SURGICAL
EMERGENCIES IN
THE NEWBORN
TRACY L. MCTIERNAN, MA, CPNP
DIVISION OF PEDIATRIC SURGERY
NYU LANGONE MEDICAL CENTER
WHAT ARE WE TALKING
ABOUT?
Congenital Diaphragmatic Hernia
Esophageal Atresia
Congenital Intestinal Obstruction
Duodenal Atresia
Ileal and Jejunal Atresia
Meconium Ileus
Malrotation and Volvulus
Hirschsprung’s Disease
Imperforate Anus
Abdominal Wall Defects
Omphalocele
Gastroschisis
Congenital Diaphragmatic Hernia
Incidence
Estimated to be between 1/2000 to 5000 live births
1/3 of infants are stillborn
Males > females in live births
Approximately 80% are on the left side
Occurrence risk in a 1st degree relative ~2%
Etiology
Cause of CDH is unknown
Increasing evidence that it may be related to
exposure to environmental factors
Associated Anomalies
Incidence ranges from 10-50%
Skeletal defects ~32%
Cardiac anomalies ~24%
Tracheobronchial tree ~18%
Pathology
In most cases the defect is established by gestational week 12
Classic left sided CDH features a 2-4 cm posterolateral defect
Herniated contents often include the left lobe of the liver, the
spleen, and almost the entire GI tract
Long term compression of the developing fetal lungs results
in pulmonary maldevelopment and lung hypoplasia
All the major bronchial buds are present in the CDH lung
but the number of bronchial branches is greatly reduced
Alveolar development is also severely affected
Pathology
Pulmonary vascular bed is abnormal, resulting in
increased pulmonary vascular resistance
Increasing hypoxia results in increasing right-to left
shunting leading to severe and progressive
respiratory failure
Diagnosis
Prenatal ultrasound is accurate in 40-90% of cases
Mean gestational age is 24 weeks with some
discovered as early as 11 weeks
Polyhydramnios is present in up to 80% of cases
After birth the respiratory symptoms are determined
by the degree of pulmonary hypoplasia and reactive
pulmonary hypertension
Diagnosis
Most severely affected infants develop respiratory
distress at birth
Majority demonstrate symptoms within the first 24
hours
Infants will have scaphoid abdomen and symmetrically
distended chest
Tracheal deviation away from the defect
Confirmed by plain chest radiograph which
demonstrates loops of bowel in the chest
Management
Key to consider that CDH is a physiologic emergency NOT
a surgical emergency
Early surgery further decreases lung compliance
The post birth transition of vascular and pulmonary function
is prolonged in CDH
In theory, delayed surgery provides additional time for this
transition to occur resulting in a more stable infant
Infants should be intubated and an nasogastric tube passed
Ventilation by mask or Ambu bag is contraindicated
May be managed on a conventional ventilator or a high
frequency ventilator
Management
Key to success is currently thought to be gentle
ventilation with permissive hypercapnea to reduce
barotrauma
Preductal pulseoximetry should be monitored
Metabolic acid base disturbances should be
corrected with fluid management or bicarbonate
administration
ECMO in severe cases - but often NOT necessary
Surgical Management
Timing of surgery is dependent on the infants condition,
ideally anywhere from 5 days to 2 weeks of age
Infant’s ventilator settings are improving and being weaned
Surgical approach is usually through a subcostal incision.
Laparoscopic and thoracoscopic techniques can also be used
Abdominal viscera are gently reduced into the abdominal
cavity
Defect is closed primarily or utilizing a patch
Abdominal wall is closed if possible avoiding increased intraabdominal pressure
Outcomes
Survival rates as high as 80-90% are being reached
with current treatment modalities
High variation in survival rates among institutions
represent different treatment strategies
Associated anomalies such as congenital heart
disease remain a significant risk factor for poor
outcome
Esophageal Atresia and
Tracheoesophageal Fistula
Incidence
EA and TEF are relatively common congenital anomalies
1 in 4500 live births in the US
Male=Female
0.5% - 2% increase risk in newborns with one affected sibling
Risk increases to 20% if more than one sibling is affected
Classification
Esophageal atresia rarely occurs as an isolated
congenital anomaly.
