neuropathology01web
advertisement
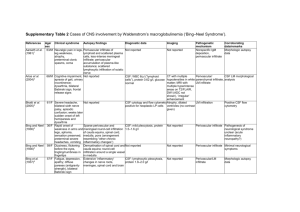
Neuropathology I Main elements of the CNS and their basic pathologic reactions Neurons marked variations in size and shape (Purkinje cell, granular cell) cell body + processes (axon and dendrites) Nissl substance (GER) – proteosynthesis hypoxic/ischemic injury shrinkage of the cell body, ↑eosinophilia („red cell change“), pyknosis of the nucleus axonal injury swelling and rounding of the neuronal body, central chromatolysis (disappearance of the Nissl substance) axonal spheroids (disruption of axonal transport), Waller degeneration distally from the site of injury neuronal atrophy shrinkage of the neuronal body, ↑basophilia, thickened and tortuous („corkscrew“) dendrites neurodegenerative diseases, trans-synaptic degeneration accumulation of abnormal material lysosomal disorders inclusions (viral, neurodegenerative diseases) Astrocytes oval-shaped pale nucleus, numerous processes (invisible in HE) supporting and metabolic function gliosis (hypertrophy and hyperplasia) repair of brain tissue damage gemistocytes (eccentrically expanded pink cytoplasm) Rosenthal fibres thick, elongated, eosinophilic protein aggregates within astrocytic processes chronic gliosis, low-grade gliomas corpora amylacea round, basophilic, PAS+ polyglucosan aggregates within end processes subpial, perivascular Oligodendrocytes small, round-shaped, dark nucleus in HE myelin formation regressive changes in demyelinating disorders and leukodystrophy Ependymal cells cuboidal lining of the ventricular system ependymal granulations ependymal damage local proliferation of subependymal astrocytes Choroid plexus villous structure covered by cuboidal epithelium stroma contains fenestrated capillaries CSF secretion cystic degeneration Microglia small elongated nucleus in HE bone marrow-derived cells gitter cells phagocytosis rod cells neurosyphilis microglial nodules, neuronophagia nodules around dying neurons Cerebral edema, hydrocephalus and intracranial hypertension Cerebral edema accumulation of fluid in excess within cerebral parenchyma Vasogenic edema BBB disrupted (haemorrhagia, trauma, tumour) → ↑permeability of vessels → fluid shifted into intercellular spaces localized or diffuse Cytotoxic edema ischaemia → energy failure → disturbance of ionic gradient on cellular membrane → shift of fluid from extracellular to intracellular space usually diffuse macro diffuse or localized brain swelling, brain softer than normal, flattened gyri, ventricular system compressed micro vacuolation, red cell change, loss of myelin staining, enlargement of extracellular spaces Hydrocephalus accumulation of excessive CSF within the ventricles Normal circulation of CSF produced by choroid plexus → circulation through ventricular system → exit to subarachnoideal space (foramina Luschka and Magendie) → resorbed by arachnoid granulations Causes impaired flow of CSF (subarachnoideal scarring after meningitis or hematoma, block of ventricular system by tumour or blood clot, congenital malformations) ↓resorption of CSF (hypoplasia or damage of arachnoideal granulations) ↑secretion of CSF (choroid plexus tumours) Noncommunicating h. CSF flow block within ventricular system ventricular dilatation proximal to the block Communicating h. reduced CSF resorption dilatation of the entire ventricular system Hydrocephalus e vacuo compensatory enlargement of the ventricled due to brain atrophy macro children before the closure of cranial sutures → enlargement of the head adults → dilatation of the ventricular system, intracranial hypertension Intracranial hypertension brain enclosed within rigid container (skull) ↑volume of intracranial contents (edema, hydrocephalus, tumour, haemorrhage, abscess…) → ↑intracranial pressure → displacement of brain tissue across dural barriers or through openings (herniation), decrease of blood perfusion (global ischaemia) General clinical features of intracranial hypertension headache vomiting papilloedema (ophthalmoscopy) Three patterns of brain herniation transtentorial (uncinate) tonsilar subfalcine (cingulate) Transtentorial (uncinate) herniation medial aspect of temporal lobe compressed against margin of tentorium damage of III. cranial nerve → pupillary dilation and impairment of ocular movements on the side of the lesion compression of posterior cerebral artery → ischemia of occipital lobe (including primary visual cortex) tearing of penetrating vessels → Duret’s hemorage of midbrain and pons Tonsilar herniation cerebelar tonsils into foramen magnum