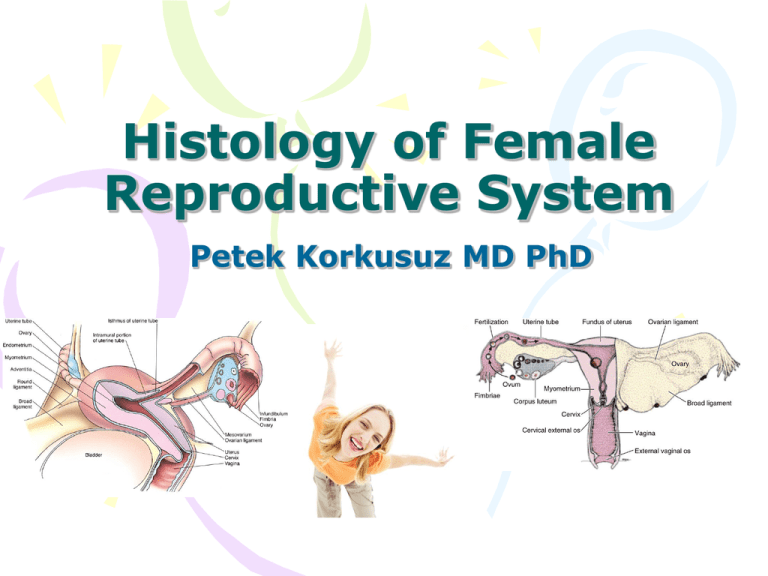
Histology of Female
Reproductive System
Petek Korkusuz MD PhD
Aim
• To learn the histology and the
histophysiology of female genital
system
Learning Goals
• To learn the histology and
of the ovaries
• To learn the histology and
of the oviducts
• To learn the histology and
of the uterus
• To learn the histology and
of the vagina
• To learn the histology and
of the external genitalia
histophysiology
histophysiology
histophysiology
histophysiology
histophysiology
Female genital system
•Internal reproductive
organs
paired ovaries
oviducts,
Uterus
vagina
•External genitalia (vulva)
Mons pubis
Labia majora
Labia minora
Vestibule
clitoris
Ovaries
•Located within the pelvis,
are almond-shaped bodies 3
cm long, 1.5 to 2 cm wide,
and 1 cm thick.
•Surface epithelium covering
the ovaries is called the
germinal
epithelium
(simple
squamous
low
cuboidal
epith),
is
a
modified peritoneum. Directly
beneath this epithelium is the
tunica
albuginea,
the
connective
tissue
capsule
whose collagen fibers are
oriented parallel to the ovary
surface.
•Each ovary is subdivided
into the highly cellular cortex
and a medulla.
Ovaries
• Ovarian cortex is
composed of a
connective tissue
framework, the
stroma, housing
fibroblast-like stromal
cells, ovarian
follicles in various
stages of development.
• Medulla contains
interstitial cells, large
blood vessels, lymph
vessels, and nerve
fibers embedded in a
connective tissue
stroma.
Ovaries
• Before the onset of
puberty, all of the follicles
of the ovarian cortex are
in the primordial follicle
stage.
• The pulsatile release of
GnRH from the
hypothalamus results in a
similar, pulsatile, release
of gonadotropins [FSH],
and [LH]) from the
basophils of the anterior
pituitary that culminates in
the commencement of
follicular development and
the onset of the ovulatory
cycle (follicular-ovulatoryluteal phase).
Ovarian follicles
• The development of the
primary follicles is
independent of FSH;
differentiation and
proliferation of the
follicular cells are triggered
by local factors secreted by
cells of the ovary.
• Secondary and later
follicles are under the
influence of FSH.
• Follicular development
usually culminates in the
release of a single oocyte
(ovulation).
Ovarian follicles
•Are surrounded by stromal
tissue
•Consist of a primary oocyte
and its associated follicular
cells arranged in a single
spherical layer or several
concentric layers around the
primary oocyte.
•There are 4 stages of
follicular development based
on the growth of the follicle
and the development of the
oocyte:
•Primordial follicles
•Unilaminar and
multilaminar primary
follicles
•Secondary (antral) follicles
•Graafian (mature) follicles
Primordial follicles
• The most primitive
follicles,
• Retained in a resting
phase in fetal ovary
• Are abundant before
birth, after which
they become fewer
in number.
• Is composed of a
primary oocyte,
arrested in the
prophase stage of
meiosis I
• is surrounded by a
single layer of
flattened follicular
cells.
Primary follicles
•Primordial follicles develop
into primary follicles
distinguished as a result of
changes in the primary
oocyte, the follicular cells,
and the surrounding stromal
tissue.
•The primary oocyte grows
to 100-150 μm in diameter
with an enlarged nucleus
(sometimes called the
germinal vesicle).
