Contraception (30-08-11)
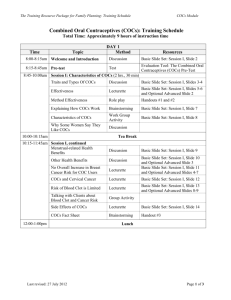
advertisement

Contraception Background Contraception and sexual health Office for National Statistics October 2009 www.statistics.gov.uk ► Surveyed 4366 people (59% response) ► 55% of women aged 16-49 had used family planning services in the last 5 years ► Service use greatest among 25-29y (73%) ► Primary methods: Oral contraception (25%) Male condom (25%) ► Emergency contraception used by 7% of women in last year 42% obtained from a pharmacy (20% in 2001/2) 31% obtained from a GP or practice nurse (43% in 2001/2) Condom failure cited as main reason for using EHC Types and choice of contraception Types of non-surgical contraception BNF 58; September 2009 ► Hormonal contraception Most effective method of fertility control Has major and minor side effects ► Intrauterine devices (IUD) ► Highly effective May produce highly undesirable local effects eg menorrhagia Background risk of PID May be used in women of all ages irrespective of parity Less appropriate for those with increased risk of PID Can be used as emergency contraception Barrier methods Less effective Suitable for well-motivated couples if used with spermicide Accessible Safe Contraceptive choice Contraception and sexual health 2008/9. www.statistics.gov.uk ► ► ► ► ► ► ► ► ► ► ► ► At least one method (76%) OC (25%) Male condom (25%) Male sterilisation (11%) Female sterilisation (6%) IUD (6%) Withdrawal (4%) Injection / implant (4%) Safe period (2%) Hormonal IUS (2%) Emergency contraception (1%) Cap (0%) Use of oral contraception with age Contraception and sexual health 2008/9. www.statistics.gov.uk ► In general, proportion of women using the pill decreases with age ► Use of male condom more prevalent amongst younger couples Types of hormonal contraceptives (1) ► Combined hormonal contraceptives Combined oral contraceptive (COC) ►Usually ethinyloestradiol with a progestogen ►1/2/3/4 generation Transdermal preparation ►Ethinyloestradiol with norelgestromin (an active metabolite of norgestimate) (Evra) Vaginal preparation ►Ethinyloestradiol with etonorgestrel (NuvaRing) Types of hormonal contraceptives (2) 1st generation 2nd generation 3rd generation 4th generation Noerthisterone (Loestrin) Levonorgestrel (Microgynon) Desogestrel (Mercilon) (Marvelon) Drospirenone (Yasmin) Gestodene (Femodette) (Femodene) Dienogest (Qlaira with estradiol valerate Etynodiol diacetate (only in POP) Norgestimate (Cilest) Types of hormonal contraceptives (3) ► Progestogen only contraceptives Progestogen only pill (POP) ► Suitable when COCs unsuitable (eg predisposition to VTE) ► Higher failure rate than COCs ► Norethisterone (Micronor) ► Etynodiol diacetate (Femulen) ► Levonorgestrel (Norgeston) ► Desogestrel (Cerazette) Parenteral progestogen-only contraceptive ► Injection Medroxyprogesterone acetate (Depo-Provera) Norethisterone enantate (Noristerat) ► Implant Etonorgestrel (Implanon) Progestogen-only intra-uterine device (IUD) ► Levonorgestrel (Mirena) Types of hormonal contraceptives (4) ► Emergency hormonal contraceptives Levonorgestrel (Levonelle) Ulipristal acetate (ellaOne) Effectiveness of different forms of contraception How do we measure effectiveness? MeReC Bulletin 2006; 17: 1-9 ► Judged by failure rates: Mode of action of the method Ease of use ► Typical use vs. perfect use ► Pearl Index (PI) No. of unintended pregnancies per 100 women years 1 woman year is 13 menstrual cycles PI=1.0 if 100 women use a contraceptive method for 13 cycles and 1 becomes pregnant Failure rates associated with different methods (1) MeReC Bulletin 2006; 17: 1-9 % of women experiencing unintended pregnancy in 1st year of use Typical use (%) Perfect use (%) No method 85 85 Spermicides 29 15 Withdrawal 27 4 Periodic abstinence Calendar Ovulation method Sympto-thermal Post-ovulation 25 9 3 2 1 Cap plus spermicide Parous women Nulliparous women 32 16 26 9 Sponge Parous women Nulliparous women 32 16 20 9 Diapragm plus spermicide 16 6 Failure rates associated with different methods (2) MeReC Bulletin 2006; 17: 1-9 % of women experiencing unintended pregnancy in 1st year of use Typical use (%) Perfect use (%) Female condom (without spermicide) 21 5 Male condom (without spermicide) 15 2 COC and POP 8 0.3 Evra patch 8 0.3 Depo-Provera injection 3 0.3 Mirena 0.1 0.1 Female sterilisation 