Esophageal atresia alone is due to failure of the
recanalization of the esophagus during the 8th
week of gestation
Gross Classification
85% are type C (Distal TEF)
7% are type A (Pure atresia)
4% are type E ( H-type fistula)
Proximal fistula is the least common
Associated Anomalies
VACTERL: vertebral, anal, cardiac, TE, renal, limb
Congenital heart disease is
associated with higher
mortality
VSD is most common
ASD
Tetralogy of Fallot
PDA
Echocardiogram – important
to determine position of aortic
arch
Associated Anomalies
Vertebral and radial anomalies will be seen on x-ray
Sonogram of the kidneys
Physical Exam of the anus
Clinical Features
Prenatally
• Predictive value of prenatal ultrasound ~20-40%
• Polyhydramnios (2/3 cases)
• Small or absent stomach bubble
Postnatally• Most infants are symptomatic within the first few hours of life
• Excessive salivation
• Regurgitation of first feed
• Cyanosis with/without feeds
• Respiratory distress
• Inability to pass a catheter into the stomach
• Gastric distention (with distal fistula)
Diagnosis
Failure to pass NG tube (not Type E)
CXR- tube coiled in upper esophagus
“Pouchogram” with air
Distal air on AXR confirms the presence of a fistula
H-type fistulas are often diagnosed later
Diagnosis
Confirm with AP chest x-ray that
demonstrates the catheter curled in the
upper esophageal pouch.
•Abdominal XR can help distinguish
esophageal blind pouch (no gastric air) from
distal TEF (gastric air)
Diagnosis
Attempt to pass catheter into stomach. Cannot pass more than 10-15 cm.
Diagnosis
When diagnosis is
uncertain or proximal
TEF is suspected, a
small amount of watersoluble contrast
material can be injected
into the esophageal
pouch under
fluoroscopic guidance
(must remove contrast
material immediately to
avoid regurgitation and
aspiration)
Diagnosis
Proximal Esophageal Atresia
Diagnosis- Type E “H type” TEF
Management
Preoperatively
•
•
•
•
•
•
•
Minimize complications from aspiration
Suction blind pouch continuously with Replogle tube
NPO/TPN
Upright position of child
Early surgery for short gap atresia
Long gap atresia may be delayed up to 6-12 weeks
Long gap atresia should have gastrostomy tube placed for
enteral nutrition
Management
Surgery
•
•
•
Surgical ligation of the fistula
Primary anastomosis of the esophageal segments
Primary repair may not be possible if the distance between
esophageal segments is long. Staged procedures have
been performed that include elongation of the esophagus
with circular myotomy, interposition of the colon, and
gastric transposition
To repair esophageal atresia, a thoracotomy incision is made (A). The proximal and distal
esophageal segments are identified (B). The distal fistula is transected (C) and anastomosed to the
upper esophageal pouch (D). (With H-type fistula a cervical approach can be used in most cases)
Post Operative Management
Management
Post Operative
•
•
•
•
•
•
•
•
Adequate fluid resuscitation
Wean ventilator
No deep tracheal suctioning
Avoid bag/mask ventilation
No pacifiers/sucking
Chest tube remains in place for approximately one week
Replogle tube (10 Fr) remains in place +/- one week
Esophagram 1 week post op
Outcome
PROGNOSIS
85% to 95% survival
Infants with increased risk
of morbidity and mortality
•Low birth weight (>1500)
•Major CHD
•Severe associated
anomalies
•Ventilator dependency
•Long gap atresia
Outcome
Complications
•
•
•
Anastomotic Leak
Esophageal stricture
Recurrent fistula
Other Associated Issues
Tracheomalacia
Disturbed peristalsis and delayed gastric emptying are common
“Seal Bark” cough
Gastroesophageal reflux and aspiration
Congenital Intestinal Obstruction
Intestinal Atresia
Duodenal atresia
Ileal and jejunal atresia
Meconium Ileus
Malrotation and Volvulus
Hirschspung’s Disease
Imperforate Anus
Duodenal Atresia
Incidence
Most common site of neonatal intestinal obstruction
1 in 6,000 to 10,000 live births
75% of stenoses and 40% of atresias are found in Duodenum
Multiple atresias in 15% of cases
50% pts are LBW and premature
Etiology
No specific genetic abnormality
Increase incidence in siblings
Has been shown to occur in several generations of a
family
Association with Trisomy 21
Associated Anomalies
Down Syndrome 28%
Annular pancreas 23%
Congenital heart disease 23%
Malrotation 20%
Esophageal atresia/TEF 9%
Genitourinary 8%
Anorectal 4%
Other bowel atresia 4%
None 45%
Pathology
Type I: The most common type
is formed by a membrane
composed of mucosa and
submucosa and obstructs the
lumen. A variation is the
windsock deformity.
