasty) cause scar tissue to create tension to stretch opening to drain aqueous fluid Glaucoma Stage 4 Diabetic Retinopathy Leading cause of new blindness between ages of 20-74 84% of diabetics will develop some form depends of length of time you have diabetes Vascular disorder that affects the retina capillaries become sclerotic Diabetic Retinopathy Management Yearly ophthalmologic exams Laser photocoagulation Focus is educational vision changes -blurred black spots (Floaters) flashing lights sudden loss of vision Diabetic Retinopathy - vision Ear Disorders External Otitis swimmers ear pseudomonas, bacteria, fungus or trauma Treatment cleansing antibiotics - local and systemic education Ear Disorders Otitis Media inflammation of middle ear common in infants and young children Red bulging tympanic membrane Treatment antibiotics myringotomy Ear Infection check up Inner Ear Disorders Meniere’s Disease chronic recurrent attack of vertigo with tinnitus progressive hearing loss Treatment antivert The Client with Hearing Loss Affects 24% of older adults Affects 39% of those over age 75 2 Types Conductive disruption transmission of sound obstructions - cerum, scarring, tumors Sensorineural inner ear, auditory nerve or pathways The Client with Hearing Loss Treatment Amplification hearing aids Surgery reconstruct the middle ear - tympanoplasty cochlear implant Nursing Care Sensory/Perceptual Alteration: Auditory, Impaired communication, Social isolation What are your interventions? What kind of pt. teaching will you provide? What’s your post-op nursing care? What is happening here? What about this vision