0.5 0.5 Male sterilisation 0.15 0.10 Pregnancy rates associated with LARC methods MeReC Bulletin 2006; 17: 1-9 Pregnancy rate (%) Copper IUD <2 over 5 years, for IUDs with at least 380mm copper Progestogen-only intrauterine system <1 over 5 years Progestogen-only injectable contraceptives <0.4 over 2 years (when injections given at the recommended intervals) Progestogen-only subdermal implants <0.1 over 3 years What constitutes good prescribing? Barber N. BMJ 1995; 310: 923-5 EFFECTIVE Benificence SAFE Non-malfeasance COST Justice PATIENT FACTORS Patient autonomy Risks of contraception Increased risk of VTE Current Problems in Pharmacovigilance 1999; 25: 12 Drug Safety Update Vol 1, Issue 9, April 2008 ► All COCs increase the risk of VTE ► The risk associated with COCs containing desogestrel or gestodene (2.5 per 10000 women years) is greater than that associated with other COCs (1.5 per 10000 women years) and with never users (0.5-1.0 per 10000 women years) ► The risk is still low and lower than the risk of VTE in pregnancy (6 per 10000 women years) What about VTE risk with Evra? Drug Safety Update Vol 1, Issue 9, April 2008 ► The VTE risk in users of Evra may be slightly increased compared with that of users of second-generation pills What about VTE risk with Yasmin? Drug Safety Update Vol 1, Issue 9, April 2008 ► The risk is somewhere between pills containing levonorgestrel (second generation) and those containing desogestrel or gestodene (third generation) ► The risk is lower than that of pregnancy Myocardial infarction ► Absolute risk of an MI in young women is very low ► Smoking and OC use increases risk significantly Stroke ► Absolute risk of stroke is very small (1 additional stroke per year per 24000 non-smoking, normotensive women using a low-dose oestrogen) Advice to older women Faculty of Family Planning and Reproductive Healthcare Clinical Effectiveness Unit. Contraception for women aged over 40 years. J Fam Plan Reprod Healthcare 2005; 31: 51-64 ► Women aged over 40 can use combined hormonal contraception unless there are co-existing diseases or risk factors ► The risks of using combined hormonal contraception outweight the benefits for smokers aged ≥35 years ► Women who smoke are best advised to discontinue combined hormonal contraceptives and find another contraceptive method at 35 years Cancer ► OC use does not increase a woman’s overall risk of cancer and may slightly decrease it ► The risk of individual cancers may be increased or decreased depending on duration of use and length of time since last use ► Small, if any, increased risk of breast cancer, but in addition to background risk which increases with age ► Small increased risk of cervical cancer ► Decreased risk of cervical cancer Newer agents Cerazette Which POP? RDTC. Drug Update. Sep 2007 ► Desogestrel 75mcg ► Inhibits ovulation in addition to thickening cervical mucus, with theoretical improved contraceptive efficacy vs. standard POPs ► Desogestrel has a 12h missed pill window ► As desogestrel is more expensive than standard POPs, reserve for women who find the strict regimen of standard POPs difficult to keep to Yasmin MeReC Bulletin Volume 17, Number 2, November 2006 ► Ethinyloestradiol 30mcg / drospirenone 3mg ► An option for those women suitable for a COC. Yasmin has no conclusive advantages over other standard strength COCs Evra MeReC Bulletin Volume 17, Number 2, November 2006 ► Transdermal patch releasing ethinyloestradiol 33.9mcg and norelgestromin 203mcg per 24h ► Option for some women wishing to use a reversible method of contraception and who are experiencing compliance problems with COCs ► Evra vs. oral COCs Better compliance with patch No evidence of improved efficacy, pregnancy rates or safety Similar overall tolerability to COCs VTE risk may be higher with Evra NuvaRing ► Vaginal ring delivering ethinyloestradiol 15mcg and etonogestrel 120mcg per 24h ► One ring inserted vaginally for 3 week duration followed by 7 day ring-free break ► Contraceptive efficacy similar to COCs ► Possibly better cycle control than COCs Qlaira ► Estradiol valerate / dienogest in complex quadriphasic dosage regimen ► First COC containing estradiol ► Continuous 28 day cycle of 26 active tablets and 2 placebo ► Contraceptive effectiveness similar to COCs with comparable side effects and tolerability ► Fewer have withdrawal bleeding Long acting reversible contraception (LARC) (1) NICE Clinical Guideline No 30, October 2005 ► Uptake low 8% of women aged 16-49 in 2003-4 25% pill 23% male condoms ► LARC includes: Copper intrauterine devices (IUD) Progestogen-only intrauterine systems (IUS) eg Mirena Progestogen-only injectable contraceptives eg Dep-provera Progestogen-only subdermal implants eg Implanon Long acting reversible contraception (LARC) (2) NICE Clinical Guideline No 30, October 2005 ► All currently available LARC methods are more cost effective than COCs even at 1 year of use ► IUDs, IUS and implants are more cost effective than the injectable contraceptives ► Increasing the uptake of LARC methods will reduce the numbers of unintended pregnancies Depo-Provera: effect on bones MHRA, 18th November 2004 ► The CSM advised: In adolescents may be used as first line contraception but only after discussion about other methods In women of all ages, careful re-evaluation of the risks and benefits of treatment should be carried out in those who wish to continue use for more than 2 years In women with significant lifestyle and/or medical risk factors for osteoporosis other methods of contraception should be considered Emergency contraception ► Levonelle (levonorgestrel 1.5mg) 1 tablet preferably taken within 12h but no later than 72h ► Non-hormonal IUD ► EllaOne (ulipristal acetate 30mg) 1 tablet ASAP but no later than 120h Case study ► Nicola is a 35y old sales manager. Before the birth of her children she took marvelon for 12 years. She has a complete family and is about to return from maternity leave to work in 2 weeks. She has a BMI of 29kg/m² and smokes. She had a DVT in her second pregnancy in her calf which was treated with heparin ► She would like to recommence the COC. She has gained weight since her children and is concerned the COC will cause more gain. She has heard yasmin does not have this side effect What type of COC is marvelon? ► Third generation COC containing ethinyloestradiol and desogestrel Is there any evidence that Yasmin is less likely to cause weight gain than other COCs? ► For a woman concerned about weight gain with COCs, there is no good evidence upon which to recommend Yasmin instead of other preparations What background questions would you ask in order to identify a preferred method of contraception for Nicola? ► The primary goal is to allow choice of the method with which they feel most comfortable taking into account their lifestyle, preferences and concerns ► Effectiveness compared with alternatives How it works Correct use Health risks and benefits ► ► ► ► ► ► ► ► Medical history Medical risk factors for / personal history of VTE? Family history Breast cancer in 1st degree relatives? Social circumstances Will she travel long distances by car? Personal preferences As family is complete would she prefer the convenience and effectiveness of long-acting method? Exclude pregnancy Menstrual and sexual history ► During further discussion, her job involves long car journeys of up to 4-5 hours. She has completed her family and is seeking a highly reliable form of contraception How would this new information influence the advice which you might offer to her? The “pill scare” – Current Problems in Pharmacovigilance 1999; 25: 12 Risk of VTE associated with COC use and non-use Circumstance Risk of VTE per 100000 women Healthy, non-pregnant women (not taking any oral contraceptive) 5 cases per year Women taking COCs containing levonorgestrel 15 cases per year of use Women taking COCs containing desogestrel or gestodene 25 cases per year of use ► Risk of VTE in pregnancy 60 per 100000 ► Risk of dying on the road 6 in 100000 ► A family history of VTE and continuous travel of more than 3 hours are both risk factors for VTE ► Obesity is also a risk factor ► Her risk of VTE is increased by her personal history of VTE, she travels long distances, and she is overweight ► There is also a small additional risk of MI and stroke from her age, smoking and body weight ► She requests more information on LARC What information and advice would you offer her? ► Contraceptive efficacy ► Duration of use ► Risks and possible side effects ► Non-contraceptive benefits ► Procedure for initiation and removal / discontinuation ► When to seek help when using the method End