Type II: The atretic ends of the
duodenum are connected by a
fibrous cord.
Type III: Complete separation
of the atretic segments. Most
biliary duct anomalies are
associated with this type.
Diagnosis
Prenatally
•
•
•
Diagnosed in 32-57% of patients
Dilated stomach bubble apparent by 3rd trimester
Polyhydramnios in 32-59% of cases
Postnatally
•
•
•
•
•
Symptoms usually appear within the first 24 hours
Recognition of partial obstruction can be delayed
Repeated bilious emesis is characteristic – 85%
Bilious emesis is a surgical emergency until proven
otherwise
Nonbilious emesis is present when the atresia is above the
level where the bile duct enters the duodenum (papilla of
Vater)
Diagnosis
Radiologic studies
Plain radiograph of the
abdomen will generally
confirm the diagnosis with a
finding of the “double
bubble sign
Upper GI series or barium
enema may be helpful to
differentiate from midgut
volvulus
Management
Replogle tube (10 Fr)
Intravenous fluid resuscitation
Electrolyte correction
PICC line may be considered
If midgut volvulus has been ruled out, surgical correction is
not urgent
Surgery performed is a duodenoduodenostomy or
duodenojejunostomy
Can be performed laparoscopically
Post-operative Management
NPO
Replogle tube (10 Fr)
IV fluids /hyperalimentation
No feeds until return of bowel function
Complications
Early postoperative complications can be related to:
•
•
•
Prematurity
Coexisting congenital anomalies
Parenteral nutrition
Anastomotic obstruction/stenosis
Anastomotic leak
Adhesions
Prolonged feeding intolerance
Duodenal dysmotility
Outcomes
Current survival rates are 90-95%
Higher mortality rates are associated with
prematurity and multiple congenital anomalies
Postoperative complications are reported to be 1418%
Jejunoileal Atresia
Incidence
Has been reported to be as high as 1/3000 live births in the
US
Wide variation in the reported incidence
Males = females
1/3 to ¼ of infants are low birth weight
Higher incidence in African-American infants
Increased risk with maternal use of pseudoephedrine alone
and in combination with acetaminophen
Increased in mothers with migraine headaches receiving
ergotamine tartrate and caffeine
Etiology
Cause is unknown
Most likely associated with a late intrauterine
mesenteric vascular catastrophe
Has been associated with volvulus, intussusception,
internal hernia and constriction of the mesentery in a
tight gastroschisis or omphalocele
Associated anomalies
Gastroschisis/Omphalocele
Ascites
Cystic fibrosis
Malrotation and volvulus
Genitourinary
Pathology
Equally distributed between the jejunum (51%) and
the ileum (49%)
Atresia is usually single (>90%)
Multiple atresias more often involve the proximal
jejunum
Currently 5 classifications
Type I: Mucosal atresia with intact
bowel and mesenetery
TypeII: Blind ends separated by a
fibrous cord
Type III(a): Blind ends separated by
a V-shape mesenteric defect
Type III(b): Apple-peel atresia
Type IV: Multiple atresias (string of
sausages)
Diagnosis
Clinical Signs
•
•
•
•
•
Polyhydramnios - more commonly seen in proximal
atresias
Bilious emesis – SURGICAL EMERGENCY UNTIL
PROVEN OTHERWISE
Abdominal distension
Jaundice
Failure to pass meconium
Radiologic Studies
•
•
Supine and erect abdominal films
Contrast enema or UGI
Management
Replogle tube (10 Fr) to continuous suction
Intravenous fluids
Electrolyte correction
PICC line placement
Operative procedure depends on defect
• May require multiple anastomoses
• May require ostomy
• May require tapering of proximally dilated intestine
Postoperative Management
IV fluid resuscitation
NPO
Replogle (10 Fr) to suction
Clear liquids with return of bowel function
Advance to formula- medium chain triglyceride or casein
hydrolysate formulas should be offered
Malabsorption and diarrhea are common in infants:
•
•
•
•
With short bowel length
In whom the ileocecal valve has been resected
With multiple atresias
Apple peel atresia
Outcomes
Overall survival rates for jejunoileal atresia are
reported to range from 80-90%
Most common cause of early death
•
•
•
Pneumonia
Peritonitis
Sepsis
Postoperative complications