•Follicular cells become
cuboidal in shape. As long as
only a single layer of follicular
cells encircles the oocyte, the
follicle is called a unilaminar
primary follicle.
Multilaminar primary follicles
• Follicular cells proliferate and
stratify, forming several layers of
cells around the primary oocyte,
the
follicle
is
called
a
multilaminar primary follicle,
and the follicular cells are more
commonly
referred
to
as
granulosa cells.
• During this stage, an amorphous
substance (the zona pellucida)
appears, separating the oocyte
from the surrounding follicular
cells.
• Microvilli of the oocyte and
filopodia of the follicular cells
invade the zonula pellucida and
form gap junctions through
which
they
communicate
throughout
follicular
development.
Multilaminar primary
follicles
• Stromal cells form
an inner theca interna,
composed mostly of a richly
vascularized cellular layer
an outer theca externa,
composed mostly of fibrous
connective tissue.
• Theca interna cells produce
androstenedione which
enters the granulosa cells,
where it is converted by the
enzyme aromatase into the
estrogen estradiol.
• Granulosa cells are
separated from the theca
interna by a thickened basal
lamina.
Secondary follicles
•Are similar to primary
follicles except for the
presence of accumulations of
liquor folliculi (containing
hyaluronate, growth factors,
gonadotropins) among the
granulosa cells.
•Continued proliferation of
the granulosa cells of the
secondary follicle depends on
FSH released by basophil
cells of the anterior pituitary.
•As more fluid is produced,
individual droplets of liquor
folliculi coalesce to form a
single, fluid-filled chamber,
the antrum.
Secondary follicles
• Granulosa cells become rearranged so that the primary oocyte is
now surrounded by a small group of granulosa cells that project out
from the wall into the fluid-filled antrum. This structure is called the
cumulus oophorus.
• The loosely arranged low cuboidal granulosa cells immediately
adjacent to the ZP move slightly away from the oocyte, but their
filopodia remain within the ZP, maintaining contact with the primary
oocyte.
• This single layer of granulosa cells that immediately surrounds the
primary oocyte is called the corona radiata.
Preantral follicle formed by an
oocyte and several layers of
granulosa cells. The oocyte is
surrounded by the zona pellucida
Antral follicle
Secondary follicles
• Most of the follicles
that reach this stage
of development
undergo atresia.
• A few secondary
follicles continue to
develop into mature
follicles.
Graafian follicles
•Continued proliferation of the granulosa cells and continued
formation of liquor folliculi result in the formation of a
graafian (mature) follicle
•GF diameter reaches 2.5 cm by the time of ovulation.
•GF may be observed as a transparent bulge on the surface of
the ovary, nearly as large as the ovary itself.
•The follicular cells of the wall of the follicle compose the
membrana granulosa.
Graafian follicles
• Continued formation of
liquor folliculi causes the
cumulus oophorus
composed of the primary
oocyte, the corona radiata,
and associated follicular
cells to become detached
from its base to float freely
within the liquor folliculi.
• By 14th day of the
menstrual cycle, estrogen
produced mostly by the
developing graafian follicle,
but also by secondary
follicles, causes elevation
of blood estrogen to levels
high enough to shutting off
of FSH release and a surge
in LH release.
Graafian follicles-ovulation
• The high blood levels of LH
causes the completion of
the first phase of meiosis I,
resulting in the formation
of the secondary oocyte.
• The secondary oocyte
begins, and is arrested in,
the metaphase stage of
meiosis II and is released
from the graafian follice, a
process known as
ovulation.
• The remnants of the
graafian follicle are
converted into the corpus
hemorrhagicum and then
the corpus luteum.
Corpus luteum. Granulosa lutein cells constituting the majority of the cells, derive from
the granulosa layer. They are larger and stain more lightly than the theca lutein cells
originating from the theca interna.
Ovulation
Corpus luteum
• Formed from the collapsed follicle wall that contains the granulosa
and theca cells
• Granulosa lutein cells form a thick folded layer around the former
follicular cavity (cav)
• Wthin the folds are cells of theca interna (arrows)
• High magn shows the wall of CL mainly composed of granulosa
lutein cells with rounded nucleus.
• The theca lutein cells also have a rounded nucleus, but they are
smaller than granulosa lutein cells.
A small portion of a
corpus luteum.
Most cells present
in the figure are
granulosa lutein
cells
.
Photo micrograph corpus albicans:
large amounts of hyaline material
can be seen among degenerating
cells of the former CL.
Electron micrograph of
theca lutein cells of CL
Ovaries
Scanning electron micrograph of an ovary, showing an oocyte
surrounded by follicular cells. The structure covering the oocyte is
the zona pellucida, which appears as an irregular meshwork.
x2950.