brainstem compresion → damage of respiratory and cardiac centres of medulla Subfalcine (cingulate) herniation cingulate gyrus under the edge of falx compression of anterior cerebral artery → infarction Infections Infections Possible routes of entry hematogeneous spread (most common; endocarditis, bronchiectasia…) local extension from paranasal sinuses, teeth, middle ear direct implantation (trauma, lumbar puncture, ventricular drainage) via peripheral nerves (lyssa, herpetic viruses) Acute pyogenic meningitis leptomeninges + subarachnoid space perivascular spread into underlying brain → meningoencephalitis Etiology neonates: E. coli, Proteus, Streptococci group B toddlers + young children: Haemophilus influenzae adolescents: Neisseria meningitidis (meningococcus) older people: Streptococcus pneumoniae (pneumococcus), Listeria monocytogenes Clinical presentation fever, headache, clouding of consciousness, neck stiffnes lumbar puncture: ↑pressure, ↑↑neutrophils, ↑protein, ↓glucose Morphology leptomeningeal and subarachnoideal purulent exudate over the convexity of brain („pus cap“) Complications pyocephalus vasculitis → infarctions arachnoid adhesions → hydrocephalus Acute viral („aseptic“) meningitis morbilli, ECHO, Coxsackie, EBV, HSV2 clinical course less severe macro mild brain swelling micro mild lymphocytic infiltration of leptomeninges lumbar puncture ↑lymphocytes, mild ↑protein, glucose normal Tuberculous meningitis Mycobacterium tuberculosis hematogeneous spread rare in developed countries children and young adults Clinical presentation headache, malaise, mental confusion, vomiting lumbar puncture: mononuclear cells, protein ↑↑, glucose n. or ↓ Macro base of the brain (basilary m.) gelatinous exudate within subarachnoid space white nodules Micro lymphocytes, plasma cells, macrophages epithelioid granulomas with Langhans’ giant cells caseous necrosis obliterative endarteritis (marked intimal thickening) Complication: arachnoid fibrosis → hydrocephalus Brain abscess acute focal suppurative infection bacterial infection (Staphylococci, Streptococci) hematogeneous spread (endocarditis, bronchiectasia, osteomyelitis) local extension (sinusitis, middle ear - mastoiditis) direct implantation (trauma) Clinical presentation focal neurological deficits signs of Intracranial hypertension Morphology solitary or multiple central liquefactive necrosis + purulent exudate pyogenic membrane (granulation tissue) gliosis, perifocal edema Complications pyocephalus herniation Encephalitis infection of brain parenchyma usually associated with meningitis (meningoencephalitis) Viral encephalitis most common form of encephalitis plenty of viral agents (measles, herpetic viruses, rabies, CMV, HIV…) common features: perivascular mononuclear infiltrates microglial nodules, neuronophagia inclusion bodies Tick encephalitis arboviruses (arthropod borne) several forms (central european, russian, St. Louis fever, …) transmitted by tick bites, disease reservoirs – animals (rodents) perivascular monocelular infiltrates, lymphocytic meningitis severe cases: focal gray and white matter necroses, individual neuronal necrosis followed by neuronophagia and glial nodules → neurologic deficits (paresis) Herpetic encephalitis HSV1 any age, most common in children and young adults frontal and temporal lobes → alterations in mood, memory and behavior foci of necrosis and hemorrhage perivasculat inflammatory infiltrates intranuclear inclusions in both neurons and glial cells HSV2 neonates (infection from mother during delivery) severe disseminated encephalitis Varicella-zoster virus immunosuppressed patients acute encephalitis with intranuclear inclusions Rabies (lyssa) rhabdovirus reservoirs: various animals (dogs, foxes, bats) transmission by bite of a rabid animal (saliva) virus enters CNS by ascending along peripheral nerves → incubation period up to 9 months Clinical presentation nonspecific symptoms (malaise, fever, headache) severe CNS excitability (even slight touch → convulsions) hydrophobia (painful pharyngeal contracture after swallowing or even looking at water) death from respiratory center failure Morphology swelling and hyperemia of brain slight lymphocytic infiltration of leptomeninges Negri bodies – intracytoplasmatic eosinophilic inclusions (hippocampus, Purkinje cells) Poliomyelitis acuta anterior enterovirus eradicated in some countries (Czech rep.), common in developing countries most cases: asymptomatic or mild gastroenteritis small fraction of patients: involvement of motor gray matter damage and loss of motor neurons