•
•
Intestinal obstruction at the anastomosis
Anastomotic leak
Outcomes
Factors affecting morbidity and mortality
•
•
•
•
Associated anomalies
Short bowel syndrome
Prematurity
Respiratory distress
Meconium Ileus
Incidence
Almost always associated with cystic fibrosis
Reported to be the presenting symptom in 15-20%
of cases
Incidence is reported to be 30-40% in all patients
with cystic fibrosis
Pathology
Simple meconium ileus
• Small intestine mucous glands produce overly
thick secretions
• Meconium formed is abnormally viscid, sticky
and adherent
• Proximal ileum dilated with thick, sticky
meconium
• Distal ileum and colon are collapsed and
obstructed by thickly packed round mucous plugs
– rabbit pellets
Complicated meconium ileus
•
In utero dilated proximal intestine volvulizes
•
Early in gestation may cause one or more atresias
•
Late in gestation infants may present with
perforation -> meconium peritonitis
Associated Anomalies
Cystic fibrosis
Diagnosis
Prenatally
•
•
Prenatal history of cystic fibrosis
Polyhydramnios is reported in ~20% of mothers – more common
finding in complicated meconium ileus
Postnatally
•
•
Intestinal obstruction is evident 24-48 hours after birth
-> abdominal distention
-> bilious emesis
-> failure to pass meconium within 48 hours
Complicated meconium ileus presents at or shortly after birth
-> severe abdominal distension
-> abdominal wall may be red and inflamed
-> extremely ill appearing infant
Radiologic Studies – Simple MI
•Plain radiographs
Varying sized loops
of distended bowel
Absence of air fluid
levels
Soap bubble
appearance particularly
in the right lower
quadrant
•
Contrast Enema
Water soluble contrast
Microcolon
Pellet-like meconium
when contrast is refluxed
into the terminal ileum
Curative in 30% of
patients
Radiologic studies – Complicated MI
•
Plain film
Areas
of calcification (calcified meconium)
Large dense mass with a rim of calcification – cystic
meconium peritonitis
Intraperitoneal calcifications can occur within 4 days of
perforation
•
Contrast enema may not be necessary
Management – Simple MI
Aggressive fluid resuscitation
Naso/orogastric tube to suction
Hyperosmolar contrast enema (Gastrografin)
•
May be curative in 30-60% of patients
Goal of surgery is to completely evacuate the
obstructing plugs and meconium
•
•
•
Enterotomy and irrigation
Intestinal resection and primary anastomosis
Ostomy may be necessary
Management – Complictated MI
•
•
•
•
•
Typically a much sicker infant
Aggressive fluid resuscitation
Electrolyte correction
Findings at surgery dictate the procedure
More likely to have an ostomy
Outcomes
Current 5 year survival is approaching 100%
72% survival at 10 years
Current operative mortality is reported to be 10-20%
Current life expectancy for patients with cystic fibrosis is 35
years
Complications are related to the CF
Most common gastrointestinal problem in patients with CF is
distal intestinal obstruction syndrome
¼ of patients will develop gallstones
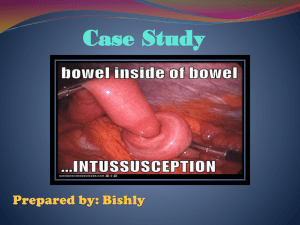
Intussusception occurs in 1%
Rectal prolapse develops in 1/3 to 1/5 of patients
Colonic strictures secondary to high dose oral enzyme
therapy
Intestinal Malrotation and Volvulus
Incidence
Occurs in 1/500 live births
Male to female ration is 2:1 in neonatal presentation
No sexual predilection in patients over 1 year
As many as 40% present within the first week
50% present by 1 month
75% present by 1 year
Etiology
Rotation and fixation of the intestine takes place
during the first 3 months of gestation
As rotation begins, the intestine moves outside the
abdomen
At 10 weeks of gestastional age the intestine returns
to the abdomen
Normal mesenteric attachment extends from the
ligament of Treitz to the cecum
Ascending and descending colon are fixed
retroperitoneally
Etiology
Malrotation is when the normal process of rotation
is arrested or deviated at various stages
Anomalous fixation may also occur
Dense fibrous bands extending from the cecum and
right colon across the duodenum to the
retroperitoneum may form – Ladd’s Bands
Pathology
Midgut may be supported by a narrow pedicle that contains
