Breast Lumps
Presented by :Divya Divakaran
Foundation Year 2
Doctor
Contents
•
•
•
•
•
•
•
•
Anatomy of Breast
History taking
Clinical examination
Specific considerations
Triple assessment
Diagnosis
Management
What about men?
Anatomy of Breast
• Introduction to breast :
• Breasts (mammary glands) = modified sweat
glands
• The breast is composed of glandular, ductal,
connective, and adipose tissue. The mammary
glands are modified sweat gland and are
composed of 15-20 lobules, each drained by a
lactiferous duct. Each lactiferous duct
independently drains on the nipple. Areola
surrounds nipple
• In men, little fat is present in the breast, and the
glandular system normally does not develop.
• Lie in superficial fascia anterior to deep fascia of pec.
major
BOUNDARIES :• Bounded by the clavicle superiorly
• Infra-mammary fold inferiorly
• The sternum medially
• Lateral border of the latissimus muscle laterally
Coopers ligament
• The glands are firmly attached to the skin by
connective tissue structures known as
Cooper's ligaments or suspensory ligaments.
Coopers ligament help maintain the structural
integrity. They are named for Astley Cooper,
who first described them in 1840. It is these
ligaments which pull on the skin, creating the
characterisctic dimpling (or peau d'orange)
associated with malignancy
Four Quadrants of the Breast
•
•
•
•
Upper outer (superolateral) quadrant
Upper inner (superomedial) quadrant
Lower outer (inferolateral) quadrant
Lower inner (inferomedial) quadrant
• The French term peau d'orange means skin of
an orange
• Advaned malignancy leads to infiltration and
shortening of Cooper’s ligament
• Leads to irregular dimpling
of skin or retraction of nipple
• Arteries : Predominatly Internal mammary,
lateral thoracic, thoracoacromial, posterior
intercostal
• Veins : Mainly Axillary (subclavian, intercostal,
internal thoracic)
• Lymphatics : Axillary, parasternal, inferior
phrenic nodes
• Nerves : 4th-6th intercostal nerves
• The lymphatic drainage of the breast deserves
special attention, due to its role in the
metastasis of cancer cells. The majority of
lymph (>75%), particularly from the lateral
quadrants, drains to the axillary lymph
nodes. The remainder of lymph drains to
either the parasternal nodes or the opposite
breast
History taking : The Lump
•
•
•
•
•
Onset : when was the lump first noticed
Location : which side - right or left
Single or multiple : how many ?
Unilateral or bilateral
Duration : since when did the pt notice the lump
• Progression : Has it changed in size (ca)
• Is there any pain : type, severity (painless in ca )
• Association with menstrual cycle
• Skin changes, nipple discharge or retraction
• Axillary / supraclavicular swelling
• Previous breast cancer
• H/o trauma, SOB, bone pain, fever or weight
loss
Risk factors
•
•
•
•
•
•
•
•
Female sex, older age
Family history of breast ca
Oral contraceptive pill / HRT
Cycles (early menarche or late menopause)
Pregnancy : lack of child bearing
Lack of breast feeding
Smoking, alcohol intake
High fat diet
• Past medical history
• Surgical history
• Drug history
• Allergies
• Social history : support, activity level, smoking,
alcohol, drugs
Examination
• Specific considerations :
• Chaperone must be present
• Explain to them what the examination will
entail and gain the patients consent
Examination
• Inspection
• Palpation
• Auscultation
Inspection
• Inspect the patient in upright position
• Make a general inspection of both breasts.
Look for any asymmetry, scars, obvious lumps
or nipple abnormalities (e.g. inversion or
discharge)
• You should also comment on any skin changes
(peau d’orange, eczema).
• Ask the patient to place her hands above her
head and repeat the inspection
• Look for any obvious mass
Palpation
• Start on the “normal” side first
• Ask the patient to place her hand behind her
head on the side you are examining
• Systematically examine all areas of the breast
with your hand laid flat on the breast. Start
from outside and work towards the nipple.