Hypothalamo-hypophiseal-ovarian
axis
• Pituitary hormones control
most ovarian functions.
• FSH stimulates follicular
growth and synthesis of
estrogen by the granulosa
cells.
• LH induces ovulation and
transforms the granulosa
layer and the theca interna
into an actively secreting
gland, the corpus luteum.
• Estrogen and progesterone
produced in the ovary act
on the hypothalamus,
stimulating or inhibiting
the liberation of GnRH.
Uterine (Fallopian) tubes
• Paired tubes extending bilaterally from the uterus toward
the ovaries
• Transport ovum from the ovary to uterus; provide
necessary envitonment for fertilization and initial
development of zygote to the morula stage
• One end of the tube is adjacent to the ovary and opens into
peritoneal cavity; the other end communicates with the
uterine cavity
• Each tube is approx 10-12 cm long and divide into 4
segments:
–
–
–
–
İnfindibulum with fimbria,
ampulla,
isthmus,
uterine (intramural) part
Uterine (Fallopian) tube wall
is composed of three layers:
• Serosa (or peritoneum):
outermost layer composing of
mesothelium and a thin layer
of connective tissue
• Muscularis: thoughout most of
its length is made of an inner,
realitevly thick circular and an
outer thinner longitudinal
layer. The boundary between
these layers is often indistinct
• Mucosa: inner lining
consisting of thin longitudinal
fols that project into the
lumen of the uterine tube.
Folds are most numerous and
complete in ampulla, become
smaller in isthmus. Epith is
simple columnar composing of
cilliated and noncilliated (peg)
cells.
Uterine (Fallopian) tube wall
•
•
•
2 different epith cell types represent different functional states of a single
cell type.
The epith cells undergo cyclic hypertrophy during follicular phase and
atrophy during the luteal phase inresponse to changes in hormonal levels
particularly estrogen.
The uterine tube demonstrates active movements just before ovulation as
the fimbriae become closely apposed to the ovary and localize over the
region of the ovarian surface where rupture will occur.
Uterus
•A single, thick, pear-shaped
structure located in the
midline of the pelvis,
•Receives at its broad, closed
end the terminals of the
paired oviducts.
•It is divided into three
regions:
body,
fundus,
cervix.
•The uterine wall of the body
and the fundus is composed
of
endometrium
myometrium
adventitia or serosa.
Endometrium
• Mucosal lining of the
uterus,
• is composed of a simple
columnar epithelium and a
lamina propria.
• Epithelium is composed of
nonciliated secretory
columnar cells and
ciliated cells,
• Lamina propria houses
simple branched tubular
glands that extend as far
as the myometrium
• Morphological/
physiological alterations in
the endometrium during
the phases of the
menstrual cycle are
controlled by hormones.
Endometrium
• Consists of two layers,
the E. functionalis, a
thick, superficial layer that
is sloughed at
menstruation
the E. basalis, a deep,
narrow layer whose glands
and connective tissue
elements proliferate and
regenerate the functionalis
during each menstrual
cycle.
• E.functionalis is
vascularized by numerous
coiled helical arteries
that supply the glands and
connective tissue.
• The straight arteries are
much shorter and supply
only the E. basalis.
Myometrium-serosa
• Myometrium is
composed of inner
longitudinal, middle
circular, and outer
longitudinal layers of
smooth muscle.
• Much of the anterior
portion of the uterus
is covered by
adventitia ,
• Fundus and posterior
portion of the body
are covered by a
serosa.
Menstruel cycle-menstruation
•Menst begins on the day
bleeding from the uterus
•Occurs when fertilization
does not take place.
•Corpus luteum becomes
nonfunctional about 14 days
after ovulation, thus reducing
the levels of progesterone
and estrogen.
•Although the entire
functionalis layer of the
endometrium is sloughed, it
is not completely released
from the wall immediately;
rather, this process continues
for 3 to 4 days.
Menstruel cycle- proliferative
(follicular) phase
• FP occurs at the same
time as the development
of the ovarian follicles.
• It begins when the
menstrual flow ceases, on
about day 4,
• It continues through day
14 by which time the
functionalis layer of the
endometrium has been
fully restored to its
previous status with a full
complement of epithelium,
glands, stroma, and coiled
arteries.
Menstruel cycle- secretory(luteal)
phase
• SP commences after
ovulation.
• During this phase, the
endometrium continues to
thicken.
• Secretory products first
accumulate in the basal
region of the cytoplasm of
the cells constituting the
endometrial glands,
• Granules move apically,
and are released into the
lumen of the gland.
• This glycogen-rich material
will nourish the conceptus
before the formation of the
placenta.