the entire blood supply
Narrow pedicle predisposes the bowel to a clockwise twisting
from the duodenum to the transverse colon
Distension and peristalsis may initiate torsion of the intestine
on the pedicle - Volvulus
Acute midgut volvulus occurs when the blood supply to the
midgut is disrupted by the torsion
Vascular obstruction and necrosis of the complete midgut
develops rapidly
Ladd’s Bands can cause a mechanical duodenal obstruction
without vascular compromise
Associated Anomalies
Are found in 30 to 60% of patients
Malrotation is almost always associated with
•
•
•
Diaphragmatic hernia
Omphalocele/gastroschisis
Prune belly syndrome
Can be associated with
•
•
•
•
•
•
•
Duodenal atresia
Ileal atresia
Meconium ileus
Congenital heart disease
Imperforate anus
Annular pancreas
Biliary atresia
Diagnosis
Clinical symptoms
•
•
•
•
•
Most frequent symptom is bilious emesis
Pain and irritability in the toddler or older child
Abdomen is soft and non-tender to palpation initially
Becomes distended and tender with strangulation of
bowel
Stool may be bloodstained
Radiologic studies
•
•
Abdominal radiographs may show a dilated duodenem
with a fluid level, however can be read as normal in 20%
of cases
Barium enema is unreliable – position of cecum varies
Diagnosis
•
Radiologic studies
Upper GI series with small bowel follow through is
the most reliable – 96% specificity in one report
Dilated
duodenum with a typical corkscrew appearance
Absence of Ligament of Treitz
Small bowel on right side of abdomen
UGI may be misleading if duodenal obstruction is
complete (also seen with duodenal atresia)
Management
Once the diagnosis is made on a symptomatic child,
the patient should be taken to the operating room
immediately
Ladd’s procedure is performed
•
•
•
•
•
Derotation of the bowel
Division of the Ladd’s bands if present
Widening the small bowel mesentary by lysis of congenital
adhesions
Return the bowel to a position of nonrotation
Appendectomy
Management
If ischemic bowel is present every attempt to
preserve bowel length should be made
Bowel is not surgically fixed into position
Procedure may also be done laparoscopically
Outcomes
Mortality rate with midgut volvulus is at least 15%
Return of bowel function is dependent upon
duration of obstruction and extent of compromise
High incidence of short gut syndrome
Recurrent obstructions are rare
Higher incidence of intussusception post op than
with laparotomies for other reasons ~3%
Hirschsprung’s Disease
Incidence
Ranges from 1/4400 to 1/7000 live births
Male to female ratio 4:1
Long segment disease ratio approaches 1:1 but may
actually favor females
Incidence increases to 6% for siblings of affected
children
Brothers and sons of affected females have the
greatest risk (24% and 29%, respectively)
Etiology
Cause of Hirschsprung’s Disease is unknown
Features of the disease are suggestive of a complex
pattern of inheritance
RET gene mutation was found in~ 35% of sporadic
cases and 49% of familial cases
Associated Anomalies
Trisomy 21 has been reported in 4-16% of cases
Large and small bowel atresia
Anorectal atresia
Ondine’s curse
Pathology
Absence of ganglion cells in the distal intestine is the
hallmark of the disease
Ganglion cells are absent in the submucosal plexus and
intermuscular plexus
Rectosigmoid region in ~80% of cases
Aganglionosis is almost always continuous distally
Long segment disease has been reported 11-26% of
cases
Total colonic 3-12%
Small bowel 0.4-3%
Diagnosis
Clinical findings
•Delayed passage of meconium within the first 48 hours
of life
•95 % of full term infants stool within the first 24 hours
•Remainder will stool by 48 hours
•This history may be absent in 6 to 42% of patients
•Constipation
•Abdominal distension
•Failure to thrive
•Hirschsprung’s Disease should be considered in any
child who has a history of constipation dating back to
the newborn period
Diagnosis
Radiologic studies
•Supine and positional abdominal radiographs distended loops with paucity of air in the rectum
•Contrast Enema with water soluble contrast –
