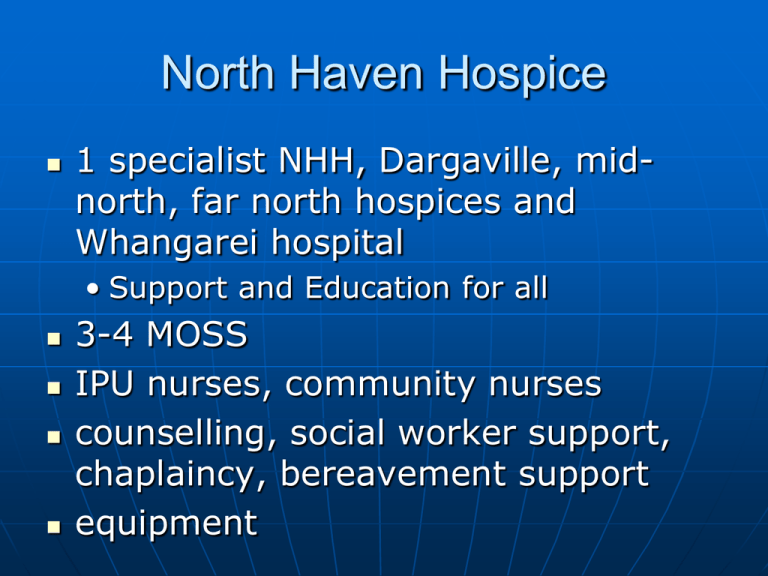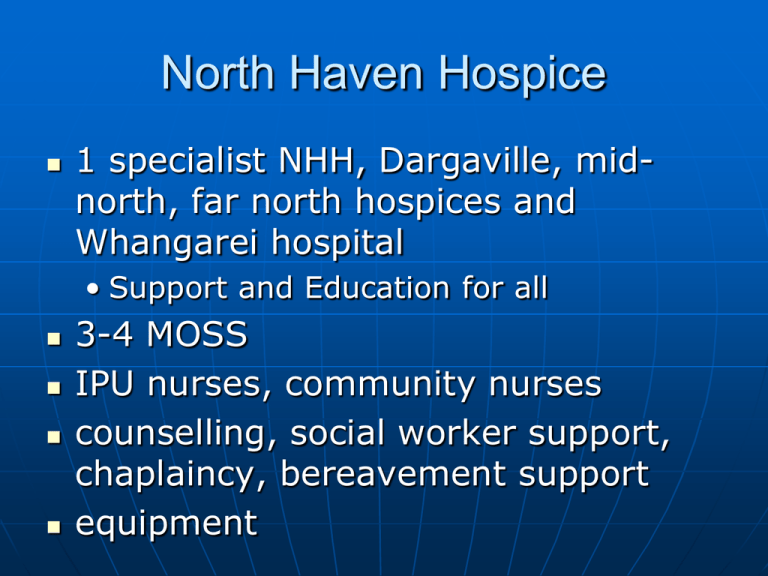
North Haven Hospice
1 specialist NHH, Dargaville, midnorth, far north hospices and
Whangarei hospital
• Support and Education for all
3-4 MOSS
IPU nurses, community nurses
counselling, social worker support,
chaplaincy, bereavement support
equipment
North Haven Hospice
90% of patients want to be at home
Symptom management, Respite,
End-of-Life care,
Alive Discharge rate from IPU?
70% Cancer, 30% non-malignant i.e.
COPD,RF,HF, MND, Paeds
Aiming to help with the more
complex symptom management
patients with a life limiting illness
with a prognosis of less than a year
Malignant Spinal Cord
Compression
By Richard Corkill
Palliative Care Specialist
.
Learning
Objectives 1
1.
2.
3.
Understand the importance of educating
patients with cancer about bone
metastases and metastatic spinal cord
compression (MSCC)
Know where to seek advice when you
suspect a patient may have spinal
metastases or metastatic spinal cord
compression
Recognise those signs and symptoms
which should prompt urgent or
immediate action
Learning Objectives 2
4.
5.
Know which imaging methods to use
to investigate patients
Have a general overview of the
different types of treatment for
MSCC
Malignant Spinal Cord
Compression (Definition)
Spinal cord compression due to
malignancy is defined as a
compression of the thecal sac by
tumour in the epidural space
85%
Malignant Spinal Cord Compression
Importance
Incidence 10% of Cancer Patients
failure to recognises it results in increased patient
suffering
Prompt treatment is essential to maintain
function
Treatment should start within 24-48 hours of
neurological damage when potentially reversible
Delays due to failure to recognise symptoms, lack
of clear referral pathway and no investigation
pathway
Friday referral why?