of spinal cord and brainstem → flaccid paralysis with muscle atrophy most severe cases: paralysis of respiratory muscles → death from asphyxia micro: perivascular lymphocytic infiltrates necrosis of motor neurons → neuronophagia, glial nodules Human immunodeficiency virus 60% of patients with AIDS develop neurologic dysfunctions either direct effect of HIV or secondary involvement by opportunistic infections (toxoplasma, cryptococcus, HSV1, HSV2, VZV, CMV, …) HIV meningoencephalitis cause of AIDS-dementia complex HIV-infected macrophages → cytokines → neuronal damage widely distributed microglial nodules with multinucleated giant cells HIV vacuolar myelopathy HIV polyneuropathy Neurosyphilis Treponema pallidum third stage, 10% of untreated patients Tabes dorsalis degeneration of posterior spinal columns and roots (sensory fibres) → grayish and shrunken unsteady and stamping gait loss of deep tendon reflexes very severe „lightning“ pains in lower limbs severe degeneration of large joints (Charcot joint) Progressive paralysis (general paresis of the insane) deterioration of personality changes in mental functions (bizzare and grandiose delusions) complete dementia brain atrophy disorganisation of the cortex (neuronal degeneration, gliosis, perivascular lymphocytic infiltrates, rod cells) Other encephalitides Lyme disease (borreliosis) Borrelia burgdorferi, transmitted via tick bites see musculoskeletal pathology Fungal encephalitis Candida, Aspergilus, Mucor, Cryptococcus multiple abscesses, granulomas, hemorrhagic infarcts Toxoplasmosis Toxoplasma gondii immunosuppressed individuals, AIDS multiple foci of necrosis surrounded by mixed inflammatory infiltration tachyzoites and cyst filled by bradyzoites Amoebic encephalitis Naegleria: swimming pools, rapidly fatal necrotizing encephalitis Acantamoeba: chronic granulomatous meningoencephalitis Cysticercosis encysted larvae of tapeworm (Taenia solium) intracranial hypertension (mass effect), seizures Slow viral infections very long latent period Subacute sclerosing panencephalitis altered measles virus or aberrant T-cell response (measles or vaccination in clinical history) adolescents progressive loss of intelectual functions, motor abnormalities, dementia, death within 1 year brain atrophy, dilatation of ventricles, firm brain tissue loss of neurons, gliosis, subcortical demyelination intranuclear inclusion bodies within neurons and oligodendroglia perivascular lymphocytic infiltrations Progressive multifocal leucoencephalopathy JC virus (member of papovavirus group) preferential infection of oligodendrocytes → demyelination immunosupressed individuals (lymphoproliferative disorders, AIDS, immunosuppressive therapy) variable progressive neurologic symptoms multiple small gray foci throughout the brain loss of myelin staining, reduced number of axons, lipid-laden macrophages abnormal oligodendrocytes (intranuclear amphophilic inclusions), atypical astrocytes Prion diseases abnormal forms of normal cellular protein (prion protein, PrP; prion = proteinaceous infection) abnormal PrP – „knotted“ conformation ability of abnormal PrP to initiate comparable conformation changes of other PrP molecules → transmissible diseases spontaneous conformation change → sporadic forms mutation of gene encoding PrP → higher rate of conformation changes → familial forms accumulation of abnormal PrP → cell injury (cytoplasmic vacuoles, neuronal cell death Creutzfeldt-Jacob disease (CJD) rare (incidence 1 per million) in 85% sporadic, some cases familial iatrogenic infections (corneal transplants, human growth hormone preparations, brain implantation electrodes) peak incidence in 7. decade of life rapidly progressive dementia, motor dysfunction, fatal within 1 year usually no gross abnormalities or mild atrophy (due to rapid course) spongiform transformation of gray matter multiple small empty vacuoles (intracellular), loss of neurons, reactive gliosis Variant Creutzfeldt-Jacob disease (vCJD) UK 1995 young adults, slower clinical course exposure to bovine spongiform encephalopathy (BSE, „mad cow disease“) similar histologic picture, abundant cortical amyloid plaques Gerstmann-Sträussler-Scheinker syndrome dementia with cerebellar ataxia often familial (autosomal dominant pattern), transmissible several mutations in PrP gene micro similar to CJD + amyloid plaques and amyloidosis of small vessels Kuru endemic to highlands of New Guinea (Fore tribe) ritual canibalism cerebellar ataxia, progressive motor dysfunction, severe tremor (kuru = shivering) death usually within 1 year