classic finding is a narrow spastic distal segment with
a dilated proximal segment
•Point of caliber change or transition zone is the key
radiographic finding
•Diagnostic accuracy of contrast enema has been
reported to be 76% to 92%
•In any infant with a suspected diagnosis of
Hirschspung’s Disease no rectal stimulation of
any kind should be performed
Diagnosis
•Rectal biopsy is the gold standard
•May be done at the bedside
•Accuracy of suction rectal biopsy has been reported as
high as 99.7%
•Major problem is inadequate specimen
•Full thickness rectal biopsy may be preformed in the
operating room
Management
Primary pull-through procedure
Transanal approach for normal segment disease
Intraoperative biopsies are performed to confirm the
transition zone
Procedure may be performed with laparoscopic
assistance
Older children may require a colostomy first with the
definitive procedure performed several weeks later
Outcome
Early Complications
•Intestinal obstruction 8-13%
•Wound infection 10-15%
•Anorectal stenosis 10-20%
•Anastomotic leak 2%
Late Complications
•Incontinence 3-8% - greatest impact on quality of life
•Constipation reported to range from 6-30%
•Hirschsprung’s enterocolitis
Major cause of morbidity and mortality
Incidence ranges from 20-30%
Cause is unknown but some feel it is related to persistent state of colonic and
small bowel stasis which leads to bacterial overgrowth
Outcome
Hirschsprung’s enterocolitis
Manifested by explosive diarrhea, abdominal
distension and fever
Treatment is with aggressive washout with a rectal
tube, IV antibiotics or oral metronidazole
Quality of life is reasonably good and significantly
better when compared to patients with other anorectal
malformations
Imperforate Anus
Incidence
Average incidence worldwide is believed to be 1 in 5000 live
births
There is a slight male preponderance
Males are twice as likely to have high imperforate anus
Some families have a genetic predisposition
Most common in females – rectovestibular fistula
Most common in males – rectourethral fistula
Imperforate anus without fistula 5% of patients and half of
these patients have Down’s syndrome
Cause is unknown
Associated Anomalies
VACTERL syndrome
50-60% of patients will have one or more anomalies
~ 1/3 will have congenital heart disease
•ASD
•PDA
•Tetrology of Fallot
•VSD
Gastrointestinal
•Tracheoesophageal abnormalities 10%
•Duodenal obstruction 1-2%
Associated Anomalies
Spinal and vertebral
•1/3 to ½ of patients
•Tethered cord is most common
•Spinal lipomas
•Syringomelia
•Myelomemingocele
•Hemivertebrae
•Scoliosis
•Butterfly vertebrae
•Hemisacrum
Associated Anomalies
Genitourinary
•Incidence ranges from 1/3 to 1/2 of patients
•Incidence increases with increasing complexity of malformation
•Vesicoureteral reflux is most common
•Renal agnenesis and dysplasia
•Cryptochidism 3-19%
•Hypospadias 5%
Gynecologic
•Hydrocolpos in the newborn period
•Mullarian anomalies leading to menstrual difficulties
•Uterine abnormalities
•Vaginal anomalies
Pathology
Deformities are divided into high, intermediate and low
Classification depends on how far the rectum is descended
into the pelvis and whether there is a fistula
Patients will have varying degrees of striated muscle
development from normal appearing to no muscle at all
Majority of patients are born without an anal canal and,
consequently, can not discriminate between liquid and gas
after surgical repair
Patients will have a spectrum of rectosigmoid motility
disorders which can lead to constipation issues
Diagnosis
All suspected cases of anorectal malformation require a
thorough perineal examination
Infants should be given sufficient time to pass meconium
Two positional radiographs may be helpful
Invertograms are not useful
Figure 341-3 Imperforate anus in females. A, Vestibular fistula. B, Cloaca. (From Peña
A: Atlas of Surgical Management of Anorectal Malformations. Springer-Verlag, New York, 1989,
pp 50, 60.)
Figure 341-2 Imperforate anus in males. A, Low lesions. B, High lesions. (From
Peña A: Atlas of Surgical Management of Anorectal Malformations. Springer-Verlag, New
York, 1989, pp 7, 26.)