MSCC Demographics
40-60 years of age
Cervical, Thoracic & Lumbar spinal areas
Multiple levels (20%)
10% further episode
10% MSCC – first presentation of cancer
Cancer sites
• Breast (15-20%), Prostate (15-20%), Lung
(15-20%)
• Myeloma(5-10%), Lymphoma(5-10%),
thyroid, renal, melanoma
Malignant Spinal Cord Compression
Diagnosis
Symptoms
• Back pain (90%), band-like, radicular,
worse at night and on coughing, not
responsive to normal analgesia (3/12)
• Weakness(70%), gone off legs (50%
immobile at diagnosis (70% remain)
• Tingling and Numbness ascends legs,
sensory loss(50%)
• Bladder and bowel problems(40%)
incontinence, frequency, overflow,
palpable bladder.
• Pain may improve with increasing SCC
Signs
Malignant Spinal Cord
Compression
Diagnosis
• Pyramidal Weakness
• Motor level
• Sensory level
• Loss of reflexes
• Reduced anal tone
• Palpable bladder
• Spinal bony tenderness
Spinal Metastases
Severe unremitting or progressive
spinal pain
Spinal pain aggravated by straining
(e.g. cough, sneezing, passing stool)
Nocturnal spinal pain preventing
sleep
Localised spinal tenderness
Metastatic spinal cord
compression
Spinal met symptoms +
• Radicular pain
• Limb weakness
• Difficulty walking
• Sensory loss or bladder or bowel
dysfunction
• Neurological signs of spinal cord or
cauda equina compression
Malignant Spinal Cord
Compression
Investigation
Urgent whole spine MRI (95% accuracy)
• (ask for urgent report or films)
Bloods FBC, U+E’s, Cal, LFT
Immunoglobulin electrophoresis, BJ urine, PSA, LDH, BHCG and AFP
Abdo U/S, Mammogram
CT spine if MRI Contraindicated
Plain X-Rays
Malignant Spinal Cord Compression
Treatment
Depends upon patient wishes, performance
status, length of neurological problem, and
response to steroids
Management multidisciplinary
Strict bed rest, log-rolling, bed pans, eating!
Dexamethasone 16 mg iv stat or po plus cover
with a PPI
Steroids+
•
•
•
•
•
RT
Sx + RT
Sx (decompression+ spinal stabilization)
Chemo (lymphoma and SCLCa)
Symptom Control LCP, Dex, NSAIDs Morphine, Catheter
Treatment - Surgery
Solitary lesion
Rapid onset symptoms
Prognosis of greater 3 months
Short premorbid period
Good bone either side of lesion
Fit enough for surgery
No known histology
Unstable spine or vertebral bone fragment
Previous radiotherapy
Neurological deterioration on radiotherapy
Radio-resistant tumour
MSCC Surgery + RT vs RT
101 pts 7 centres 2005 ant
approach
Criteria
Retained ability to
walk
Median time able to
walk
Median time continent
Immobile – walked
Overall survival
Opioids
Steroids
Sx+RT
84%
vs RT
vs 57%
122
vs 13 days
156
62
126
Less
Less
vs
vs
vs
vs
vs
17 days
19%
100 days
more
more
Malignant Spinal Cord Compression
Prognosis
70-80% of patients who were ambulatory
at start of treatment retain ability
Only 5% of paraplegic patients regain
walking ability with radiotherapy
Hence need for earlier diagnosis
3-6/12 Lung – Breast and Prostate
respectively
If long history (1-2/52) then irreversible
Malignant Spinal Cord
Compression Prognosis
Pre-treatment neurological status
Time to treatment
Vascular event – sudden onset
Vertebral collapse
Performance status and disease
status
Malignant Spinal Cord
Compression Discussion
Need to keep eyes open
Early referral if appropriate
Don’t wait for dexamethasone
response or for Friday
Be aware of those that would benefit
from surgical intervention
Increasing evidence for surgery in
improving function
Malignant Spinal Cord
Compression Future
Known malignancy (esp breast,
prostate and lung) with spine bone
mets and increasing back refer on to
get urgent MRI
NICE Guidance 2008
Need clear pathway for diagnosis and
treatment,
local access to urgent MRI within 24
hours and
informing high risk patients of
symptoms and access to help.
Organisations may wish to consider
their pathways and training for staff
in rapid assessment and handling of
such patients
Cochrane Collaboration 2010
Interventions for the treatment of metastatic
extradural SCC in adults
Stable spines & mobile pts – RT
Mobile pts with poor prognostic
factors for RT - Surgery
Non-ambulant pts with single
compression, <48 hr paraplegia,
radioresistant tumours and a
predicted survival of >3/12 - Surgery
High dose Dex – signif side effects
Going Forward
What clinical practice changes could
you make?
Clinical Audit of mscc patients in
Northland over last 5 years.
Pathway development
Patient information card or letter.