Menstruel cycle- secretory(luteal)
phase
• SP completes the
menstrual cycle as
the 28th day
approaches
• presaging the
menstrual phase of
a new menstrual
cycle.
Cervix
•
•
•
•
•
•
•
Endometrium of the cervix is
different from the rest of uterus
Mucosa measures 2-3 mm thick;
containd large branched glands,
lacks spiral arteries
Mucosa undergoes little change in
thickness during menstr cycle, is
not sloughed during menstruation.
Cervical glands undergo functional
chnges realted to the transport of
the spermatozoa
Amount and properties of the
mucus secreted by the gland cells
vary during the mens cycle.
At midcycle the amount of mucus
increase 10 fold.
Blockage of opennings of mucosal
glands results in the formation of
nabothian cysts.
• The transformation
zone is the site of
transition between
vaginal startified
squamous epith
and cervical simple
columnar
epithelium.
Vagina
• Is a fibromuscular tube
that joins internal
reproductive organs to the
external environment
• Extends from the cervix to
the vestibule (area
between labia minora)
• In a virgin the opening into
the vagina may be
surrounded by the hymen
• Hymen consists of folds of
mucous membrane
extending into the vaginal
lumen
•
Vagina
Vaginal wall consists of
Inner mucosal layer:
• with numerous transverse
folds or rugae and is lined
by startified squamous
nonkeratinized epithelium.
• CT papillae from the
underlying lamina propria
project into the epithelium,
lacking glands. LP has two
regions: outer cellular
loose CT and deeper dense
CT that may be considered
as submucosa
• Keratohyalin granules may
be present in the epithelial
cells, but keratinization
does not occur
Vaginal epithelium
• Epith surface is lubricated
mainly by mucus produced by
cervical glands and
additionaly by vestibular
glands
• Epithelium undergoes cyclic
changes during menstruel
cycle:
– Epith cells synthesize and
accumulate glycogen as they
migrate toward the surface
during the follicular phase
with estrogen
– Epith cells continously are
desquamated
– Near or during the menstruel
phase the superficial layer
may be shed
Vagina
Intermediate muscular layer
• An outer longitudinal and inneer
circular smooth muscle layer
• The outer sm layer is continuous
with corresponding layer in the
uterus
• Striated muscle fibers of the
bulbospongiosus muscle are
present at the vaginal opening
Outer adventitial layer
• organized into inner dense
connective tissue layer adjacent
to the muscularis
• and an outer loose connective
tissue
External genitalia(vulva)
Mons pubis
Labia majora
Labia minora
Vestibule
Clitoris
Mons pubis and Labia majora
• Is the rounded
prominence
over the pubic
symphisis
• Formed by
subcutaneous
adipose tissue
• Covered with
pubic hair
• 2 folds of skin heavily
endowed with adipose tissue
and a thin layer of smooth
muscle; extending from
mons pubis
• Homologue to scrotum
• Smooth muscle corresponds
to dartos muscle of the
scrotum
• Outer surface covered by
pubic hair;devoid of hair on
the inner surface
• Numerous sweat and
sebaceous glands open on
both surfaces
Labia
majora
Labia minora and Clitoris
• Paired hairless folds of
skin bordering the
vestibule
• Homologous to the skin
of the penis
• Deep epithelial cells have
abundant melanin
pigment
• The core of CT within
each fold is devoid of fat
• CT contains numerous
blood vessels, fine elastic
fibers, large sebaceous
glands
• Errectile structure
homologous to the penis
• Its body is composed of 2
small erectile bodies
(corpora cavernosa)
• Glans clitoris is a small
rounded tubercle of
erectile tissue
• The skin over glans is very
thin forms the prepuce of
the clitoris; contains
numerous sensory nerve
endings
Vestibule
• Lined with stratified squamous epithelium
• Lesser vestibular (Skene) glands:
numerous small mucous glands near the
clitoris and around the external urethral
orrifice
• Greater vestibular (Bartholin’s) glands:
large paired tubuloalveolar glands
homologous to male bulbourethral glands
located at the lateral wall of the vestibule.
Their lubricating mucous secreting ducts
open into vestibule near the vaginal
opening
Cervical smears
• Valuable diagnostic tool for evaluating vaginal
and cervical mucosa
• Superficial epithelial cells are scrapped from the
mucosa, spread on a glass slide, fixed and
stained with Papanicolaou stain ( hematoxylin,
orange G, eosin, azure)
Sensory nerve endings in the
external genitalia
• Meissner’s corpuscles: abundant in the
skin over the mons pubis and labia majora
• Pacinian corpuscles: in the deeper layers
of the CT located in labia majora in
association with the erectile tissue
• Free nerve endings: equally distributed in
the skin of external genitalia
• Questions ????