Management
IV fluids
Replogle tube (10 Fr)
Workup for VATER syndrome
•Echocardiogram
•Dedicated spinal films/spinal ultrasound
•Renal ultrasound
Newborn Female
Perineal Inspection
Single perineal
orifice
Perineal fistula
Cloaca
Colostomy
Anoplasty
or
Dilatations
No visible fistula
Vestibular fistula
Primary
repair
Rectum
below
coccyx
High
rectum
Colostomy
Adapted from Pena, A, Levitt, M: Anorectal Malformations. In Grossfeld, J, O’Neill, J, et al (ed)
Pediatric Surgery. 6th Ed.
Newborn Male
Perineal Inspection
Perineal fistula
Rectal gas below coccyx
No associated anomalies
Rectal gas above
coccyx
Associated defects
Abnormal sacrum
Anoplasty
PSARP +/- colostomy
Flat bottom
Colostomy
Adapted from Pena, A, Levitt, M: Anorectal Malformations. In Grossfeld, J, O’Neill, J, et al (ed) Pediatric
Surgery. 6th Ed.
Management
Operative repair
•Anoplasty for perineal fistulas
•Posterior Sagittal Anorectoplasty - PSARP
Electrical stimulation of the perineum to
evaluate sphincter contraction
Midline sagittal incision dividing the sphincter
mechanism into 2 equal parts
Important nerves and vessels do not cross the
midline
•Colostomy with delayed PSARP for high imperforate
anus
Management
Postoperatively
•Oral feeding may begin when the infant is awake enough
•Antibiotics for at least 24 hours
•Rectourethral fistula – foley cathether for 7 days
•Rectal dilation program is begun ~ 2 weeks post op
•Colostomy, if present, is closed when anal caliber is
adequate (~12Fr Hegar dilator in a 1-4 month old)
•Diligent perianal care – protective barrier cream
•Multiple stools initially
Outcomes
Complications
•Wound infections and dehiscence can be catastrophic
•Rectal strictures
•Vaginal strictures
•Rectal mucosal prolapse
•Urologic injuries in males
•Constipation -> megarectosigmoid -> overflow
pseudoincontinence
Studies suggest that 75% of patients achieve good bowel
control and continence
Outcomes
Incontinence is generally divided into 2 groups
1. Constipation – aggressive bowel irrigation is
suggested
2. Increased motility leading to diarrhea – constipating
diet, medication to decrease bowel motility and colonic
irrigation is suggested
May require a bowel management program to achieve
continence
Appendicostomy for retrograde enemas may be helpful
Late toilet training
Abdominal Wall Defects
Omphalocele
Incidence
1-2.5 per 5000 live births
Male preponderance
Second most common abdominal wall defect
Etiology
Cause is unknown
Rare reports occurring in families
No specific gene has been identified
Associated Anomalies
30-70% will have associated anomalies
Congenital heart disease – up to 45%
•VSD
•ASD
•Ectopia Cordis
•Tricuspid Atresia
•Coarctation of the Aorta
•Persistent Pulmonary Hypertension of the Newborn
Chromosomal Abnormalities – up to 40%
•Beckwith-Wiedemann syndrome
•Down’s Syndrome
•Trisomy 13-15
•Trisomy 16-18
Associated Anomalies
Musculoskelatal abnormalities
Neural tube defects
GERD – up to 43% in one study
Cryptorchidism – 33%
Macrosomia
Pathology
Central abdominal wall defect
Usually greater than 4cm in diameter
Covered by a translucent sac unless ruptured inutero
Muscles of the abdominal wall are normal
Sac usually contains the liver, midgut and frequently the
spleen and gonad
All have malrotation
Infants are usually full term
Diagnosis
Usually antenatally by ultrasound
In a European study sensitivity of ultrasound was 75%
Usually detected at 18 weeks +/- 6 weeks
Management
May be delivered vaginally
Placed on mechanical ventilation
Replogle (10 Fr) tube should be placed
Intravenous fluids
Prophylactic antibiotics
Cardiology evaluation and echocardiogram – this should not
delay surgery
Surgery
•Small defects may be closed primarily
•More likely a staged procedure with the placement of a silo
Silo is reduced daily if tolerated at the bedside – ideally
reduced in 7 days
Operating room for final closure
Contents of omphalocele after sac is removed
Management
Post Operative Care
•IV fluids to maintain adequate urine output
•Wean ventilator after final closure
•Replogle tube (10 Fr)