Imagine that the breast is a clock face and
examine at each ‘hour’
• LUMP : size, shape, position,consistency,
surface,overlying skin
• Don’t forget that the breast tissue extends
towards the axilla in the ‘axillary tail’
• Ensure you ask the patient if she experiences
any pain during examination
• Examine the other breast in the same manner
• Ask the patient to squeeze both nipples
Lymph node examination
• Examine both axillae for any enlarged lymph
nodes
• Whilst examining the patient’s axilla, you
should fully support the weight of that arm
with yours
• Examine the axilla with your other hand
• Ensuring that you feel all four walls (anterior,
posterior, medial and lateral) as well as feeling
into the apex of the axilla
• Repeat this on the other
side
• Palpate the supraclavicular
fossa on both sides to check
for lymphadenopathy
• Finaly auscultate the chest
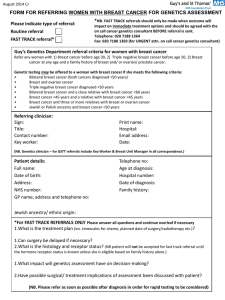
Triple assessment
• Clinical findings
• Radiological findings (Mammography/ USS)
• Biopsy : Histology/cytology
• If there is any abnormality detected in the
examination, or imaging, then biopsies are taken.
This can be in the form of FNAC (Fine Needle
Aspiration Cytology) or a core (Tru-Cut) biopsy.
Breast Cancer
•
Commonest Cancer among women in UK. About
48,000 women get breast cancer in Britain each
year.
• Breast cancer originates from breast tissue, most
commonly from the inner lining of milk ducts
(ductal ca )or the lobules that supply the ducts
with milk (lobular ca)
• Ductal Ca 90%, lobular Ca 10%
• Increase in incidence with age
• Associated with mutations in the breast
cancer susceptibility genes BRCA1 or BRCA2
• Risk factors : Smoking, alcohol, OCPs, HRT
• C/F : painless lump, discharge, skin changes
Stages of breast ca
Common symptoms for breast cancer in both men and women are:
• Swelling or redness in the skin on or around the breast area
• A change in size or shape of one or both of the breast
• A lump or mass in the breast or near the under arm
• Changes in the appearance of nipple
• Discharge of fluid other than milk out of the nipple
Types of breast Cancer
• Breast cancer is often divided into noninvasive and invasive types
• Non-invasive breast cancer is also known as
cancer or carcinoma in situ. This cancer is
found in the ducts of the breast and has
not developed the ability to spread outside
the breast. This form of cancer rarely shows as
a lump in the breast and is usually found on a
mammogram
• Invasive cancer has the ability to spread
outside the breast
• Invasive ductal breast cancer accounts for
about 80% of all cases of breast cancer
Spread
It is possible for breast
cancer to spread to other
parts of the body, usually
through the lymph nodes
or the bloodstream. If this
happens, it is known
metastatic breast cancer.
It metastasis to the lymph
nodes, lungs, liver, bones
etc
• Treatment : Breast cancer is treated using a
combination of surgery (lumpectomy or
mastectomy), chemotherapy and radiotherapy
• There is a good chance of recovery if it is
detected in its early stages.
Fibroadenoma
• Fibroadenoma of the breast is a benign tumor
composed of two elements : epithelium and
stroma
• Fibroadenomas are called breast mouse owing to
their high mobility in the breast
• Painless, firm and mobile
• In young women of child bearing
year
• Hormone-dependent and frequently regress
after menopause
• Investigation : needle biopsy
• Treatment : surgical excison
Benign breast conditions
• Mastalgia : cyclical and non cyclical
• Cyclical mastalgia : painful nodularity
associated with ovulation, hyperplasia
secondary to E2
• Non cyclical mastalgia : trauma, mastitis,
shingles, diurectics
Mastitis
•
Inflammation of breast tissue
• Staph aureus is the main
organism
• 2-10% in lactating women at 2-4 weeks post partum
• Treated with antibiotics
• 90% cured, 10% abscess formation (drainage)
Duct ectasia
• Blockage of the lactiferous duct
The duct widening is commonly believed to be a
result of secretory stasis (stagnant colostrum) or
subject to hormonal interactions or non specific
• pre-menopausal age
• Mimic breast cancer, noncyclic breast pain
• Clinical features : pain, nipple retraction or
nipple discharge
• Self limiting and not indicated for surgery
• Benign lesion
Pappiloma
• Types: central and peripheral
• Central type: single solitary lesion develops
near nipple, seen nearing menopause
Peripheral type : multiple papillomas in the
periphery of breast seen in young women
• C/F: Bloody nipple discharge, masses are too
small to be palpated
• Higher risk of malignant change
• Investigation : galactogram +/- biopsy, not
shown in mammograpghy due to small size
• Excision is sometimes performed (benign)
Men !!!
• Less than 1%
• Peak incidence at 60yrs
• Worst prognosis
Men
• Gynaecomastia : steroids, hormonal therapy,
spiranolactone, CCB, testicular tumours,
pituitary tumours, obesity and in elderly
Summary
• History
• Think risk factors
• Likely diagnosis
• Practise examination
Any Questions ?