•NPO until return of bowel function
•Return of bowel function may be delayed
•TPN
Outcomes
Post operative complications
•Hypovolemia – very high fluid requirements
•Tight closure -> ventilatory compromise, decreased
venous return and low cardiac output, oliguria
•Metabolic acidosis as a result of kinking of the
hepatic veins from reduction of the liver
Survival rates range from 70-95%
Mortality is often related to associated anomalies
Abdominal Wall Defects
Gastroschisis
Incidence
2-4.9 per 10,000 live births
Male preponderance
Most common abdominal wall defect
Etiology
Cause is unknown, but may be related to fetal distress
Infants are more likely to be premature
Term babies are more likely to be SGA
Associated Anomalies
Much less common than with omphalocele
Intestinal atresia may be seen in 10-15%
GERD ~ 16%
Undescended testicle ~15%
Malrotation is always present
Pathology
Small abdominal wall defect: usually 2-4cm
Occurs adjacent to the umbilicus almost always to the
right
Abdominal muscles are normal
There is no sac
Midgut is herniated through the defect
Matted bowel loops may be present at birth
Exposed bowel may appear normal at birth but quickly
becomes matted with fibrinous exudate such that
individual loops can not be distinguished
Diagnosis
Antenatally by ultrasound
Sensitivity has been reported to be 83%
Detected at 20 weeks +/- 7 weeks
Management
May be delivered vaginally
Cover exposed bowel with warm saline moistened sterile
dressing
Replogle tube (10 Fr)
Support of the premature infant
Monitor for fluid and heat loss
Should be taken to the operating room ASAP
The faster the bowel can be reduced the more likely
primary closure can be achieved
If reduction and primary closure can not be achieved a
silo is placed
Post operatively requires adequate fluid resuscitation
Management
Post operatively
•Wean ventilator after final closure
•Replogle tube (10 Fr)
•NPO until return of bowel function
•May be more prolonged than with omphalocele
•TPN
Outcomes
Post operative complications
•Hypovolemia
•Closure too tight -> ventilatory compromise, decreased venous
return and low cardiac output, oliguria
Survival rate is ~90%
Complications related to prematurity responsible for most morbidity
and mortality
Primary fascial closure has been reported in up to 80%; some
recommend silos in all cases
Median time to feeding ~30 days with a range reported of 5-60 days
Atresias are repaired several weeks after intestinal reduction and
fascial closure
Associated atresia may require more time to feeds
In Summary
BILIOUS EMESIS IS VOLVULUS UNTIL
PROVEN OTHERWISE
History and plain films will guide sequence of
further studies
Remember the associated anomalies
References
Boloker, J., Bateman, D., Wung, J., Stolar, C. Congenital Diaphragmatic Hernia in 120 Infants Treated
Conservatively With Permissive Hypercapnea/Spontaneous Respiration/Elective Repair. Journal
of Pediatric Surgery 2002; 37: 357-366
Dalla Vechia, L.K.,MD; Grosfeld, J.L., MD; West, K,. MD; Rescoria, F., MD; Scherer, L., MD;
Engum, S., MD. Intestinal Atresia and Stenosis. Arch Surg. 1998;133:490-497
Grosfeld, J., MD; O’Neill, J., MD; Fonkalsrud, E. MD; Coran, A., MD (eds). Pediatric Surgery. 6th ed.
Philadelphia, PA: Mosby-Elsevier; 2006.
Lewis, N., MBBS, FRCS; Glick, P., MD, MBA. Duodenal Atresia and Stenosis, Surgical Perspective.
eMedicine from WebMD. 2010. http://emedicine.medscape.com/article/935748
Millar, A., Rode, H., Cywes, S. Malrotation and Volvulus in Infancy and Childhood. Seminars in
Pediatric Surgery 2003;12: 229-236.
Parish, A., MD, Hately, R., MD. Intestinal Malrotation. Emedicine 2010.
http://emedicine.medscape.com/article/930313
Reid, J., MD. Midgut Volvulus. Emedicine 2010. http://emedicine.medscape.com/article/411249overview
Rowe, M., O’Neill, J., Grosfeld, J., Fonkalsrud, E., Coran, A. (eds). Essentials of Pediatric Surgery. St.
Louis, MI: Mosby-Year Book, Inc.; 1995.
University of Michigan Department of Surgery. Meconium Ileus.
http://surgery.med.umich.edu/pediatric/clinical/physician_content/a-m/meconium_ileus.shtml